Abstract
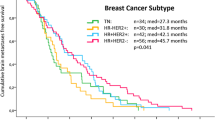
Our group has previously published the Diagnosis-Specific Graded Prognostic Assessment (GPA) showing the prognostic factors associated with survival in patients with brain metastases (BM). The purpose of this study is to investigate the relationship of breast cancer subtype to the time interval from primary diagnosis (PD) to development of BM (TPDBM), number of BM at initial BM presentation and survival. We analyzed our previously described multi-institutional retrospective database of 865 breast cancer patients treated for newly-diagnosed BM from 1993 to 2010. Several factors found to be associated with survival were incorporated into the Breast-GPA, including tumor subtype. The GPA database was further analyzed to determine if the subtype correlated with the TPDBM, number of BM, and survival from PD. After exclusions for incomplete data, 383 patients remained eligible for analysis. The subtypes were approximated as follows: Luminal B: triple positive; HER2: HER2 positive/ER/PR negative; Luminal A; ER/PR positive/HER2 negative; Basal: triple negative. Patients with Basal (90), HER2 (119), Luminal B (98) and Luminal A (76) tumor subtypes had a median TPDBM of 27.5, 35.8, 47.4 and 54.4 months (p < 0.01), median survival from PD of 39.6, 66.4, 90.3 and 72.7 months (p < 0.01) and median survival from BM of 7.3, 17.9, 22.9 and 10.0 months (p < 0.01), respectively. Tumor subtype is an important prognostic factor for survival in patients with breast cancer and BM. Although TPDBM is not an independent prognostic factor for survival (and thus not part of the Breast-GPA), the TPDBM does correlate with tumor subtype but does not correlate with the number of BM. Patients with Basal and HER2 tumor subtypes have short TPDBM. Prospective studies are needed to determine if screening brain MRIs are indicated in patients with Basal or HER2 subtypes.
Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics 2012. CA Cancer J Clin 62:10–29
Lin NU, Bellon JR, Winer EP (2004) CNS metastases in breast cancer. J Clin Oncol 22:3608–3617
Gaspar L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Sperduto PW, Kased N, Roberge D et al (2012) Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30:419–425
Sperduto PW, Kased N, Roberge D et al (2012) Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 82:2111–2117
Gabos Z, Sinha R, Hanson J et al (2006) Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol 24:5658–5663
Carey LA, Perou CM (2009) Gene arrays, prognosis and therapeutic interventions. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the Breast. 4th edn. Philadelphia, PA, Wolters Kluwer/Lippincott Williams & Wilkins, p. 458–472
Perou CM, Sorlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Nguyen PL, Taghian AG, Katz MS et al (2008) Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER2 is associated with local and distant recurrence after breast conserving therapy. J Clin Oncol 26:2373–2378
Andrews DW, Scott CB, Sperduto PW et al (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Sperduto PW, Wang M, Robins HI, et al. A phase III trial of whole brain radiation therapy (WBRT) and stereotactic radiosurgery (SRS) alone versus WBRT & SRS with temozolamide or erlotinib for non-small cell lung cancer and 1-3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys. Available at http://dx.doi/10.1016/j.ijrobp.2012.11.042
Le Scodan R, Jouanneau L, Massard C (2011) Brain metastases from breast cancer: prognostic significance of HER-2 overexpression, effect of trastuzumab and cause of death. BMC Cancer 11:395
Sperduto PW, Chao ST, Sneed PK et al (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: A multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 77:655–661
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514
Vas-Luis I, Ottesen RA, Hughes ME, et al (2012) Impact of hormone receptor status on patterns of recurrence and clinical outcomes among patients with human epdermal growth factor-2-positive breast cancer in the National Comprehensive Cancer Network: a prospective cohort study. Breast Cancer Res 14:R129
Acknowledgments
Dr. Mehta has served as a consultant to Abbott, Bristol-Meyers-Squibb, Elekta, Genentech, Merck, Novartis, Novocure, Tomotherapy and Viewray; he serves on the Board of Directors of Pharmacyclics, He holds stock options in Pharmacyclics and Accuray. Dr. Lin has served as a consultant to Novartis (<$10 K) and GlaxoSmithKline (<$10 K). Grant Support This research was supported in part by Grant W81XWH-062-0033 from the U.S. Department of Defense Breast Cancer Research Program, to RJW, and by NIH Grant P30- CA77598 utilizing the services of the Biostatistics Core, Masonic Cancer Center, University of Minnesota shared resource.
Conflict of interest
The authors have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sperduto, P.W., Kased, N., Roberge, D. et al. The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer. J Neurooncol 112, 467–472 (2013). https://doi.org/10.1007/s11060-013-1083-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1083-9