Abstract
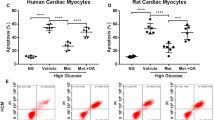
Cardiomyocyte death is an important pathogenic process in cardiac complications of diabetes. Diabetic patients often suffer glycemic variability. Pyroptosis is a form of programmed cell death triggered by inflammasomes and related with caspase-1 and gasdermin D activation. The present study was designed to examine the effects of intermittent high glucose simulating glycemic variability on the pyroptosis of cardiomyocytes in vitro. Rat H9C2 cardiomyocytes were incubated with normal glucose (NG), constant high glucose (CHG) and intermittent high glucose (IHG). Results showed that compared to CHG treatment, IHG further inhibited cell proliferation and promoted cell death of H9C2 cardiomyocytes. In addition, IHG upregulated higher levels of the expressions of inflammasome NLR family pyrin domain containing 3 (NLRP3) and adaptor protein apoptosis-associated speck-like protein containing CARD domain (ASC) and increased higher levels of activated caspase-1 and gasdermin D than CHG treatment. Moreover, the production of reactive oxygen species (ROS) and activation of NF-κB that is induced by IHG were significantly higher than that induced by CHG. Knockdown of sodium–glucose cotransporters 1 (SGLT1) in H9C2 cardiomyocytes was performed and the effects of SGLT1 on IHG-induced pyroptosis was evaluated. The results demonstrated that knockdown of SGLT1 partially reduced IHG-induced pyroptosis, ROS generation and NF-κB activation. Our results indicated that IHG is harmful to cardiomyocytes and it might be partially because of the SGLT1-depedent pyroptosis in cardiomyocytes.






Similar content being viewed by others
References
Frangogiannis NG (2015) Pathophysiology of myocardial infarction. Compr Physiol 5:1841–1875. https://doi.org/10.1002/cphy.c150006
Takemura G, Kanamori H, Okada H, Miyazaki N, Watanabe T, Tsujimoto A, Goto K, Maruyama R, Fujiwara T, Fujiwara H (2018) Anti-apoptosis in nonmyocytes and pro-autophagy in cardiomyocytes: two strategies against postinfarction heart failure through regulation of cell death/degeneration. Heart Fail Rev 23:759–772. https://doi.org/10.1007/s10741-018-9708-x
Mishra PK, Adameova A, Hill JA, Baines CP, Kang PM, Downey JM, Narula J, Takahashi M, Abbate A, Piristine HC, Kar S, Su S, Higa JK, Kawasaki NK, Matsui T (2019) Guidelines for evaluating myocardial cell death. Am J Physiol Heart Circ Physiol 317:H891–H922. https://doi.org/10.1152/ajpheart.00259.2019
Zhaolin Z, Guohua L, Shiyuan W, Zuo W (2019) Role of pyroptosis in cardiovascular disease. Cell Prolif 52:e12563. https://doi.org/10.1111/cpr.12563
Fang Y, Tian S, Pan Y, Li W, Wang Q, Tang Y, Yu T, Wu X, Shi Y, Ma P, Shu Y (2020) Pyroptosis: a new frontier in cancer. Biomed Pharmacother 121:109595. https://doi.org/10.1016/j.biopha.2019.109595
Shi J, Gao W, Shao F (2017) Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci 42:245–254. https://doi.org/10.1016/j.tibs.2016.10.004
Hoseini Z, Sepahvand F, Rashidi B, Sahebkar A, Masoudifar A, Mirzaei H (2018) NLRP3 inflammasome: its regulation and involvement in atherosclerosis. J Cell Physiol 233:2116–2132. https://doi.org/10.1002/jcp.25930
