Abstract
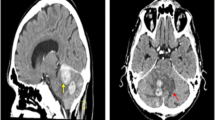
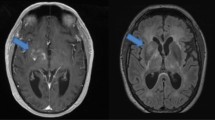
To increase awareness about lymphomatosis cerebri by describing a patient with a unique presentation Case report a 58 year old woman presented with progressive lower extremity weakness, postural hypotension, and 90 pound weight loss over 3 months a brain magnetic resonance image revealed multiple non-enhancing foci of T2 hyperintensity in the periventricular white matter despite treatment with corticosteroids, she expired autopsy demonstrated normal gross appearance of the brain and spinal cord microscopic inspection revealed diffuse infiltration of the central nervous system (CNS) parenchyma and white matter by large atypical B cells, consistent with a diagnosis of lymphomatosis cerebri lymphomatosis cerebri is a primary CNS lymphoma variant that is poorly recognized and often misdiagnosed it commonly presents as a rapidly progressive dementia, although patients may present with neurologic dysfunction without dementia diagnosis requires a pathological examination treatment with intravenous high–dose methotrexate based chemotherapy should be considered in appropriate patients.




Similar content being viewed by others
References
DeAngelis LM (2001) Brain tumors. N Engl J Med 344:114–123
Kanai R, Shibuya M, Hata T, Hori M, Hirabayashi K, Terada T, Fujii K (2008) A case of ‘lymphomatosis cerebri’ diagnosed in an early phase and treated by whole brain radiation: case report and literature review. J Neurooncol 86:83–88
Bakshi R, Mazziotta JC, Mischel PS, Jahan R, Seligson DB, Vinters HV (1999) Lymphomatosis cerebri presenting as a rapidly progressive dementia: clinical, neuroimaging and pathologic findings. Dement Geriatr Cogn Disord 10:152–157
Carlson BA (1996) Rapidly progressive dementia caused by nonenhancing primary lymphoma of the central nervous system. AJNR 17:1695–1697
de Toledo M, Lopez-Valdes E, Ferreiro M, Cervera JL, Ramos A, Cabello A, Hernandez-Lain A, Montes-Montes S, Lagares A, Alvarez-Linera Prado J (2008) Lymphomatosis cerebri as the cause of leukoencephalopathy. Revista de Neurologia 46:667–670
Furusawa T, Okamoto K, Ito J, Kojima N, Oyanagi K, Tokiguchi S, Sakai K (1998) Primary central nervous system lymphoma presenting as diffuse cerebral infiltration. Radiat Med 16:137–140
Kitai R, Hashimoto N, Yamate K, Ikawa M, Yoneda M, Nakajima T, Arishima H, Takeuchi H, Sato K, Kikuta K (2012) Lymphomatosis cerebri: clinical characteristics, neuroimaging, and pathological findings. Brain Tumor Pathol 29:47–53
Leschziner G, Rudge P, Lucas S, Andrews T (2011) Lymphomatosis cerebri presenting as a rapidly progressive dementia with a high methylmalonic acid. J Neurol 258:1489–1493
Lewerenz J, Ding X, Matschke J, Schnabel C, Emami P, von Borczyskowski D, Buchert R, Krieger T, de Wit M, Munchau A (2007) Dementia and leukoencephalopathy due to lymphomatosis cerebri. J Neurol Neurosurg Psychiatr 78:777–778
Pandit L, Chickabasaviah Y, Raghothaman A, Mustafa S, Vasudevan A (2010) Lymphomatosis cerebri—a rare cause of leukoencephalopathy. J Neurol Sci 293:122–124
Raz E, Tinelli E, Antonelli M, Canevelli M, Fiorelli M, Bozzao L, Di Piero V, Caramia F (2011) MRI findings in lymphomatosis cerebri: description of a case and revision of the literature. J Neuroimaging 21:e183–e186
Rollins KE, Kleinschmidt-DeMasters BK, Corboy JR, Damek DM, Filley CM (2005) Lymphomatosis cerebri as a cause of white matter dementia. Hum Pathol 36:282–290
Vital A, Sibon I (2007) A 64-year-old woman with progressive dementia and leukoencephalopathy. Brain Pathol (Zurich, Switzerland) 17: 117–118, 121
Weaver JD, Vinters HV, Koretz B, Xiong Z, Mischel P, Kado D (2007) Lymphomatosis cerebri presenting as rapidly progressive dementia. Neurologist 13:150–153
Poussaint TY, Barnes PD, Nichols K, Anthony DC, Cohen L, Tarbell NJ, Goumnerova L (1997) Diencephalic syndrome: clinical features and imaging findings. AJNR 18:1499–1505
Ashworth B (1982) Cerebral histiocytic lymphoma presenting with loss of weight. Neurology 32:894–896
Miyoshi Y, Yunoki M, Yano A, Nishimoto K (2003) Diencephalic syndrome of emaciation in an adult associated with a third ventricle intrinsic craniopharyngioma: case report. Neurosurgery 52: 224–227; discussion 227
Fleischman A, Brue C, Poussaint TY, Kieran M, Pomeroy SL, Goumnerova L, Scott RM, Cohen LE (2005) Diencephalic syndrome: a cause of failure to thrive and a model of partial growth hormone resistance. Pediatrics 115:e742–e748
Hsu CY, Hogan EL, Wingfield W Jr, Webb JG, Perot PL Jr, Privitera PJ, Talbert OR, Balentine JD (1984) Orthostatic hypotension with brainstem tumors. Neurology 34:1137–1143
Telerman-Toppet N, Vanderhaeghen JJ, Warszawski M (1982) Orthostatic hypotension with lower brain stem glioma. J Neurol Neurosurg Psychiatr 45:1147–1150
Thomas JE, Schirger A, Love JG, Hoffman DL (1961) Orthostatic hypotension as the presenting sign in craniopharyngioma. Neurology 11:418–423
Abrey LE, Yahalom J, DeAngelis LM (2000) Treatment for primary CNS lymphoma: the next step. J Clin Oncol 18:3144–3150
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keswani, A., Bigio, E. & Grimm, S. Lymphomatosis cerebri presenting with orthostatic hypotension, anorexia, and paraparesis. J Neurooncol 109, 581–586 (2012). https://doi.org/10.1007/s11060-012-0931-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0931-3