Abstract
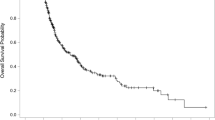
We retrospectively evaluated the relationship between the response of lung lesions and distant progression-free survival (DPFS) after radiosurgery in patients with brain metastases. A total of 47 consecutive patients were treated with radiosurgery for brain metastases. Distant progression was defined as a new enhancing intracranial tumor or leptomeningeal enhancement noted on follow-up magnetic resonance imaging. Progression of lung lesions was defined as follows: (1) a 20% increase in the summed diameter of the target lesions; (2) an absolute increase of 5 mm when the summed diameter was very small; or (3) detection of new lesions in the lung. Distant progression after radiosurgery was observed for twenty-one (44.7%) patients; we observed development of new distant metastases in nine patients, development of leptomeningeal seeding in eight patients, and combined failure of distant progression and local control failure in four patients. Forty-two (89.4%) patients had lung lesions at the time of radiosurgery, and progression of their lung lesions during the post-radiosurgery follow-up period was observed for 18 (38.3%) of these. The median DPFS was 7.00 months (95% CI, 6.153–7.847). Actuarial DPFS 3, 6, and 12 months after radiosurgery was 81.5, 61.3, and 36.7%, respectively. In multivariate analysis, only the criterion progression of lung lesions reached statistical and independent significance (P = 0.021, OR = 3.372, 95% CI, 1.200–9.480). The response of lung lesions after radiosurgery is likely to be a good predictor of DPFS after radiosurgery in patients with brain metastases.



Similar content being viewed by others
References
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Aoyama H, Tago M, Kato N, Toyoda T, Kenjyo M, Hirota S, Shioura H, Inomata T, Kunieda E, Hayakawa K, Nakagawa K, Kobashi G, Shirato H (2007) Neurocognitive function of patients with brain metastasis who received either whole-brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 68:1388–1395
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Karlsson B, Hanssens P, Wolff R, Soderman M, Lindquist C, Beute G (2009) Thirty years’ experience with Gamma Knife surgery for metastases to the brain. J Neurosurg 111:449–457
Sheehan JP, Yen CP, Nguyen J, Rainey JA, Dassoulas K, Schlesinger DJ (2011) Timing and risk factors for new brain metastasis formation in patients initially treated only with Gamma Knife surgery. J Neurosurg 114:763–768
Varlotto JM, Flickinger JC, Niranjan A, Bhatnagar AK, Kondziolka D, Lunsford LD (2003) Analysis of tumor control and toxicity in patients who have survived at least one year after radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 57:452–464
Sawrie SM, Guthrie BL, Spencer SA, Nordal RA, Meredith RF, Markert JM, Cloud GA, Fiveash JB (2008) Predictors of distant brain recurrence for patients with newly diagnosed brain metastases treated with stereotactic radiosurgery alone. Int J Radiat Oncol Biol Phys 70:181–186
Lassman AB, DeAngelis LM (2003) Brain metastases. Neurol Clin 21:1–23
Chason JL, Walker FB, Landers JW (1963) Metastatic carcinoma in the central nervous system and dorsal root ganglia. A prospective autopsy study. Cancer 16:781–787
Zimm S, Wampler GL, Stablein D, Hazra T, Young HF (1981) Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer 48:384–394
Tom MI (1946) Metastatic tumours of the brain. Can Med Assoc J 54:265–268
Globus JH, Meltzer T (1942) Metastatic tumors of the brain. Arch Neurol Psychiatry 482:163–226
Han JH, Kim DG, Chung HT, Park CK, Paek SH, Kim CY, Jung HW (2008) Gamma Knife radiosurgery for skull base meningiomas: long-term radiologic and clinical outcome. Int J Radiat Oncol Biol Phys 72:1324–1332
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90–05. Int J Radiat Oncol Biol Phys 47:291–298
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
King AB, Ford FR (1942) A clinical and anatomical study of neurological conditions resulting from metastases in the central nervous system due to carcinoma of the lung: review of 100 cases. Bull Johns Hopkins Hosp 70:124–156
Jawahar A, Matthew RE, Minagar A, Shukla D, Zhang JH, Willis BK, Ampil F, Nanda A (2004) Gamma knife surgery in the management of brain metastases from lung carcinoma: a retrospective analysis of survival, local tumor control, and freedom from new brain metastasis. J Neurosurg 100:842–847
Yu C, Chen JC, Apuzzo ML, O’Day S, Giannotta SL, Weber JS, Petrovich Z (2002) Metastatic melanoma to the brain: prognostic factors after gamma knife radiosurgery. Int J Radiat Oncol Biol Phys 52:1277–1287
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1, 960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, Postmus P, Collette L, Musat E, Senan S (2007) Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357:664–672
Acknowledgments
This study was supported by Grant no. 11-2008-027 from the SNUBH Research fund. We would like to express our appreciation to Ji Young Park for her sincere help with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, J.H., Kim, D.G., Oh, C.W. et al. Progression of the lung cancer primary correlates with the identification of new brain metastases after initial radiosurgery. J Neurooncol 106, 161–167 (2012). https://doi.org/10.1007/s11060-011-0653-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0653-y