Wu X, Zhang H, Qi W, Zhang Y, Li J, Li Z, Lin Y, Bai X, Liu X, Chen X, Yang H, Xu C, Yang B (2018) Nicotine promotes atherosclerosis via ROS-NLRP3-mediated endothelial cell pyroptosis. Cell Death Dis 9:171. https://doi.org/10.1038/s41419-017-0257-3
Toldo S, Mauro AG, Cutter Z, Abbate A (2018) Inflammasome, pyroptosis, and cytokines in myocardial ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 315:H1553–H1568. https://doi.org/10.1152/ajpheart.00158.2018
Yang F, Qin Y, Wang Y, Meng S, Xian H, Che H, Lv J, Li Y, Yu Y, Bai Y, Wang L (2019) Metformin inhibits the NLRP3 inflammasome via AMPK/mTOR-dependent effects in diabetic cardiomyopathy. Int J Biol Sci 15:1010–1019. https://doi.org/10.7150/ijbs.29680
Luo B, Li B, Wang W, Liu X, Xia Y, Zhang C, Zhang M, Zhang Y, An F (2014) NLRP3 gene silencing ameliorates diabetic cardiomyopathy in a type 2 diabetes rat model. PLoS ONE 9:e104771. https://doi.org/10.1371/journal.pone.0104771
Kuricova K, Pacal L, Soupal J, Prazny M, Kankova K (2016) Effect of glucose variability on pathways associated with glucotoxicity in diabetes: evaluation of a novel in vitro experimental approach. Diabetes Res Clin Pract 114:1–8. https://doi.org/10.1016/j.diabres.2016.02.006
Marshall RJ, Armart P, Hulme KD, Chew KY, Brown AC, Hansbro PM, Bloxham CJ, Flint M, Ronacher K, Bielefeldt-Ohmann H, Gallo LA, Short KR (2020) Glycemic variability in diabetes increases the severity of influenza. mBio. https://doi.org/10.1128/mBio.02841-19
Perlman EJ, Moore GW, Hutchins GM (1989) The pulmonary vasculature in meconium aspiration. Hum Pathol 20:701–706. https://doi.org/10.1016/0046-8177(89)90159-7
Cao G, Fan J, Yu H, Chen Z (2018) Resveratrol attenuates high glucose-induced cardiomyocytes injury via interfering ROS-MAPK-NF-kappaB signaling pathway. Int J Clin Exp Pathol 11:48–57
Zhang X, Lin Q, Chen J, Wei T, Li C, Zhao L, Gao H, Zheng H (2018) High glucose-induced cardiomyocyte death may be linked to unbalanced branched-chain amino acids and energy metabolism. Molecules. https://doi.org/10.3390/molecules23040807
Qiu Z, Lei S, Zhao B, Wu Y, Su W, Liu M, Meng Q, Zhou B, Leng Y, Xia ZY (2017) NLRP3 inflammasome activation-mediated pyroptosis aggravates myocardial ischemia/reperfusion injury in diabetic rats. Oxid Med Cell Longev 2017:9743280. https://doi.org/10.1155/2017/9743280
Kim M, Chung H, Yoon C, Lee E, Kim T, Kwon M, Lee S, Rhee B, Park J (2012) Increase of INS-1 cell apoptosis under glucose fluctuation and the involvement of FOXO-SIRT pathway. Diabetes Res Clin Pract 98:132–139. https://doi.org/10.1016/j.diabres.2012.04.013
Wang JS, Huang Y, Zhang S, Yin HJ, Zhang L, Zhang YH, Song YW, Li DD (2019) A protective role of paeoniflorin in fluctuant hyperglycemia-induced vascular endothelial injuries through antioxidative and anti-inflammatory effects and reduction of PKCbeta1. Oxid Med Cell Longev 2019:5647219. https://doi.org/10.1155/2019/5647219
Yin X, Zheng F, Pan Q, Zhang S, Yu D, Xu Z, Li H (2015) Glucose fluctuation increased hepatocyte apoptosis under lipotoxicity and the involvement of mitochondrial permeability transition opening. J Mol Endocrinol 55:169–181. https://doi.org/10.1530/JME-15-0101
Poulsen SB, Fenton RA, Rieg T (2015) Sodium-glucose cotransport. Curr Opin Nephrol Hypertens 24:463–469. https://doi.org/10.1097/mnh.0000000000000152
Rieg T, Vallon V (2018) Development of SGLT1 and SGLT2 inhibitors. Diabetologia 61:2079–2086. https://doi.org/10.1007/s00125-018-4654-7
