Abstract
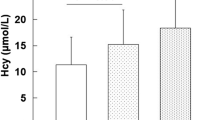
Objective To determine the incidence of methylene tetrahydrofolate reductase (MTHFR) gene 677C→T polymorphism and plasma homocysteine (Hcy) levels in a group of subjects who underwent coronary angiography, in an attempt to establish a correlation between these parameters and the severity of coronary artery disease (CAD) and to investigate the correlation between hyperhomocysteinemia (HHcy) and the presence of 677C→T polymorphism. Background Elevated plasma Hcy level is an independent risk factor for CAD. A common mutation (677C→T) in the gene coding for MTHFR has been reported to reduce the enzymatic activity and is associated with elevated levels of Hcy, especially in subjects with low folate intake. Methods The study group comprised of 84 patients with CAD and 100 age-and-sex matched controls who had no history or clinical evidence of CAD and/or MI. DNA was extracted from peripheral blood and genotypes were determined by polymerase chain reaction, restriction mapping with Hinf1, and gel electrophoresis. Conventional risk factors for CAD were prospectively documented. Results Allele and genotype frequencies in cases and control subjects were compatible with Hardy–Weinberg equilibrium. The frequencies of TT, CT, and CC genotypes among CAD patients were 4.8, 27.4, and 67.8% and in controls were 1.0, 19.0, and 80%. Hcy levels were higher in patients with triple-vessel disease compared to single and double vessel disease (P = 0.002). Multivariate analyses identified HHcy, diabetes mellitus, and hypertension as the independent predictors of CAD. Conclusions HHcy appears to have a graded effect on the risk of CAD as well as the severity and extent of coronary atherosclerosis. Our findings support that homozygous genotype of MTHFR is a genetic risk factor for CAD. A further study with larger sample size including assessment of vitamin status is needed to better clarify the relationship between MTHFR genotypes and CAD.
Similar content being viewed by others
References
Suematsu N, Ojaimi C, Kinugawa S, Wang Z, Xu X, Koller A, Recchia FA, Hintze TH (2007) Hyperhomocysteinemia alters cardiac substrate metabolism by impairing nitric oxide bioavailability through oxidative stress. Circulation 115:255–262
Boers GH (1994) Hyperhomocysteinaemia: a newly recognized risk factor for vascular disease. Neth J Med 45:34–41
Mueller PW, Thacker SB (2002) Homocystine and cardiovascular disease: a systematic review of the evidence with special emphasis on case-control studies and nested case-control studies. Int J Epidemiol 31:59–70
Refsum U, Ueland PM, Nygård O, Vollset SE (1998) Homocysteine and vascular disease. Ann Rev Med 49:31–62
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJH, den Heijer M, Kluijtmans LAJ, van den Heuvel LP, Rozen R (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylene tetrahydrofolate reductase. Nat Genet 10:111–113
Guenther BD, Sheppard CA, Tran P, Rozen R, Matthews RG, Ludwig ML (1999) The structure and properties of methylene tetrahydrofolate reductase from Escherichia coli suggest how folate ameliorates human hyperhomocysteinemia Nat Struct Biol 6:359–365
Morita H, Taguchi J, Kurihara H, Kitaoka M, Kaneda H, Kurihara Y, Maemura K, Shindo T, Minamino T, Ohno M, Yamaoki K, Ogasawara K, Aizawa T, Suzuki S, Yazaki Y (1997) Genetic polymorphism of 5,10-methylene tetrahydrofolate reductase (MTHFR) as a risk factor for coronary artery disease. Circulation 95:2032–2036
Kluijtmans LAJ, van den Heuvel LP, Boers GHJ, Frosst P, Stevens EMB, van Oost BA, den Heijer M, Trijbels FJM, Rozen R, Blom HJ (1996) Molecular genetic analysis in mild hyperhomocysteinemia: a common mutation in the methylene tetrahydrofolate reductase gene is a genetic risk factor for cardiovascular disease. Am J Hum Genet 58:35–41
Meleady R, Ueland PM, Blom B, Whitehead AS, Refsum H, Daly LE, Vollset SE, Donohue C, Giesendorf B, Graham IM, Ulvik A, Zhang Y, Monsen ALB (2003) Thermolabile methylene tetrahydrofolate reductase, homocysteine, and cardiovascular disease risk: The European Concerted Action Project. Am J Clin Nutr 77:63–70
