Abstract
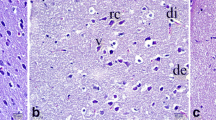
Cerebral ischemia reperfusion (IR) is associated with neuronal death, which leads to disability and cognitive decline. The pathomechanism occurs because ischemia is exacerbated during the reperfusion period. Neuronal damage susceptibility depends on the affected brain areas and the duration of ischemia. Prevention and supplementation to neurons may help them endure during IR and further benefit them in rehabilitation. We investigated the protective effect of p-coumaric acid (PC) on cerebral IR injuries in mice. We randomly divided 30 male ICR mice into 3 groups of Sham (received vehicle and not induced IR), Control-IR (received vehicle and induced IR) and PC-IR (received 100 mg/kg PC and induced IR). We orally administered vehicle or 100 mg/kg of p-coumaric acid for 2 weeks before inducing the cerebral IR injuries by using 30 min of a bilateral common carotid artery occlusion followed by a 45-min reperfusion. We induced the IR condition in the Control-IR and PC-IR groups but not the Sham group, and only the PC-IR group received p-coumaric acid. After IR induction, we sacrificed all the mice and collected their brain tissues to evaluate their oxidative statuses, whole brain infarctions and vulnerable neuronal deaths. We studied the whole-brain infarction volume by 2, 3, 5-triethyltetrazoliumchloride staining of sections. We performed a histological investigation of the vulnerable neuronal population in the dorsal hippocampus by staining brain sections with 0.1% cresyl violet. The results indicated that IR caused significant increases in calcium and malondialdehyde (MDA) levels, whole brain infarction volume and hippocampal neuronal death. Pretreatment with p-coumaric acid significantly reduced MDA levels, whole-brain infarction volume and hippocampal neuronal death together and increased catalase and superoxide dismutase activities. We conclude here that pretreating animals with p-coumaric acid can prevent IR-induced brain oxidative stress, infarction size and neuronal vulnerability to death in cerebral IR injuries.




Similar content being viewed by others
References
Abdel-Wahab MH, El-Mahdy MA, Abd-Ellah MF, Helal GK, Khalifa F, Hamada FM (2003) Influence of p-coumaric acid on doxorubicin-induced oxidative stress in rat’s heart. Pharmacol Res 48:461–465
Amalan V, Vijayakumar N, Indumathi D, Ramakrishnan A (2016) Antidiabetic and antihyperlipidemic activity of p-coumaric acid in diabetic rats, role of pancreatic GLUT 2: In vivo approach. Biomed Pharmacother 84:230–236. https://doi.org/10.1016/j.biopha.2016.09.039
Arundine M, Tymianski M (2003) Molecular mechanisms of calcium-dependent neurodegeneration in excitotoxicity. Cell Calcium 34(4-5):325–337. https://doi.org/10.1016/S0143-4160(03)00141-6
Ayala A, Munoz MF, Arguelles S (2014) Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med Cell Longev 2014:360438
Collard CD, Gelman S (2001) Pathophysiology, clinical manifestations, and prevention of ischemia-reperfusion injury. Anesthesiology 94(6):1133–1138. https://doi.org/10.1097/00000542-200106000-00030
Davolio C, Greenamyre JT (1995) Selective vulnerability of the CA1 region of hippocampus to the indirect excitotoxic effects of malonic acid. Neurosci Lett 192(1):29–32. https://doi.org/10.1016/0304-3940(95)11600-2
Guven M, Aras AB, Akman T, Sen HM, Ozkan A, Salis O, Sehitoglu I, Kalkan Y, Silan C, Deniz M, Cosar M (2015) Neuroprotective effect of p-coumaric acid in rat model of embolic cerebral ischemia. Iran J Basic Med Sci 18(4):356–363
Hadwan MH, Abed HN (2016) Data supporting the spectrophotometric method for the estimation of catalase activity. Data Brief 6:194–199. https://doi.org/10.1016/j.dib.2015.12.012
Hou ST, MacManus JP, Kwang WJ (2002) Molecular mechanisms of cerebral ischemia-induced neuronal death. Int Rev Cytol 221. Academic Press, pp 93–148
Iwasaki Y, Ito S, Suzuki M, Nagahori T, Yamamoto T, Konno H (1989) Forebrain ischemia induced by temporary bilateral common carotid occlusion in normotensive rats. J Neurol Sci 90(2):155–165. https://doi.org/10.1016/0022-510X(89)90098-1
Jivad N, Rabiei Z (2015) Review on herbal medicine on brain ischemia and reperfusion. Asian Pac J Trop Biomed 5(10):789–795. https://doi.org/10.1016/j.apjtb.2015.07.015
Kalogeris T, Baines CP, Krenz M, Korthuis RJ, Kwang WJ (2012) Chapter six - cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol 298. Academic Press, pp 229–317. https://doi.org/10.1016/B978-0-12-394309-5.00006-7