Boeder S, Edelman SV (2019) Sodium-glucose co-transporter inhibitors as adjunctive treatment to insulin in type 1 diabetes: a review of randomized controlled trials. Diabetes Obes Metab 21(Suppl 2):62–77. https://doi.org/10.1111/dom.13749
Zambrowicz B, Freiman J, Brown PM, Frazier KS, Turnage A, Bronner J, Ruff D, Shadoan M, Banks P, Mseeh F, Rawlins DB, Goodwin NC, Mabon R, Harrison BA, Wilson A, Sands A, Powell DR (2012) LX4211, a dual SGLT1/SGLT2 inhibitor, improved glycemic control in patients with type 2 diabetes in a randomized, placebo-controlled trial. Clin Pharmacol Ther 92:158–169. https://doi.org/10.1038/clpt.2012.58
Li Z, Agrawal V, Ramratnam M, Sharma RK, D’Auria S, Sincoular A, Jakubiak M, Music ML, Kutschke WJ, Huang XN, Gifford L, Ahmad F (2019) Cardiac sodium-dependent glucose cotransporter 1 is a novel mediator of ischaemia/reperfusion injury. Cardiovasc Res 115:1646–1658. https://doi.org/10.1093/cvr/cvz037
Balteau M, Tajeddine N, de Meester C, Ginion A, Des Rosiers C, Brady NR, Sommereyns C, Horman S, Vanoverschelde JL, Gailly P, Hue L, Bertrand L, Beauloye C (2011) NADPH oxidase activation by hyperglycaemia in cardiomyocytes is independent of glucose metabolism but requires SGLT1. Cardiovasc Res 92:237–246. https://doi.org/10.1093/cvr/cvr230
Luo B, Huang F, Liu Y, Liang Y, Wei Z, Ke H, Zeng Z, Huang W, He Y (2017) NLRP3 Inflammasome as a molecular marker in diabetic cardiomyopathy. Front Physiol 8:519. https://doi.org/10.3389/fphys.2017.00519
Meng L, Lin H, Zhang J, Lin N, Sun Z, Gao F, Luo H, Ni T, Luo W, Chi J, Guo H (2019) Doxorubicin induces cardiomyocyte pyroptosis via the TINCR-mediated posttranscriptional stabilization of NLR family pyrin domain containing 3. J Mol Cell Cardiol 136:15–26. https://doi.org/10.1016/j.yjmcc.2019.08.009
Ye B, Chen X, Dai S, Han J, Liang X, Lin S, Cai X, Huang Z, Huang W (2019) Emodin alleviates myocardial ischemia/reperfusion injury by inhibiting gasdermin D-mediated pyroptosis in cardiomyocytes. Drug Des Devel Ther 13:975–990. https://doi.org/10.2147/DDDT.S195412
Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, MacDonald K, Speert D, Fernandes-Alnemri T, Wu J, Monks BG, Fitzgerald KA, Hornung V, Latz E (2009) Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol 183:787–791. https://doi.org/10.4049/jimmunol.0901363
Qiu Z, He Y, Ming H, Lei S, Leng Y, Xia ZY (2019) Lipopolysaccharide (LPS) aggravates high glucose- and hypoxia/reoxygenation-induced injury through activating ROS-dependent NLRP3 inflammasome-mediated pyroptosis in H9C2 cardiomyocytes. J Diabetes Res 2019:8151836. https://doi.org/10.1155/2019/8151836
Simard JC, Cesaro A, Chapeton-Montes J, Tardif M, Antoine F, Girard D, Tessier PA (2013) S100A8 and S100A9 induce cytokine expression and regulate the NLRP3 inflammasome via ROS-dependent activation of NF-κB(1). PLoS ONE 8:e72138. https://doi.org/10.1371/journal.pone.0072138
Wei H, Bu R, Yang Q, Jia J, Li T, Wang Q, Chen Y (2019) Exendin-4 protects against hyperglycemia-induced cardiomyocyte pyroptosis via the AMPK-TXNIP pathway. J Diabetes Res 2019:8905917. https://doi.org/10.1155/2019/8905917
Zhong Y, Wang JJ, Zhang SX (2012) Intermittent but not constant high glucose induces ER stress and inflammation in human retinal pericytes. Adv Exp Med Biol 723:285–292. https://doi.org/10.1007/978-1-4614-0631-0_37