Chambers JC, Ireland H, Thompson E, Reilly P, Obeid OA, Refsum H, Ueland P, Lane DA, Kooner JS (2000) Methylene tetrahydrofolate reductase 677 C→T mutation and coronary heart disease risk in UK Indian Asians. Arterioscler Thromb Vasc Biol 20:2448–2452
Tsai MY, Welge BG, Hanson NQ, Bignell MK, Vessey J, Schwichtenberg K, Yang F, Bullemer FE, Rasmussen R, Graham KJ (1999) Genetic causes of mild hyperhomocysteinemia in patients with premature occlusive coronary artery disease. Atherosclerosis 143:163–170
Gardemann A, Weidemann H, Philipp M, Katz N, Tillmanns H, Hehrlein FW, Haberbosch W (1999) The TT genotype of the methylene tetrahydrofolate reductase C677T gene polymorphism is associated with the extent of coronary atherosclerosis in patients at high risk for coronary artery disease. Eur Heart J 20:584–592
Laraqui A, Allami A, Carrié A, Raisonnier A, Coiffard AS, Benkouka F, Bendriss A, Benjouad A, Bennouar N, El Kadiri N, Benomar A, Fellat S, Benomar M (2007) Relation between plasma homocysteine, gene polymorphisms of homocysteine metabolism-related enzymes, and angiographically proven coronary artery disease. Eur J Intern Med 18:474–483
Gallagher PM, Meleady R, Shields DC, Tran KS, McMaster D, Rozen R, Evans A, Graham IM, Whitehead AS (1996) Homocysteine and risk of premature coronary heart disease: evidence for a common gene mutation. Circulation 94:2154–2158
Eikelboom JW, Lonn E, Genest J Jr, Hankey G, Yusuf S (1999) Homocyst(e)ine and cardiovascular disease: a critical review of epidemiological evidence. Ann Intern Med 131:363–375
Zheng YZ, Tong J, Do XP, Pu XQ, Zhou BT (2000) Prevalence of methylene tetrahydrofolate reductase C677T and its association with arterial and venous thrombosis in the Chinese population. Br J Haematol 109:870–874
Nair KG, Nair SR, Ashavaid TF, Dalal JJ, Eghlim FF (2002) Methylene tetrahydrofolate reductase gene mutation and hyperhomocysteinemia as a risk factor for coronary heart disease in the Indian population. J Assoc Physicians India 50:S9–S15
Mukherjee M, Joshi S, Bagadi S, Dalvi M, Rao A, Shetty KR (2002) A low prevalence of the C677T mutation in the methylene tetrahydrofolate reductase gene in Asian Indians. Clin Genet 61:155–159
Refsum H, Yajnik CS, Gadkari M, Schneede J, Vollset SE, Orning L, Guttormsen AB, Joglekar A, Sayyad MG, Ulvik A, Ueland PM (2001) Hyperhomocysteinemia and elevated methylmalonic acid indicate a high prevalence of cobalamin deficiency in Asian Indians. Am J Clin Nutr 74:233–241
Karthikeyan G, Prabhakaran D, Reddy KS (2002) Plasma homocysteine levels and cardiovascular risk in Indians. J Assoc Physicians India 50:S24–S28
Graham IM, Daly LE, Refsum HM et al (1997) Plasma homocysteine as a risk factor for vascular disease. The European Concerted Action Project. J Am Med Assoc 277:1775–1781
Evans RW, Shaten BJ, Hempel JD, Cutler JA, Kuller LH (1997) Homocysteine and risk of cardiovascular disease in Multiple Risk Factor Interventional Trial. Arterioscler Thromb Vasc Biol 17:1947–1953
Ubbink JB, Fehily AM, Pickering J, Elwood PC, Vermaak WJH (1998) Homocysteine and ischaemic heart disease in the Caerphilly cohort. Atherosclerosis 140:349–356
Danesh J, Lewington S (1998) Plasma homocysteine and coronary heart disease:systematic review of published epidemiologic studies. J Cardiovasc Risk 5:217–221
Kark JD, Selhub J, Adler B (1999) Non-fasting plasma total homocysteine level and mortality in middle-aged and elderly men and women in Jerusalem. Ann Intern Med 131:321–330
Angeline T, Jeyaraj N, Tsongalis GJ (2007) MTHFR Gene polymorphisms, B-vitamins and hyperhomocystinemia in young and middle-aged acute myocardial infarction patients. Exp Mol Pathol 82:227–233
Markan S, Sachdeva M, Sehrawat BS, Kumari S, Jain S, Khullar M (2007) MTHFR 677 CT/MTHFR 1298 CC genotypes are associated with increased risk of hypertension in Indians. Mol Cell Biochem 302:125–131
