Abstract
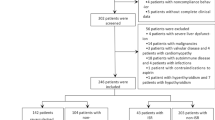
In-stent restenosis (ISR) remains the most common complication of percutaneous coronary intervention. Due to shared risk factors, it is postulated that non-alcoholic fatty liver disease (NAFLD) patients have an increased risk of ISR. This study aimed to determine the association between NAFLD and ISR in patients after bare metal stenting. This study included a cohort of 210 consecutive patients (150 men and 60 women) undergoing follow-up angiography. The primary end-point was angiographic ISR. Multivariate logistic regression analysis was used to identify independent risk factors for ISR. The cumulative ISR rate during follow-up was analyzed by Kaplan–Meier method. Subgroup analyses were also done for different gender. The ISR rate was 29.5 %. Patients with NAFLD had a significantly higher prevalence of ISR than patients without NAFLD (43.3 vs. 16.0 %, P < 0.001). In logistic regression analysis, NAFLD was associated with increased ISR, independent of low-density lipoprotein cholesterol, body mass index (adjusted odds ratio: 2.688, 95 % confidence intervals: 1.285–5.537, P < 0.001). Male NAFLD patients had a higher prevalence of ISR than patients without NAFLD (48.4 vs. 15.3 %, P < 0.001), while the prevalence of ISR in female patients with and without NAFLD were comparable (7.7 vs. 17.0 %, P = 0.404). Kaplan–Meier analysis showed a significant association between NAFLD and ISR in all patients (log-rank P = 0.008) and in male subgroup (log-rank P = 0.033), but not in female subgroup (log-rank P = 0.313). This preliminary study suggests that NAFLD could independently associate with a high prevalence of ISR, especially in male patients.



Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- CVD:
-
Cardiovascular disease
- HDL:
-
High density lipoprotein
- ISR:
-
In-stent restenosis
- LDL:
-
Low density lipoprotein
- NAFLD:
-
Non-alcoholic fatty liver disease
- OR:
-
Odds ratios
- PCI:
-
Percutaneous coronary intervention
References
Fan JG, Farrell GC (2009) Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol 50:204–210
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt CL, Harrison SA (2011) Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 140:124–131
David K, Kowdley KV, Unalp A, Kanwal F, Brunt EM, Schwimmer JB (2009) Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology 49:1904–1912
Utzschneider KM, Kahn SE (2006) Review: the role of insulin resistance in nonalcoholic fatty liver disease. J Clin Endocrinol Metab 91:4753–4761
Kasturiratne A, Weerasinghe S, Dassanayake AS, Rajindrajith S, de Silva AP, Kato N, Wickremasinghe AR, de Silva HJ (2012) Influence of non-alcoholic fatty liver disease on the development of diabetes mellitus. J Gastroenterol Hepatol 28(1):142–147
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, Natale S, Vanni E, Villanova N, Melchionda N et al (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37:917–923
Targher G, Arcaro G (2007) Non-alcoholic fatty liver disease and increased risk of cardiovascular disease. Atherosclerosis 191:235–240
Bonora E, Targher G (2012) Increased risk of cardiovascular disease and chronic kidney disease in NAFLD. Nat Rev Gastroenterol Hepatol 9:372–381
Targher G, Chonchol M, Pichiri I, Zoppini G (2011) Risk of cardiovascular disease and chronic kidney disease in diabetic patients with non-alcoholic fatty liver disease: just a coincidence? J Endocrinol Invest 34:544–551
Wong VW, Wong GL, Yip GW, Lo AO, Limquiaco J, Chu WC, Chim AM, Yu CM, Yu J, Chan FK et al (2011) Coronary artery disease and cardiovascular outcomes in patients with non-alcoholic fatty liver disease. Gut 60:1721–1727
Targher G, Day CP, Bonora E (2010) Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med 363:1341–1350
Sun Z, Almutairi AM (2010) Diagnostic accuracy of 64 multislice CT angiography in the assessment of coronary in-stent restenosis: a meta-analysis. Eur J Radiol 73:266–273
Grewe PH, Deneke T, Machraoui A, Barmeyer J, Muller KM (2000) Acute and chronic tissue response to coronary stent implantation: pathologic findings in human specimen. J Am Coll Cardiol 35:157–163
Desouza CV, Hamel FG, Bidasee K, O’Connell K (2011) Role of inflammation and insulin resistance in endothelial progenitor cell dysfunction. Diabetes 60:1286–1294
