Abstract
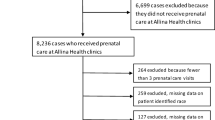
Objectives The Edinburgh Postnatal Depression Scale (EPDS) identifies women with depressive symptoms in pregnancy. Our primary objective was to determine the prevalence of EPDS screen-positive women delivering on our no prenatal care (laborist) service and to compare these patients to private patients delivering with prenatal care. Methods Retrospective cohort analysis of EPDS scores during January 1, 2015 to June 18, 2015 was conducted. Scores ≥ 10 were considered at-risk. Results were analyzed as an aggregate and then as no prenatal care versus prenatal care. Characteristics for patients with at-risk scores (EPDS ≥ 10) versus low-risk scores (EPDS < 10) were quantified. Results Analysis occurred on 970 women. EPDS ≥ 10 occurred in 12.4% (n = 120/970). Positive EPDS score was 21.1% without prenatal care versus 10.9% with adequate prenatal care (P = 0.003). Maternal demographics and delivery characteristics were clinically similar in patients with prenatal care compared to no prenatal care. Private insurance was more common in patients with prenatal care compared to no prenatal care (23.5 versus 8.1%, P = 0.0001). However, analysis of patients with EPDS > 10 showed non-significant distributions of ethnicity, private insurance, Medicaid, or no insurance compared to patients with EPDS < 10. Conclusion for Practice Patients without prenatal care who arrive solely for urgent “drop-in” delivery have a measurable increased risk factor for postpartum depressive symptoms. Ethnicity and payor status were related to adequacy of prenatal care but were not significant variables when analyzing patients with EPDS > 10. Laborist services providing care to “drop-in” patients should recognize this increased risk and develop policies for screening, referral and follow-up of at-risk patients.
Similar content being viewed by others
References
Alabama Perinatal Excellence Collaborative. (2017). Depression screening & treatment. APEC Guidelines. http://apecguidelines.org/guideline/depression-s-t/. Accessed 05 December 2017.
American College of Obstetricians and Gynecologists. (2015). Screening for perinatal depression. Committee Opinion No. 630. Obstetrics & Gynecology, 125, 1268–1271.
Baer, R. J., Altman, M. R., Oltman, S. P., et al. (2018). Maternal factors influencing late entry into prenatal care: A stratified analysis by race or ethnicity and insurance status. The Journal of Maternal-Fetal & Neonatal Medicine, 1–7.
Beck, C. T. (2001). Predictors of postpartum depression. Nursing Research, 50(5), 275–285.
Brummelte, S., & Galea, L. A. (2016). Postpartum depression: Etiology, treatment and consequences for maternal care. Hormones and Behavior, 77, 153–166.
Centers for Disease Control and Prevention. (2017). Depression among women. Resource document. United States Department of Health & Human Services. https://www.cdc.gov/reproductivehealth/depression/index.htm. Accessed 28 August 2017.
Cheraghi, M., Najafian, M., Amoori, N., Bazargan, A., Cheraghi, M., & Motaghi, M. (2015). Risk factors of postpartum depression in Ramhormoz city, Iran. Neuropsychology/Neuropsychiatria i Neuropsychologia, 10(1), 1–4.
Conway, K. S., & Kennedy, L. D. (2004). Maternal depression and the production of infant health. Southern Economic Journal, 71(2), 260–286.
El-Hachem, C., Rohayem, J., Bou Khalil, R., Richa, S., Kesrouani, A., Gemayel, R., et al. (2014). Early identification of women at risk of postpartum depression using the Edinburgh Postnatal Depression Scale (EPDS) in a sample of Lebanese women. BMC Psychiatry, 14, 242.
Haas, D. M., Till, S. R., & Everetts, D. (2012). Incentives for increasing prenatal care use by women in order to improve maternal and neonatal outcomes. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd009916.
HealthyPeople.Gov. (2017). Healthy People 2020 Maternal, infant, and child health. Resource document. United States Department of Health and Human Services. https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives. Accessed 28 August 2017.