Ladecola C, Anrather J (2011) Stroke research at a crossroad: asking the brain for directions. Nat Neurosci 14(11):1363–1368. https://doi.org/10.1038/nn.2953
Leker RR, Shohami E (2002) Cerebral ischemia and trauma different etiologies yet similar mechanisms: neuroprotective opportunities. Brain Res Rev 39(1):55–73. https://doi.org/10.1016/S0165-0173(02)00157-1
Martin LJ, Al-Abdulla NA, Brambrink AM, Kirsch JR, Sieber FE, Portera-Cailliau C (1998) Neurodegeneration in excitotoxicity, global cerebral ischemia, and target deprivation: a perspective on the contributions of apoptosis and necrosis. Brain Res Bull 46(4):281–309. https://doi.org/10.1016/S0361-9230(98)00024-0
Mattson MP, Kater SB (1989) Development and selective neurodegeneration in cell cultures from different hippocampal regions. Brain Res 490(1):110–125. https://doi.org/10.1016/0006-8993(89)90436-8
Mehta SL, Kumari S, Mendelev N, Li PA (2012) Selenium preserves mitochondrial function, stimulates mitochondrial biogenesis, and reduces infarct volume after focal cerebral ischemia. BMC Neurosci 13(1):79. https://doi.org/10.1186/1471-2202-13-79
Pan J, Konstas AA, Bateman B, Ortolano GA, Pile-Spellman J (2007) Reperfusion injury following cerebral ischemia: pathophysiology, MR imaging, and potential therapies. Neuroradiology 49(2):93–102. https://doi.org/10.1007/s00234-006-0183-z
Pandey KB, Rizvi SI (2009) Plant polyphenols as dietary antioxidants in human health and disease. Oxidative Med Cell Longev 2(5):270–278. https://doi.org/10.4161/oxim.2.5.9498
Paxinos G, Franklin K (2008) The mouse brain in stereotaxic coordinates. 3rd edn. Academic Press, San Diego
Pei K, Ou J, Huang J, Ou S (2015) p-Coumaric acid and its conjugates: dietary sources, pharmacokinetic properties and biological activities. J Sci Food Agric 96(9):2952–2962. https://doi.org/10.1002/jsfa.7578
Raghavendra M, Rituparna M, Shafalika K, Anshuman T, Sumit M, S A (2009) Role of Centella asiatica on cerebral post-ischemic reperfusion and long-term hypoperfusion in rats. Int J Green Pharm 3:88–96, https://doi.org/10.4103/0973-8258.54893
Shuaib A, Breker-Klassen MM (1997) Inhibitory mechanisms in cerebral ischemia: a brief review. Neurosci Biobehav Rev 21(2):219–226. https://doi.org/10.1016/S0149-7634(96)00012-7
Spare PD (1964) A stable murexide reagent for the estimation of calcium in micro quantities of serum. Clin Chem 10:726–729
Taupin P (2006) Neurogenesis in the adult central nervous system. C R Biol 329(7):465–475. https://doi.org/10.1016/j.crvi.2006.04.001
Thong-asa W, Tilokskulchai K (2014) Neuronal damage of the dorsal hippocampus induced by long-term right common carotid artery occlusion in rats. Iran J Basic Med Sci 17(3):220–226
Wang X, Pal R, Chen XW, Limpeanchob N, Kumar KN, Michaelis EK (2005) High intrinsic oxidative stress may underlie selective vulnerability of the hippocampal CA1 region. Brain Res Mol Brain Res 140(1-2):120–126. https://doi.org/10.1016/j.molbrainres.2005.07.018
White BC, Sullivan JM, DeGracia DJ, O’Neil BJ, Neumar RW, Grossman LI, Rafols JA, Krause GS (2000) Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci 179(1-2):1–33. https://doi.org/10.1016/S0022-510X(00)00386-5
Yoon JH, Youn K, Ho CT, Karwe MV, Jeong WS, Jun M (2014) p-Coumaric acid and ursolic acid from Corni fructus attenuated beta-amyloid(25-35)-induced toxicity through regulation of the NF-kappaB signaling pathway in PC12 cells. J Agric Food Chem 62(21):4911–4916. https://doi.org/10.1021/jf501314g
Zhang Y, Hu W (2012) NFkappaB signaling regulates embryonic and adult neurogenesis. Front Biol (Beijing) 7(4):277–291. https://doi.org/10.1007/s11515-012-1233-z
Acknowledgements
We would like to thank the Animal Toxicology and Physiology Specialty Research Unit (ATPRS). The present study was supported by grant from the Department of Zoology (Project in Zoology of Graduate Program), Faculty of Science, Kasetsart University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that no conflict of interest.
Rights and permissions
About this article
Cite this article
Sakamula, R., Thong-asa, W. Neuroprotective effect of p-coumaric acid in mice with cerebral ischemia reperfusion injuries. Metab Brain Dis 33, 765–773 (2018). https://doi.org/10.1007/s11011-018-0185-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-018-0185-7