Abstract
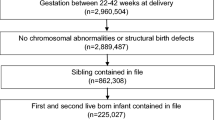
There is growing interest in the application of propensity scores (PS) in epidemiologic studies, especially within the field of reproductive epidemiology. This retrospective cohort study assesses the impact of a short interpregnancy interval (IPI) on preterm birth and compares the results of the conventional logistic regression analysis with analyses utilizing a PS. The study included 96,378 singleton infants from Louisiana birth certificate data (1995–2007). Five regression models designed for methods comparison are presented. Ten percent (10.17 %) of all births were preterm; 26.83 % of births were from a short IPI. The PS-adjusted model produced a more conservative estimate of the exposure variable compared to the conventional logistic regression method (β-coefficient: 0.21 vs. 0.43), as well as a smaller standard error (0.024 vs. 0.028), odds ratio and 95 % confidence intervals [1.15 (1.09, 1.20) vs. 1.23 (1.17, 1.30)]. The inclusion of more covariate and interaction terms in the PS did not change the estimates of the exposure variable. This analysis indicates that PS-adjusted regression may be appropriate for validation of conventional methods in a large dataset with a fairly common outcome. PS’s may be beneficial in producing more precise estimates, especially for models with many confounders and effect modifiers and where conventional adjustment with logistic regression is unsatisfactory. Short intervals between pregnancies are associated with preterm birth in this population, according to either technique. Birth spacing is an issue that women have some control over. Educational interventions, including birth control, should be applied during prenatal visits and following delivery.

Similar content being viewed by others
References
The Henry J. Kaiser Family Foundation. (2008). Statehealthfacts.org. Accessed 10 April 2011.
Conde-Agudelo, A., Rosas-Bermudez, A., & Kafury-Goeta, A. C. (2006). Birth spacing and risk of adverse perinatal outcomes: A meta-analysis. JAMA, 295(15), 1809.
Miller, J. E. (1991). Birth intervals and perinatal health: An investigation of three hypotheses. Family Planning Perspectives, 23, 62.
Winkvist, A., Rasmussen, K. M., & Habicht, J. P. (1992). A new definition of maternal depletion syndrome. American Journal of Public Health, 82, 691.
Smits, L. J., & Essed, G. G. (2001). Short interpregnancy intervals and unfavorable pregnancy outcome: Role of folate depletion. Lancet, 358, 2074.
Scholl, T. O., & Reilly, T. (2000). Anemia, iron, and pregnancy outcome. Journal of Nutrition, 130, 443S–447S.
Rosenbaum, P. R., & Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55.
Grzybowski, M., Clements, E. A., Parsons, L., et al. (2003). Mortality benefit of immediate revasularization of acute ST-segment elevation myocardial infarction in patients with contraindications to thrombolytic therapy—A propensity analysis. JAMA, 290, 1891–1898.
Mehta, R. L., Pascual, M. T., Soroko, S., et al. (2002). Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA, 288, 2547–2553.
Ioannidis, J. A., Galanos, O., Katritsis, D., et al. (2001). Early mortality and morbidity of bilateral versus single internal thoracic artery revascularization: Propensity and risk modeling. Journal of the American College of Cardiology, 37, 521–528.
Newgard, C. D., Hedges, J. R., Arthur, M., et al. (2004). Advanced statistics: The propensity score—A method for estimating treatment effect in observational research. Academic Emergency Medicine, 11(9), 953–960.
Sturmer, T., Joshi, M., Glynn, R. J., et al. (2006). A review of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariable methods. Journal of Clinical Epidemiology, 59, 437–447.
Little, R. J., & Rubin, D. B. (2000). Causal effects in clinical and epidemiological studies via potential outcomes: Concepts and analytical approaches. Annual Review of Public Health, 21, 121–145.
Rubin, D. B. (1997). Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine, 127, 757–763.
Zhu, B. P., Rolfs, R. T., Nangle, B. E., et al. (1999). Effect of the interval between pregnancies on perinatal outcomes. New England Journal of Medicine, 340, 589.
Juntunen, K., Kirkinen, P., & Kauppila, A. (1994). Natural interpregnancy intervals of fertile couples: A longitudinal survey of grand grand multiparous women. Fertility and Sterility, 62, 722.
Brookhart, M. A., Schneeweiss, S., Rothman, K. J., et al. (2006). Variable selection for propensity score models. American Journal of Epidemiology, 163(12), 1149–1156.
Rubin, D. B., & Thomas, N. (2000). Combining propensity score matching with additional adjustments for prognostic covariates. Journal of American Statistical Association, 95(450), 573–585.
Cepeda, M. S., Boston, R., Farrar, J. T., et al. (2003). Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. American Journal of Epidemiology, 158(3), 280–287.
Drake, C. (1993). Effects of misspecification of the propensity score on estimators of treatment effect. Biometrics, 49, 1231–1236.
Shah, B. R., Laupacis, A., Hux, J. E., et al. (2005). Propensity score methods gave similar results to traditional regression modeling in observational studies: A systematic review. J Clinical Epidemiol, 58(6), 550–559.
Baser, O. (2006). Too much ado about propensity score models? Comparing methods of propensity score matching. Value in Health, 9(6), 377–385.
Juhn, Y. J., Qin, R., Urm, S., et al. (2009). The influence of neighborhood environment on the incidence of childhood asthma: A propensity score approach. Journal of Allergy and Clinical Immunology, 125(4), 838–843.
Vinikoor, L. C., Messer, L. C., Laraia, B. A., et al. (2010). Reliability of variables on the North Carolina birth certificate: A comparison with directly queried values from a cohort study. Paediatric and Perinatal Epidemiology, 24, 102–112.
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health And Human Development (T32HD057780). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Howard, E.J., Harville, E., Kissinger, P. et al. The Association Between Short Interpregnancy Interval and Preterm Birth in Louisiana: A Comparison of Methods. Matern Child Health J 17, 933–939 (2013). https://doi.org/10.1007/s10995-012-1073-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1073-0