Heberlein, E. C., Picklesimer, A. H., Billings, D. L., Covington-Kolb, S., Farber, N., & Frongillo, E. A. (2016). The comparative effects of group prenatal care on psychosocial outcomes. Archives of Women’s Mental Health, 19(2), 259–269.
Massachusetts Child Psychiatry Access Program (MCPAP) For Moms. (2017). Promoting maternal mental health during and after pregnancy. Resource document. MCPAP for Moms. https://www.mcpapformoms.org/Docs/M4M%20Provider%20Brochure%20V2%201%2020%2017.pdf. Accessed 28 August 2017.
Nothnagle, M., Marchi, K., et al. (2000). Risk factors for late or no prenatal care following Medicaid expansion in California. Maternal and Child Health Journal, 4(4), 251–259.
Olson, R., Garite, T. J., Fishman, A., & Andress, I. F. (2012). Obstetrician/gynecologist hospitalists: Can we improve safety and outcomes for patients and hospitals and improve lifestyle for physicians? American Journal of Obstetrics and Gynecology, 207(2), 81–86.
Reeves, W. C., Strine, T. W., Pratt, L. A., Thompson, W., Ahluwalia, I., Dhingra, S. S., et al. (2011). Mental illness surveillance among adults in the United States. MMWR Surveillance Summaries, 60(3), 1–32.
Ruyak, S. L., Flores-Montoya, A., & Boursaw, B. (2017). Antepartum services and symptoms of postpartum depression in at-risk women. Journal of Obstetric, Gynecologic & Neonatal Nursing, 46(5), 696–708.
Sidebottom, A. C., Hellerstedt, W. L., Harrison, P. A., & Hennrikus, D. (2014). An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Archives of Women’s Mental Health, 17(1), 27–40.
Silverman, M. E., Reichenberg, A., et al. (2017). The risk factors for postpartum depression: A population based study. Depression and Anxiety, 34(2), 178–187.
Sunil, T. S., Spears, W. D., Hook, L., Castillo, J., & Torres, C. (2008). Initiation of and barriers to prenatal care use among low-income women in San Antonio, Texas. Maternal and Child Health Journal, 14(1), 133–140.
Tachibana, Y., Koizumi, T., Takehara, K., Kakee, N., Tsujii, H., Mori, R., et al. (2015). Antenatal risk factors of postpartum depression at 20 weeks gestation in a Japanese sample: Psychosocial perspectives from a cohort study in Tokyo. PLoS ONE, 10(12), e0142410.
United States Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. (2013). Child health USA 2013. Resource document. U.S. Department of Health and Human Services. https://mchb.hrsa.gov/chusa13/dl/pdf/chusa13.pdf. Accessed 28 October 2017.
United States Preventive Services Task Force. (2016). Depression in adults: Screening. Resource document. United States Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/depression-in-adults-screening1. Accessed 28 August 2017.
Veltman, L. (2015). Obstetrics hospitalists: Risk management implications. Obstetrics and Gynecology Clinics of North America, 42(3), 507–517.
Venkatesh, K. K., Nadel, H., Blewett, D., Freeman, M. P., Kaimal, A. J., & Riley, L. E. (2016). Implementation of universal screening for depression during pregnancy: Feasibility and impact on obstetric care. American Journal of Obstetrics and Gynecology, 215(5), 517.e1–517.e8.
Werner, E., Miller, M., Osborne, L. M., Kuzava, S., & Monk, C. (2014). Preventing postpartum depression: Review and recommendations. Archives of Women’s Mental Health, 18(1), 41–60.
Acknowledgements
Jeff Murawsky, Jasmine Greene, and Jennifer Condon for facilitating data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magliarditi, A.T., Lua, L.L., Kelley, M.A. et al. Maternal Depression Scale: Do “Drop-In” Laborist Patients Have Increased Postpartum Screening Risks Compared to Patients with Adequate Prenatal Care?. Matern Child Health J 23, 54–60 (2019). https://doi.org/10.1007/s10995-018-2593-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2593-z