Abstract
Objectives
Fetal alcohol spectrum disorders are more common in disadvantaged populations. Environmental factors, like suboptimal nutrition, may potentiate the developmental effects of prenatal alcohol exposure. To evaluate the impact of micronutrients, including choline, on reduction of effects of exposure, we examined timing and dose of alcohol and effects of nutritional supplementation at two OMNI-Net sites in Western Ukraine that included high and low risk individuals.
Methods
Alcohol-using and nondrinking women were randomized to one of three multivitamin/mineral supplement groups: none, multivitamins/minerals (MVM), and multivitamin/minerals plus choline. Children (N = 367) were tested at 6 months with the Bayley Scales of Infant Development (2nd ED) yielding standard scores for Mental Development Index (MDI), Psychomotor Development Index (PDI) and Behavior.
Results
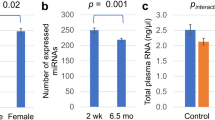
Generalized linear modeling was used: (1) for factorial analysis of effects of alcohol group, multivitamin/minerals, and choline supplementation; and (2) to examine the relationship between amount and timing of alcohol (ounces of absolute alcohol/day [ozAA/day] peri-conception and on average in the second trimester) and MVM supplementation on developmental outcomes while controlling sex, social class, and smoking. MDI was significantly impacted by peri-conceptual alcohol dose (\(\upchi_{(1)}^{2} = 8.54\), p < .001) with more alcohol associated with lower scores and males more negatively affected than females (\(\upchi_{(3)}^{2} = 11.04\), p < .002). Micronutrient supplementation had a protective effect; those receiving supplements performed better (\(\upchi_{(1)}^{2} = 8.03\), p < .005). The PDI motor scores did not differ by group but were affected by peri-conceptual alcohol dose (\(\upchi_{(1)}^{2} = 4.17\), p < .04).
Conclusions for Practice
Multivitamin/mineral supplementation can reduce the negative impact of alcohol use during pregnancy on specific developmental outcomes.

Similar content being viewed by others
References
Riley, E. P., Infante, M. A., & Warren, K. R. (2011). Fetal alcohol spectrum disorders: An overview. Neuropsychology Review, 21(2), 73–80.
Mattson, S. N., Crocker, N., & Nguyen, T. T. (2011). Fetal alcohol spectrum disorders: Neuropsychological and behavioral features. Neuropsychology Review, 21(2), 81–101.
Centers for Disease Control and Prevention (CDC). (2002). Fetal alcohol syndrome—Alaska, Arizona, Colorado, and New York, 1995–1997. Morbidity and Mortality Reports, 51(20), 433–435.
May, P. A., et al. (2014). Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics, 134(5), 855–866.
Jacobson, S. W., et al. (2002). Validity of maternal report of prenatal alcohol, cocaine, and smoking in relation to neurobehavioral outcome. Pediatrics, 109(5), 815–825.
Niclasen, J. (2014). Drinking or not drinking in pregnancy: The multiplicity of confounding influences. Alcohol and Alcoholism, 49(3), 349–355.
Abel, E. L. (1998). Fetal alcohol abuse syndrome. New York, NY: Plenum Press.
Weiss, L. A., & Chambers, C. D. (2013). Associations between multivitamin supplement use and alcohol consumption before pregnancy: Pregnancy risk assessment monitoring system, 2004 to 2008. Alcoholism, Clinical and Experimental Research, 37(9), 1595–1600.
Keen, C. L., et al. (2010). The plausibility of maternal nutritional status being a contributing factor to the risk for fetal alcohol spectrum disorders: The potential influence of zinc status as an example. BioFactors, 36(2), 125–135.
Jiang, X., West, A. A., & Caudill, M. A. (2014). Maternal choline supplementation: A nutritional approach for improving offspring health? Trends in Endocrinology and Metabolism, 25(5), 263–273.
Thomas, J. D., Abou, E. J., & Dominguez, H. D. (2009). Prenatal choline supplementation mitigates the adverse effects of prenatal alcohol exposure on development in rats. Neurotoxicology and Teratology, 31(5), 303–311.