Wu N, Shen H, Liu H, Wang Y, Bai Y, Han P (2016) Acute blood glucose fluctuation enhances rat aorta endothelial cell apoptosis, oxidative stress and pro-inflammatory cytokine expression in vivo. Cardiovasc Diabetol 15:109. https://doi.org/10.1186/s12933-016-0427-0
Piconi L, Corgnali M, Da Ros R, Assaloni R, Piliego T, Ceriello A (2008) The protective effect of rosuvastatin in human umbilical endothelial cells exposed to constant or intermittent high glucose. J Diabetes Complications 22:38–45. https://doi.org/10.1016/j.jdiacomp.2007.03.004
Del Guerra S, Grupillo M, Masini M, Lupi R, Bugliani M, Torri S, Boggi U, Del Chiaro M, Vistoli F, Mosca F, Del Prato S, Marchetti P (2007) Gliclazide protects human islet beta-cells from apoptosis induced by intermittent high glucose. Diabetes Metab Res Rev 23:234–238. https://doi.org/10.1002/dmrr.680
Zhang W, Song J, Zhang Y, Ma Y, Yang J, He G, Chen S (2018) Intermittent high glucose-induced oxidative stress modulates retinal pigmented epithelial cell autophagy and promotes cell survival via increased HMGB1. BMC Ophthalmol 18:192. https://doi.org/10.1186/s12886-018-0864-5
Zhou L, Cryan EV, D’Andrea MR, Belkowski S, Conway BR, Demarest KT (2003) Human cardiomyocytes express high level of Na+/glucose cotransporter 1 (SGLT1). J Cell Biochem 90:339–346. https://doi.org/10.1002/jcb.10631
Matsushita N, Ishida N, Ibi M, Saito M, Sanbe A, Shimojo H, Suzuki S, Koepsell H, Takeishi Y, Morino Y, Taira E, Sawa Y, Hirose M (2018) Chronic pressure overload induces cardiac hypertrophy and fibrosis via increases in SGLT1 and IL-18 gene expression in mice. Int Heart J 59:1123–1133. https://doi.org/10.1536/ihj.17-565
Meng L, Uzui H, Guo H, Tada H (2018) Role of SGLT1 in high glucose level-induced MMP-2 expression in human cardiac fibroblasts. Mol Med Rep 17:6887–6892. https://doi.org/10.3892/mmr.2018.8688
Yu LC, Turner JR, Buret AG (2006) LPS/CD14 activation triggers SGLT-1-mediated glucose uptake and cell rescue in intestinal epithelial cells via early apoptotic signals upstream of caspase-3. Exp Cell Res 312:3276–3286. https://doi.org/10.1016/j.yexcr.2006.06.023
Yaribeygi H, Atkin SL, Butler AE, Sahebkar A (2019) Sodium-glucose cotransporter inhibitors and oxidative stress: an update. J Cell Physiol 234:3231–3237. https://doi.org/10.1002/jcp.26760
Danne T, Biester T, Kordonouri O (2018) Combined SGLT1 and SGLT2 inhibitors and their role in diabetes care. Diabetes Technol Ther 20:S269-s277. https://doi.org/10.1089/dia.2018.0081
Ohgaki R, Wei L, Yamada K, Hara T, Kuriyama C, Okuda S, Ueta K, Shiotani M, Nagamori S, Kanai Y (2016) Interaction of the sodium/glucose cotransporter (SGLT) 2 inhibitor canagliflozin with SGLT1 and SGLT2. J Pharmacol Exp Ther 358:94–102. https://doi.org/10.1124/jpet.116.232025
Funding
This study was funded by the National Natural Science Foundation of China (No. 81870565).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chai, Q., Meng, Z., Lu, D. et al. Intermittent high glucose induces pyroptosis of rat H9C2 cardiomyocytes via sodium–glucose cotransporter 1. Mol Cell Biochem 476, 2479–2489 (2021). https://doi.org/10.1007/s11010-021-04104-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-021-04104-6