Vasisht S, Gulati R, Narang R, Srivastava N, Srivastava LM, Manchanda SC, Agarwal DP (2002) Polymorphism (C677T) in the 5,10- methylene tetrahydrofolate reductase gene: a preliminary study on North Indian men. Indian J Clin Biochem 17:99–107
McAndrew PE, Brandt JT, Pearl DK, Prior TW (1996) The incidence of the gene for thermolabile methylene tetrahydrofolate reductase in African Americans. Thromb Res 83:195–198
Huh HJ, Chi HS, Shim EH, Jang S, Park CJ (2006) Gene–nutrition interactions in coronary artery disease: correlation between the MTHFR C677T polymorphism and folate and homocysteine status in a Korean population. Thromb Res 117:501–506
Klerk M, Verhoef P, Clarke R, Blom HJ, Kok FJ, Schouten EG (2002) MTHFR Studies Collaboration Group. MTHFR 677C→T polymorphism and risk of coronary heart disease: a meta-analysis. JAMA 288:2023–2031
Wald DS, Law M, Morris JK (2002) Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. Br Med J 325:1202–1209
Cronin S, Furie KL, Kelly PJ (2005) Dose-related association of MTHFR 677T allele with risk of ischemic stroke: evidence from a cumulative meta-analysis. Stroke 36:1581–1587
Mager A, Lalezari S, Shohat T, Birnbaum Y, Adler Y, Magal N, Shohat M (1999) Methylene tetrahydrofolate reductase genotypes and early-onset coronary artery disease. Circulation 100:2406–2410
Brattstrom L, Wilcken DEL, Ohrvik J, Brudin L (1998) The common methylene tetrahydrofolate reductase gene mutation leads to hyperhomocysteinemia but not to vascular disease—the results of a meta-analysis. Circulation 98:2520–2526
Weiss N (2005) Mechanisms of increased vascular oxidant stress in hyperhomocys-teinemia and its impact on endothelial function. Curr Drug Metab 6:27–36
Thambyrajah J, Townend JN (2000) Homocysteine and atherothrombosis: mechanisms for injury. Eur Heart J 21:967–974
Bockxmeer FMV, Mamotte CDS, Vasikaran SD, Taylor RR (1997) Methylene tetrahydrofolate reductase gene and coronary artery disease. Circulation 95:21–23
Lievers KJ, Kluijtmans LA, Blom HJ (2003) Genetics of hyperhomocysteinaemia in cardiovascular disease. Ann Clin Biochem 40:46–59
Bostom AG, Silbershatz H, Rosenberg IH, Selhub J, D’Agostino RB, Wolf PA, Jacques PF, Wilson PW (1999) Nonfasting plasma total homocysteine levels and all-cause and cardiovascular disease mortality in elderly Framingham men and women. Arch Intern Med 159:1077–1080
Stampfer MJ, Malinow MR, Willet WC, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH (1992) A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. J Am Med Assoc 268:877–881
Alfthan G, Pekkanen J, Jauhiainen M, Pitkaniemi J, Karvonen M, Tuomilehto J, Salonen JT, Ehnholm C (1994) Relation of serum homocysteine and lipoprotein (a) concentration to atherosclerotic disease in a prospective Finnish population based study. Atherosclerosis 106:9–19
Christen WG, Ajani UQ, Glynn RJ, Hennekens CH (2000) Blood levels of homocysteine and increased risk of cardiovascular disease. Arch Intern Med; 160:422–434
Voutilainen S, Lakka TA, Hämelahti P, Lehtimäki T, Poulsen HE, Salonen JT (2000) Plasma total homocysteine concentration and the risk of acute coronary events: the Kuopio ischemic heart disease risk factor study. J Int Med 248:217–222
Wald NJ, Watt HC, Law MR, Weir DG, McPartlin J, Scott JM (1998) Homocysteine and ischaemic heart disease. Results of a prospective study with implications regarding prevention. Arch Intern Med 158:862–867
Acknowledgments
This study was supported by the grants from Indian Council of Medical Research, Ministry of Health, Government of India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alam, M.A., Husain, S.A., Narang, R. et al. Association of polymorphism in the thermolabile 5, 10-methylene tetrahydrofolate reductase gene and hyperhomocysteinemia with coronary artery disease. Mol Cell Biochem 310, 111–117 (2008). https://doi.org/10.1007/s11010-007-9671-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-007-9671-7