Kuwano T, Miura S, Shirai K, Ike A, Mori K, Shimizu T, Zhang B, Iwata A, Nishikawa H, Kawamura A et al (2011) Serum levels of bilirubin as an independent predictor of coronary in-stent restenosis: a new look at an old molecule. J Atheroscler Thromb 18:574–583
Obika M, Noguchi H (2012) Diagnosis and evaluation of nonalcoholic fatty liver disease. Exp Diabetes Res 2012:145754
Schomig A, Neumann FJ, Kastrati A, Schuhlen H, Blasini R, Hadamitzky M, Walter H, Zitzmann-Roth EM, Richardt G, Alt E et al (1996) A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med 334:1084–1089
Mazeika P, Prasad N, Bui S, Seidelin PH (2003) Predictors of angiographic restenosis after coronary intervention in patients with diabetes mellitus. Am Heart J 145:1013–1021
Huang Y, Bi Y, Xu M, Ma Z, Xu Y, Wang T, Li M, Liu Y, Lu J, Chen Y et al (2012) Nonalcoholic Fatty liver disease is associated with atherosclerosis in middle-aged and elderly chinese. Arterioscler Thromb Vasc Biol 32:2321–2326
Jornayvaz FR, Samuel VT, Shulman GI (2010) The role of muscle insulin resistance in the pathogenesis of atherogenic dyslipidemia and nonalcoholic fatty liver disease associated with the metabolic syndrome. Annu Rev Nutr 30:273–290
Polyzos SA, Kountouras J, Deretzi G, Zavos C, Mantzoros CS (2012) The emerging role of endocrine disruptors in pathogenesis of insulin resistance: a concept implicating nonalcoholic fatty liver disease. Curr Mol Med 12:68–82
Choi D, Kim SK, Choi SH, Ko YG, Ahn CW, Jang Y, Lim SK, Lee HC, Cha BS (2004) Preventative effects of rosiglitazone on restenosis after coronary stent implantation in patients with type 2 diabetes. Diabetes Care 27:2654–2660
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 116:1784–1792
Bugianesi E, Pagotto U, Manini R, Vanni E, Gastaldelli A, de Iasio R, Gentilcore E, Natale S, Cassader M, Rizzetto M et al (2005) Plasma adiponectin in nonalcoholic fatty liver is related to hepatic insulin resistance and hepatic fat content, not to liver disease severity. J Clin Endocrinol Metab 90:3498–3504
Kamishirado H, Inoue T, Sakuma M, Tsuda T, Hayashi T, Takayanagi K, Node K (2007) Effects of statins on restenosis after coronary stent implantation. Angiology 58:55–60
Rana JS, Mittleman MA, Ho KK, Cutlip DE (2005) Obesity and clinical restenosis after coronary stent placement. Am Heart J 150:821–826
Mehilli J, Kastrati A, Bollwein H, Dibra A, Schuhlen H, Dirschinger J, Schomig A (2003) Gender and restenosis after coronary artery stenting. Eur Heart J 24:1523–1530
Bernelot Moens SJ, Schnitzler GR, Nickerson M, Guo H, Ueda K, Lu Q, Aronovitz MJ, Nickerson H, Baur WE, Hansen U et al (2012) Rapid estrogen receptor signaling is essential for the protective effects of estrogen against vascular injury. Circulation 126(16):1993–2004
Novella S, Laguna-Fernandez A, Lazaro-Franco M, Sobrino A, Bueno-Beti C, Tarin JJ, Monsalve E, Sanchis J, Hermenegildo C (2012). Estradiol, acting through estrogen receptor alpha, restores dimethylarginine dimethylaminohydrolase activity and nitric oxide production in oxLDL-treated human arterial endothelial cells. Mol Cell Endocrinol
Vavra AK, Havelka GE, Martinez J, Lee VR, Fu B, Jiang Q, Keefer LK, Kibbe MR (2011) Insights into the effect of nitric oxide and its metabolites nitrite and nitrate at inhibiting neointimal hyperplasia. Nitric Oxide 25:22–30
El-Koofy N, El-Karaksy H, El-Akel W, Helmy H, Anwar G, El-Sayed R, El-Hennawy A (2012) Ultrasonography as a non-invasive tool for detection of nonalcoholic fatty liver disease in overweight/obese Egyptian children. Eur J Radiol 81:3120–3123
Acknowledgments
This work was supported by grants from the Scientific Research Foundation of Wenzhou, Zhejiang Province, China (H20090014, Y20090269), Health Bureau of Zhejiang Province (2010KYB070), Research Foundation of Education Bureau of Zhejiang Province (Y201009942), Fresh Talent Program for Science and Technology Department of Zhejiang Province (2013R413018, 2013R413035 and 2013R413015), Research Funds for Tian Qing Liver Diseases (TQGB20120057) and Project of New Century 551 Talent Nurturing in Wenzhou.
Conflict of interest
No.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, KQ., Wu, FL., Liu, WY. et al. Non-alcoholic fatty liver disease and risk of in-stent restenosis after bare metal stenting in native coronary arteries. Mol Biol Rep 41, 4713–4720 (2014). https://doi.org/10.1007/s11033-014-3342-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-014-3342-z