Abstract
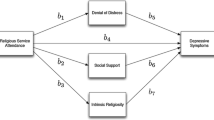
Measures of religiosity are linked to health outcomes, possibly indicating mediating effects of associated psychological and social factors. We examined cross-sectional data from 92,539 postmenopausal participants of the Women’s Health Initiative Observational Study who responded to questions on religious service attendance, psychological characteristics, and social support domains. We present odds ratios from multiple logistic regressions controlling for covariates. Women attending services weekly during the past month, compared with those not attending at all in the past month, were less likely to be depressed [OR = 0.78; CI = 0.74–0.83] or characterized by cynical hostility [OR = 0.94; CI = 0.90–0.98], and more likely to be optimistic [OR = 1.22; CI = 1.17–1.26]. They were also more likely to report overall positive social support [OR = 1.28; CI = 1.24–1.33], as well as social support of four subtypes (emotional/informational support, affection support, tangible support, and positive social interaction), and were less likely to report social strain [OR = 0.91; CI = 0.88–0.94]. However, those attending more or less than weekly were not less likely to be characterized by cynical hostility, nor were they less likely to report social strain, compared to those not attending during the past month.
Similar content being viewed by others
References
Antonucci, T. A., Kahn, R. C., & Akiyama, H. (1989). Psychosocial factors and the response to cancer symptoms. In R. Yancik & J. W. Yates (Eds.), Cancer in the elderly: Approaches to early detection and treatment (pp. 40–52). New York: Springer.
Berkman, L. F., Berkman, C. S., Kasl, S., Freeman, D. H., Le`o, L., Ostfeld, A. M., et al. (1986). Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Epidemiology, 124, 372–388.
Braam, A. W., Van Den Eeden, P., Prince, M. J., Beekman, A. T. F., Kivela, S. L., Lawlor, B. A., et al. (2001). Religion as a cross-cultural determinant of depression in elderly Europeans: Results from the EURODEP collaboration. Psychological Medicine, 31, 803–814.
Burnam, M., Wells, K., Leake, B., & Landsverk, J. (1988). Development of a brief screening instrument for detecting depressive disorders. Medical Care, 26, 775–789.
Casell, J. (1976). The contribution of the social environment to host resistance. American Journal of Epidemiology, 104, 107–123.
Cobb, S. (1976). Social support as a moderator of life stress. Psychosomatic Medicine, 38, 300–314.
Cook, W. W., & Medley, D. M. (1954). Proposed hostility and pharisaic-virtue scales for the MMPI. Journal of Applied Psychology, 38, 414–418.
DeLongis, A., Capreol, M., Holtzman, S., O’Brien, T., & Campbell, J. (2004). Social support and social strain among husbands and wives: A multilevel analysis. Journal of Family Psychology, 18, 470–479.
Exline, J. J. (2002). Stumbling blocks on the religious road: Fractures relationships, nagging vices, and the inner struggle to believe. Psychological Inquiry, 13, 182–189.
Exline, J. J., & Rose, E. (2005). Religious and spiritual struggles. In R. F. Paloutzian & C. L. Park (Eds.), Handbook of the psychology of religion and spirituality (pp. 315–330). New York: Guilford Press.
Fiala, W. E., Bjorck, J. P., & Gorsuch, R. (2002). The religious support scale: Construction, validation, and cross-validation. American Journal of Community Psychology, 30, 761–786.
Gillum, R. F., King, D. E., Obisesan, T. O., & Koenig, H. G. (2008). Frequency of attendance at religious services and mortality in a U.S. national cohort. Annals of Epidemiology, 18, 124–129.
House, J. S., Landis, K. R., & Umberson, D. (1988). Social relationships and health. Science, 241, 540–545.
House, J., Robbins, C., & Metzner, H. (1982). The association of social relationships and activities with mortality: prospective evidence from the Tecumseh Community Health Study. American Journal of Epidemiology, 116, 123–140.
Hughes, J. W., Tomlinson, A., Blumenthal, J. A., Davidson, J., Sketch, M. H., & Watkins, L. L. (2004). Social support and religiosity as coping strategies for anxiety in hospitalized cardiac patients. Annals of Behavioral Medicine, 28, 179–185.
Joshi, S., Kumari, S., & Jain, M. (2008). Religious belief and its relation to psychological well-being. Journal of the Indian Academy of Applied Psychology, 34, 345–354.
Koenig, H. G. (2005). Faith and mental health. West Conshohocken, PA: Templeton Foundation Press.
Koenig, H. G., Hays, J. C., Larson, D. B., George, L. K., Cohen, H. J., McCullough, M. E., et al. (1999). Does religious attendance prolong survival? A six-year follow-up study of 3,968 older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 54A, M370–M376.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health. New York, NY: Oxford University Press.
Krause, N. M. (2008). Aging in the Church: How social relationships affect health. West Conshohocken, Pennsylvania: Templeton Foundation Press.
Krumholz, H. M., Butler, J., Miller, J., Vaccarino, V., Williams, C. S., Mendes De Leon, C. F., et al. (1998). Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation, 97, 958–964.
Lazar, A., & Bjorck, J. P. (2008). Religious support and psychosocial well-being among a religious Jewish population. Mental Health, Religion, and Culture, 11, 403–421.
Lehrer, E. L., & Chiswick, C. U. (1993). Religion as a determinant of marital stability. Demography, 30, 385–403.
