Abstract
A total of 35 Trichosporon isolates were collected from the Taiwan Surveillance of Antimicrobial Resistance of Yeasts (TSARY) project from 1999 to 2006, and their identifications as well as drug susceptibilities were determined. The most frequently isolated species was T. asahii (62.9%), and the most common clinical sample that yielded Trichosporon isolates was urine (37.1%). The etiology of all seven invasive trichosporonosis was T. asahii. For the 22 T. asahii isolates, the MIC50 and MIC90 for amphotericin B were 0.25 and 1 μg/mL, respectively. Those for fluconazole were 2 and 4 μg/mL, respectively, and for voriconazole 0.031 and 0.063 μg/mL, respectively. When the intraclass correlation coefficients (ICCs) and agreements were calculated, we found that the MICs of fluconazole obtained from different methods were similar and the inter-method discrepancies were low. Nevertheless, no unanimous MIC of amphotericin B and voriconazole was obtained among different methods.
Similar content being viewed by others
References
Yang YL, Cheng HH, Ho YA, Hsiao CF, Lo HJ. Fluconazole resistance rate of Candida species from different regions and hospital types in Taiwan. J Microbiol Immunol Infect. 2003;36:187–91.
Yang YL, Cheng MF, Wang CW, Wang AH, Cheng WT, Lo HJ, et al. The distribution of species and susceptibility of amphotericin B and fluconazole of yeast pathogens isolated from sterile sites in Taiwan. Med Mycol. 2010;48:328–34.
Yang YL, Ho YA, Cheng HH, Ho M, Lo HJ. Susceptibilities of Candida species to amphotericin B and fluconazole: the emergence of fluconazole resistance in Candida tropicalis. Infect Control Hosp Epidemiol. 2004;25:60–4.
Yang YL, Li SY, Cheng HH, Lo HJ. Susceptibilities to amphotericin B and fluconazole of Candida species in TSARY 2002. Diagn Microbiol Infect Dis. 2005;51:179–83.
Yang YL, Wang AH, Wang CW, Cheng WT, Li SY, Lo HJ, et al. Susceptibilities to amphotericin B and fluconazole of Candida species in TSARY 2006. Diagn Microbiol Infect Dis. 2008;61:175–80.
Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011;24:682–700.
Ellner K, McBride ME, Rosen T, Berman D. Prevalence of Trichosporon beigelii. Colonization of normal perigenital skin. J Med Vet Mycol. 1991;29:99–103.
Chagas-Neto TC, Chaves GM, Melo AS, Colombo AL. Bloodstream infections due to Trichosporon spp.: species distribution, Trichosporon asahii genotypes determined on the basis of ribosomal DNA intergenic spacer 1 sequencing, and antifungal susceptibility testing. J Clin Microbiol. 2009;47:1074–81.
Hajjeh RA, Blumberg HM. Bloodstream infection due to Trichosporon beigelii in a burn patient: case report and review of therapy. Clin Infect Dis. 1995;20:913–6.
Tashiro T, Nagai H, Kamberi P, Goto Y, Kikuchi H, Nasu M, et al. Disseminated Trichosporon beigelii infection in patients with malignant diseases: immunohistochemical study and review. Eur J Clin Microbiol Infect Dis. 1994;13:218–24.
Walsh TJ. Trichosporonosis. Infect Dis Clin North Am. 1989;3:43–52.
Guo LN, Xiao M, Kong F, Chen SC, Wang H, Sorrell TC, et al. Three-locus identification, genotyping, and antifungal susceptibilities of medically important Trichosporon species from China. J Clin Microbiol. 2011;49:3805–11.
Li HM, Du HT, Liu W, Wan Z, Li RY. Microbiological characteristics of medically important Trichosporon species. Mycopathologia. 2005;160:217–25.
Rodriguez-Tudela JL, Diaz-Guerra TM, Mellado E, Cano V, Tapia C, Perkins A, et al. Susceptibility patterns and molecular identification of Trichosporon species. Antimicrob Agents Chemother. 2005;49:4026–34.
Ruan SY, Chien JY, Hsueh PR. Invasive trichosporonosis caused by Trichosporon asahii and other unusual Trichosporon species at a medical center in Taiwan. Clin Infect Dis. 2009;49:e11–7.
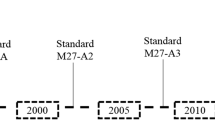
Clinical Laboratory Standards Institute CLSI. Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard-third edition. CLSI document M27-A3. Wayne, PA; 2008.
Testing SoASTotEECfAS. Subcommittee on Antifungal Susceptibility Testing of the ESCMID European Committee for Antimicrobial Susceptibility Testing: EUCAST Technical Note on the method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for conidia-forming moulds. Clin Microbiol Infect. 2008;14:982–4.
McGraw KO, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996;1:30–46.
Lo HJ, Ho AH, Ho M. Factors accounting for mis-identification of Candida species. J Microbiol Immunol Infect. 2001;34:171–7.
Leaw SN, Chang HC, Barton R, Bouchara JP, Chang TC. Identification of medically important Candida and non-Candida yeast species by an oligonucleotide array. J Clin Microbiol. 2007;45:2220–9.
Leaw SN, Chang HC, Sun HF, Barton R, Bouchara JP, Chang TC. Identification of medically important yeast species by sequence analysis of the internal transcribed spacer regions. J Clin Microbiol. 2006;44:693–9.
