Abstract
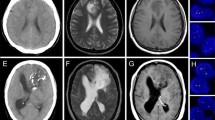
Calcification is a rare phenomenon in high grade glioma (HGG). CT scans are sensitive to mineralization but used infrequently for tumor assessment in the MRI era. The presence of calcification can be overlooked on routine MRI. Calcification may reflect chronicity and natural changes in the tumor or its milieu over time and may be accelerated by certain treatments. Calcification may have clinical significance which could signal potential risk for stroke or hemorrhage related to particular therapies; or it may be a positive prognostic factor for treatment response. The true incidence and relevance of calcification in HGG and relation to therapy is unclear. During treatment of HGG patients with bevacizumab (BVZ) we observed significant tumor calcification on brain CT. We performed a retrospective review of HGG patients treated with BVZ to quantitate the incidence of calcification in this group compared to those treated with cytotoxic therapy alone. Sixty-two patients with progressive HGG were treated with BVZ and a cytotoxic agent. Among 19 patients treated for 6+ months, 12 had a CT scan performed. We observed an unexpected phenomenon of calcification in the CT scans of several patients. We were also able to comparatively quantitate the incidence of calcification in a control group of primary glioblastoma (GB) patients not exposed to BVZ therapy. The incidence of calcification in the general GB population is increased with longer survival. The phenomenon is increased with anti-angiogenic therapy for brain tumors. Calcification may have significance as a predictor for treatment response.


Similar content being viewed by others
References
Deistung A, Schweser F, Wiestler B et al (2013) Quantitative susceptibility mapping differentiates between blood depositions and calcifications in patients with glioblastoma. PLoS One 8(3):e57924
Seet RC, Rabinstein AA, Lindell PE, Uhm JH, Wijdicks EF (2011) Cerebrovascular events after bevacizumab treatment: an early and severe complication. Neurocrit Care 15(3):421–427
Fraum TJ, Kreisl TN, Sul J, Fine HA, Iwamoto FM (2011) Ischemic stroke and intracranial hemorrhage in glioma patients on antiangiogenic therapy. J Neurooncol 105(2):281–289
Letarte N, Bressler LR, Villano JL (2013) Bevacizumab and central nervous system (CNS) hemorrhage. Cancer Chemother Pharmacol 71(6):1561–1565
Stark-Vance V (2005) Bevacizumab and CPT-11 in the treatment of relapsed malignant glioma. In: Proceedings of the World Federation of Neuro-Oncology Meeting, Edinburgh, UK
Friedman HS, Prados MD, Wen PY et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740
Wong ET, Hess KR, Gleason MJ et al (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17(8):2572–2578
Vredenburgh JJ, Desjardins A, Herndon JE II et al (2007) Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol 25(30):4722–4729
Bokstein F, Shpigel S, Blumenthal DT (2008) Treatment with bevacizumab and irinotecan for recurrent high-grade glial tumors. Cancer 112(10):2267–2273
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280
Lobel U, Sedlacik J, Sabin ND et al (2010) Three-dimensional susceptibility-weighted imaging and two-dimensional T2*-weighted gradient-echo imaging of intratumoral hemorrhages in pediatric diffuse intrinsic pontine glioma. Neuroradiology 52(12):1167–1177
Huppmann MV, Johnson WB, Javitt MC (2010) Radiation risks from exposure to chest computed tomography. Semin Ultrasound CT MR 31(1):14–28
Lee YY, Van Tassel P (1989) Intracranial oligodendrogliomas: imaging findings in 35 untreated cases. AJR Am J Roentgenol 152(2):361–369
Nakamura M, Roser F, Michel J, Jacobs C, Samii M (2003) The natural history of incidental meningiomas. Neurosurgery 53(1):62–70 (Discussion 70-61)
Sachs C, Sjoberg HE, Ericson K (1982) Basal ganglia calcifications on CT: relation to hypoparathyroidism. Neurology 32(7):779–782
Lemos RR, Ferreira JB, Keasey MP, Oliveira JR (2013) An update on primary familial brain calcification. Int Rev Neurobiol 110:349–371
Yamada M, Asano T, Okamoto K et al (2013) High frequency of calcification in basal ganglia on brain computed tomography images in Japanese older adults. Geriatr Gerontol Int 13(3):706–710
Mork SJ, Lindegaard KF, Halvorsen TB et al (1985) Oligodendroglioma: incidence and biological behavior in a defined population. J Neurosurg 63(6):881–889
Lote K, Egeland T, Hager B, Skullerud K, Hirschberg H (1998) Prognostic significance of CT contrast enhancement within histological subgroups of intracranial glioma. J Neurooncol 40(2):161–170
Tanaka Y, Takeuchi K, Maeda T (1975) Calcification in gliomas: first report with special reference to roentgenological calcification (author’s transl). No Shinkei Geka 3(3):219–225
Takeuchi K, Hoshino K (1977) Statistical analysis of factors affecting survival after glioblastoma multiforme. Acta Neurochir (Wien) 37(1–2):57–73
Bahr O, Hattingen E, Rieger J, Steinbach JP (2011) Bevacizumab-induced tumor calcifications as a surrogate marker of outcome in patients with glioblastoma. Neuro Oncol 13(9):1020–1029
Suzuki S, Nishio S, Takata K, Morioka T, Fukui M (2000) Radiation-induced brain calcification: paradoxical high signal intensity in T1-weighted MR images. Acta Neurochir (Wien) 142(7):801–804
Weiseenthal L, Williamson S, Brunschwiler C, Rueff-Weisenthal C (2012) Bevacizumab-induced tumor calcifications can be elicited in glioblastoma microspheroid culture and represent massive calcium accumulation death (MCAD) of tumor endothelial cells. 14th international symposium on anti-angiogenic therapy: recent advances and future directions in basic and clinical cancer research, LaJolla, CA, USA
Masellis AM, Sielaff TD, Bender GP (2009) Successful treatment of metastatic pancreatic adenocarcinoma with combination chemotherapy regimens. Int J Clin Oncol 14(5):478–481
Conflict of interest
We declare that there is no conflict of interest for any of the authors.
Funding
We declare that there was no outside funding that supported this research.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Blumenthal, D.T., Aisenstein, O., Ben-Horin, I. et al. Calcification in high grade gliomas treated with bevacizumab. J Neurooncol 123, 283–288 (2015). https://doi.org/10.1007/s11060-015-1796-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1796-z