Abstract
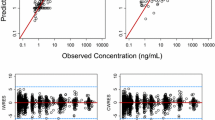
The purpose of this study was to examine the role of dose selection on population pharmacokinetic (PK) parameter estimation using a rapid binding approximation of a target-mediated drug disposition (TMDD) model previously developed for interferon-β (IFN-β). A total of 50 replicate datasets each containing 100 subjects were created using NONMEM®. The study design included IV injection of IFN-β followed by the SC route in a crossover manner, with each dose and route of administration separated by a 1,000 h washout period. Serial plasma PK samples were simulated up to 48 h for all subjects following each dose. Population mean PK parameters were re-estimated in NONMEM® for each simulated dataset using the same TMDD model after including the following doses (MIU/kg): (A) 1, 3 and 10 (original study); (B) 1, 3 and 7; (C) 1, 3 and 5; (D) 1, 3 and 4; (E) 1 and 3; (F) 3 and 10; or (G) 10 MIU/kg only. Bias in the model fit was assessed by calculating the percent prediction error (PE%) for each of the population mean PK parameters relative to the estimates obtained from the fit to the 1, 3, and 10 MIU/kg doses (Case A). Relatively unbiased population mean PK parameter estimates (median PE% <8%) were obtained only when the study design included 1, 3 and a minimum higher dose of 7 MIU/kg. Bias increased for various parameters when the highest dose was less than 7 MIU/kg along with 1 and 3 MIU/kg being the low and intermediate dose levels. An increase in the bias for binding capacity, Rtot, and the equilibrium dissociation constant, K D, was observed as the highest dose included in the dataset was reduced from 5 to 3 MIU/kg (median PE% ranged from −4.71 to −23.9% and −4.76 to −34.6%). Similar increases in the range of median PE% were also observed for other model parameters as the highest dose was reduced from 5 to 3 MIU/kg. Severely biased results were obtained from the study design that included only the 10 MIU/kg dose (Case G) suggesting that it is not sufficient to study just a high dose group. This bias was greatly reduced (median PE% <14%) for all parameters except K D when the 3 and 10 MIU/kg doses were co-modeled (Case F). Plots of the PE% for Rtot and K D versus the molar ratio of maximum dose to Rtot suggest that study designs should evaluate at least one IFN-β dose 3.5- to 4-fold higher than Rtot along with the 1 and 3 MIU/kg dose levels to obtain unbiased population PK parameter estimates. In summary, for the IFN-β model and study design, dose selection influences the ability to generate relatively unbiased population mean TMDD parameter estimates, which is based on maximum dose levels relative to Rtot. This simulation study highlights the role of dose selection in optimal study design strategies for drugs such as IFN-β that exhibit TMDD properties.





Similar content being viewed by others
References
Levy G (1994) Pharmacologic target-mediated drug disposition. Clin Pharmacol Ther 56:248–252
Mager DE (2006) Target-mediated drug disposition and dynamics. Biochem Pharmacol 72:1–10
Mager DE, Jusko WJ (2001) General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn 28:507–532
Gibiansky L, Gibiansky E, Kakkar T, Ma P (2008) Approximations of the target-mediated drug disposition model and identifiability of model parameters. J Pharmacokinet Pharmacodyn 35:573–591
Mager DE, Krzyzanski W (2005) Quasi-equilibrium pharmacokinetic model for drugs exhibiting target-mediated drug disposition. Pharm Res 22:1589–1596
Dutta S, Matsumoto Y, Ebling WF (1996) Is it possible to estimate the parameters of the sigmoid Emax model with truncated data typical of clinical studies? J Pharm Sci 85:232–239
Mager DE, Mascelli MA, Kleiman NS, Fitzgerald DJ, Abernethy DR (2003) Simultaneous modeling of abciximab plasma concentrations and ex vivo pharmacodynamics in patients undergoing coronary angioplasty. J Pharmacol Exp Ther 307:969–976
Abraham AK, Krzyzanski W, Mager DE (2007) Partial derivative-based sensitivity analysis of models describing target-mediated drug disposition. AAPS J 9:E181–E189
Mager DE, Neuteboom B, Efthymiopoulos C, Munafo A, Jusko WJ (2003) Receptor-mediated pharmacokinetics and pharmacodynamics of interferon-beta1a in monkeys. J Pharmacol Exp Ther 306:262–270
Beal SL, Sheiner LB (1989–1998) NONMEM users guides. Icon Development Solutions, Ellicott City, MD
Bonate P (2006) Nonlinear mixed effects models: theory, chap 7. In: Pharmacokinetic-pharmacodynamic modeling and simulation. Springer, New York, pp 205–265
Sheiner LB, Beal SL (1981) Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm 9:503–512
Mager DE, Woo S, Jusko WJ (2009) Scaling pharmacodynamics from in vitro and preclinical animal studies to humans. Drug Metab Pharmacokinet 24:16–24
Zuideveld KP, Van der Graaf PH, Peletier LA, Danhof M (2007) Allometric scaling of pharmacodynamic responses: application to 5-Ht1A receptor mediated responses from rat to man. Pharm Res 24:2031–2039
Acknowledgments
This research was funded, in part, by Grant GM57980 from the National Institutes of Health (D.E.M.) and a post-doctoral fellowship from Amgen, Inc. (A.M.). We wish to thank Dr. John M. Harrold at the University at Buffalo, SUNY for his computational assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Marathe and S. Van Wart contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marathe, A., Van Wart, S. & Mager, D.E. Impact of dose selection on parameter estimation using a rapid binding approximation model of target-mediated drug disposition. J Pharmacokinet Pharmacodyn 38, 223–235 (2011). https://doi.org/10.1007/s10928-010-9190-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-010-9190-0