Kalkanci A, Sugita T, Arikan S, Yucesoy M, Ener B, Otag F, et al. Molecular identification, genotyping, and drug susceptibility of the basidiomycetous yeast pathogen Trichosporon isolated from Turkish patients. Med Mycol. 2010;48:141–6.
Nakajima M, Sugita T, Mikami Y. Granuloma associated with Trichosporon asahii infection in the lung: Unusual pathological findings and PCR detection of Trichosporon DNA. Med Mycol. 2007;45:641–4.
Taj-Aldeen SJ, Al-Ansari N, El Shafei S, Meis JF, Curfs-Breuker I, Theelen B, et al. Molecular identification and susceptibility of Trichosporon species isolated from clinical specimens in Qatar: isolation of Trichosporon dohaense Taj-Aldeen, Meis & Boekhout sp. nov. J Clin Microbiol. 2009;47:1791–9.
Girmenia C, Pagano L, Martino B, D’Antonio D, Fanci R, Specchia G, et al. Invasive infections caused by Trichosporon species and Geotrichum capitatum in patients with hematological malignancies: a retrospective multicenter study from Italy and review of the literature. J Clin Microbiol. 2005;43:1818–28.
Suzuki K, Nakase K, Kyo T, Kohara T, Sugawara Y, Shibazaki T, et al. Fatal Trichosporon fungemia in patients with hematologic malignancies. Eur J Haematol. 2010;84:441–7.
Bayramoglu G, Sonmez M, Tosun I, Aydin K, Aydin F. Breakthrough Trichosporon asahii fungemia in neutropenic patient with acute leukemia while receiving caspofungin. Infection. 2008;36:68–70.
Araujo Ribeiro M, Alastruey-Izquierdo A, Gomez-Lopez A, Rodriguez-Tudela JL, Cuenca-Estrella M. Molecular identification and susceptibility testing of Trichosporon isolates from a Brazilian hospital. Rev Iberoam Micol. 2008;25:221–5.
McGinnis MR, Pasarell L, Sutton DA, Fothergill AW, Cooper CR Jr, Rinaldi MG. In vitro activity of voriconazole against selected fungi. Med Mycol. 1998;36:239–42.
Paphitou NI, Ostrosky-Zeichner L, Paetznick VL, Rodriguez JR, Chen E, Rex JH. In vitro antifungal susceptibilities of Trichosporon species. Antimicrob Agents Chemother. 2002;46:1144–6.
Perparim K, Nagai H, Hashimoto A, Goto Y, Tashiro T, Nasu M. In vitro susceptibility of Trichosporon beigelii to antifungal agents. J Chemother. 1996;8:445–8.
Uzun O, Arikan S, Kocagoz S, Sancak B, Unal S. Susceptibility testing of voriconazole, fluconazole, itraconazole and amphotericin B against yeast isolates in a Turkish University Hospital and effect of time of reading. Diagn Microbiol Infect Dis. 2000;38:101–7.
Thompson GR III, Wiederhold NP, Sutton DA, Fothergill A, Patterson TF. In vitro activity of isavuconazole against Trichosporon, Rhodotorula, Geotrichum, Saccharomyces and Pichia species. J Antimicrob Chemother. 2009;64:79–83.
Febre N, Silva V, Medeiros EA, Wey SB, Colombo AL, Fischman O. Microbiological characteristics of yeasts isolated from urinary tracts of intensive care unit patients undergoing urinary catheterization. J Clin Microbiol. 1999;37:1584–6.
Mori Y, Hiraoka M, Katsu M, Tsukahara H, Mikami Y, Mayumi M. Marked renal damage in a child with hydronephrosis infected by Trichosporon asahii. Pediatr Nephrol. 2005;20:234–6.
Wolf DG, Falk R, Hacham M, Theelen B, Boekhout T, Scorzetti G, et al. Multidrug-resistant Trichosporon asahii infection of nongranulocytopenic patients in three intensive care units. J Clin Microbiol. 2001;39:4420–5.
Acknowledgments
The authors would like to thank Bristol Myers Squibb for supplying the reference powder of amphotericin B, and Pfizer for fluconazole and voriconazole. They also thank the TSARY hospitals, especially the following 17, for providing clinical Trichosporon isolates: Chang Gung Memorial Hospital at Keelung, Chang Gung Memorial Hospital at Linkou, Chi-Mei Foundation Hospital, Chung Shan Medical Dental College Hospital, Tainan Municipal Hospital, Kuan-Tien General Hospital, Lo-Hsu Foundation Inc. Lo-Tung Poh Ai Hospital, Kaohsiung Military Hospital, Hua-Lien Mennonite Church Hospital, National Cheng-Kung University Hospital, Hua-Lien Hospital, DOH, the Executive Yuan, Show Chwan Memorial Hospital, Tri Service General Hospital, Veterans General Hospital—Taichung, Veterans General Hospital-Kaohsiung, Asia East Memorial Hospital, and Buddhist Tzu-Chi General Hospital. This work was supported in part by the NHRI fellowship research grant to MST and by grants CL-098-PP-04 and ID-099-PP-04 from the NHRI to HJL.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsai, M.S., Yang, Y.L., Wang, A.H. et al. Susceptibilities to Amphotericin B, Fluconazole and Voriconazole of Trichosporon Clinical Isolates. Mycopathologia 174, 121–130 (2012). https://doi.org/10.1007/s11046-012-9525-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-012-9525-z