Thomas, J. D., et al. (2010). Prenatal choline supplementation mitigates behavioral alterations associated with prenatal alcohol exposure in rats. Birth Defects Research Part A: Clinical and Molecular Teratology, 88(10), 827–837.
Thomas, J. D., et al. (2000). Neonatal choline supplementation ameliorates the effects of prenatal alcohol exposure on a discrimination learning task in rats. Neurotoxicology and Teratology, 22(5), 703–711.
Strain, J. J., et al. (2013). Choline status and neurodevelopmental outcomes at 5 years of age in the Seychelles Child Development Nutrition Study. British Journal of Nutrition, 110(2), 330–336.
Villamor, E., et al. (2012). Maternal intake of methyl-donor nutrients and child cognition at 3 years of age. Paediatric and Perinatal Epidemiology, 26(4), 328–335.
Cheatham, C. L., et al. (2012). Phosphatidylcholine supplementation in pregnant women consuming moderate-choline diets does not enhance infant cognitive function: a randomized, double-blind, placebo-controlled trial. American Journal of Clinical Nutrition, 96(6), 1465–1472.
anomalies, E.s.o.c. (2014). EUROCAT Prevalence Data Tables: A5—Fetal alcohol syndrome § (per 10,000 births) for the following registries: All Registries, from 2008–2012.
Bakhireva, L. N., et al. (2011). Paternal drinking, intimate relationship quality, and alcohol consumption in pregnant Ukrainian women. Journal of Studies on Alcohol and Drugs, 72(4), 536–544.
Chambers, C. D., et al. (2014). Prevalence and predictors of maternal alcohol consumption in 2 regions of Ukraine. Alcoholism, Clinical and Experimental Research, 38(4), 1012–1019.
Sobell, L. C., & Sobell, M. B. (2000). Alcohol timeline followback (TLFB). In American Psychiatric Association (Ed.), Handbook of psychiatric measures (pp. 477–479). Washington, DC: American Psychiatric Association.
Barr, H. M., & Streissguth, A. P. (2001). Identifying maternal self-reported alcohol use associated with fetal alcohol spectrum disorders. Alcoholism, Clinical and Experimental Research, 25(2), 283–287.
Hollingshead, A. B. (2011). Four factor index of social status. Yale Journal of Sociology, 8, 21–51.
Holm, P. I., et al. (2003). Determination of choline, betaine, and dimethylglycine in plasma by a high-throughput method based on normal-phase chromatography-tandem mass spectrometry. Clinical Chemistry, 49(2), 286–294.
Innis, S. M., & Hasman, D. (2006). Evidence of choline depletion and reduced betaine and dimethylglycine with increased homocysteine in plasma of children with cystic fibrosis. Journal of Nutrition, 136(8), 2226–2231.
Bayley, N. (1993). Bayley scales of infant development (BSID-2). San Antonio, TX: Psychological Corporation.
Moore, T., et al. (2012). Relationship between test scores using the second and third editions of the Bayley Scales in extremely preterm children. Journal of Pediatrics, 160(4), 553–558.
Jones, K. L., et al. (1973). Pattern of malformation in offspring of chronic alcoholic mothers. Lancet, 1(7815), 1267–1271.
Acknowledgments
All or part of this work was done in conjunction with the Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD), which is funded by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Additional information about CIFASD can be found at http://cifasd.org/. Research described in this manuscript was supported by Contract #U01AA014835 funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the NIH Office of Dietary Supplements (ODS). We wish to acknowledge the contribution of: OMNI-Net, Ukraine, Participating families and staff in Rivne and Khmelnytsky, Ukraine.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD, http://cifasd.org/).
Rights and permissions
About this article
Cite this article
Coles, C.D., Kable, J.A., Keen, C.L. et al. Dose and Timing of Prenatal Alcohol Exposure and Maternal Nutritional Supplements: Developmental Effects on 6-Month-Old Infants. Matern Child Health J 19, 2605–2614 (2015). https://doi.org/10.1007/s10995-015-1779-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1779-x