Moen, P., Dempster-McClain, D., & Williams, R. M. (1989). Social integration and longevity: An event history analysis of women’s roles and resilience. American Sociological Review, 54, 635–647.
Oman, D., Kurata, J. H., Strawbridge, W. J., & Cohen, R. D. (2002). Religious attendance and cause of death over 31 years. International Journal of Psychiatry in Medicine, 32, 69–89.
Powell, L. H., Shahabi, L., & Thoresen, C. E. (2003). Religion and spirituality: Linkages to physical health. American Psychologist, 58, 36–52.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Rasmussen, H. N., Scheier, M. F., & Greenhouse, J. B. (2009). Optimism and physical health: A meta-analytic review. Annals of Behavioral Medicine, 37, 239–256.
Ray, C. (1992). Positive and negative social support in a chronic illness. Psychological Reports, 71, 977–978.
Robins, L. N., Helzer, J. E., Croughan, J., & Ratcliff, K. S. (1981). National Institute of mental health diagnostic interview schedule: Its history, characteristics, and validity. Archives of General Psychiatry, 38, 381–389.
Rook, K. S. (1990). Parallels in the study of social support and social strain. Journal of Social and Clinical Psychology, 9, 118–132.
Salmoirago-Blotcher, E., Fitchett, G., Ockene, J. K., Schnall, E., Crawford, S., Granek, I., et al. (2011). Religion and healthy lifestyle behaviors among postmenopausal women: The women’s health initiative. Journal of Behavioral Medicine, 34, 360–371.
Scheier, M. F., Carver, C. S., & Bridges, M. W. (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life orientation test. Journal of Personality and Social Psychology, 67, 1063–1078.
Schnall, E., Wassertheil-Smoller, S., Swencionis, C., Zemon, V., Tinker, L., O’Sullivan, M. J., et al. (2010). The relationship between religion and cardiovascular outcomes and all-cause mortality in the women’s health initiative observational study. Psychology & Health, 25, 249–263.
Seeman, T. E. (1996). Social ties and health: The benefits of social integration. Annals of Epidemiology, 6, 442–451.
Sherbourne, S. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science and Medicine, 32, 705–714.
Time Magazine, special issue, February 23, 2009.
Tindle, H. A., Chang, Y. F., Kuller, L. H., Manson, J. E., Robinson, J. G., Rosal, M. C., et al. (2009). Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation, 120, 656–662.
Acknowledgments
Dr. Wassertheil-Smoller had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Grateful acknowledgment is extended to Linzhi Xu and Victor Kamensky for statistical programming. Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller. Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Ross Prentice, Garnet Anderson, Andrea LaCroix, Charles Kooperberg; (Medical Research Labs, Highland Heights, KY) Evan Stein; (University of California at San Francisco, San Francisco, CA) Steven Cummings. Clinical Centers: (Albert Einstein College of Medicine, Bronx, NY) Sylvia Wassertheil-Smoller; (Baylor College of Medicine, Houston, TX) Haleh Sangi-Haghpeykar; (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (Brown University, Providence, RI) Charles B. Eaton; (Emory University, Atlanta, GA) Lawrence S. Phillips; (Fred Hutchinson Cancer Research Center, Seattle, WA) Shirley Beresford; (George Washington University Medical Center, Washington, DC) Lisa Martin; (Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, CA) Rowan Chlebowski; (Kaiser Permanente Center for Health Research, Portland, OR) Erin LeBlanc; (Kaiser Permanente Division of Research, Oakland, CA) Bette Caan; (Medical College of Wisconsin, Milwaukee, WI) Jane Morley Kotchen; (MedStar Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Northwestern University, Chicago/Evanston, IL) Linda Van Horn; (Rush Medical Center, Chicago, IL) Henry Black; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (State University of New York at Stony Brook, Stony Brook, NY) Dorothy Lane; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Alabama at Birmingham, Birmingham, AL) Cora E. Lewis; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of California at Davis, Sacramento, CA) John Robbins; (University of California at Irvine, CA) F. Allan Hubbell; (University of California at Los Angeles, Los Angeles, CA) Lauren Nathan; (University of California at San Diego, LaJolla/Chula Vista, CA) Robert D. Langer; (University of Cincinnati, Cincinnati, OH) Margery Gass; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Hawaii, Honolulu, HI) J. David Curb; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Massachusetts/Fallon Clinic, Worcester, MA) Judith Ockene; (University of Medicine and Dentistry of New Jersey, Newark, NJ) Norman Lasser; (University of Miami, Miami, FL) Mary Jo O’Sullivan; (University of Minnesota, Minneapolis, MN) Karen Margolis; (University of Nevada, Reno, NV) Robert Brunner; (University of North Carolina, Chapel Hill, NC) Gerardo Heiss; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (University of Tennessee Health Science Center, Memphis, TN) Karen C. Johnson; (University of Texas Health Science Center, San Antonio, TX) Robert Brzyski; (University of Wisconsin, Madison, WI) Gloria E. Sarto; (Wake Forest University School of Medicine, Winston-Salem, NC) Mara Vitolins; (Wayne State University School of Medicine/Hutzel Hospital, Detroit, MI) Michael S. Simon. The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schnall, E., Kalkstein, S., Fitchett, G. et al. Psychological and Social Characteristics Associated with Religiosity in Women’s Health Initiative Participants. J Relig Health 51, 20–31 (2012). https://doi.org/10.1007/s10943-011-9549-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-011-9549-6