Abstract
Obstructive sleep apnea (OSA) are linked to the augmented risk of morbidity and mortality. Although polysomnography is considered a well-established method for diagnosing OSA, it suffers the weakness of time consuming and labor intensive, and requires doctors and attending personnel to conduct an overnight evaluation in sleep laboratories with dedicated systems. This study aims at proposing an efficient diagnosis approach for OSA on the basis of anthropometric and questionnaire data. The proposed approach integrates fuzzy set theory and decision tree to predict OSA patterns. A total of 3343 subjects who were referred for clinical suspicion of OSA (eventually 2869 confirmed with OSA and 474 otherwise) were collected, and then classified by the degree of severity. According to an assessment of experiment results on g-means, our proposed method outperforms other methods such as linear regression, decision tree, back propagation neural network, support vector machine, and learning vector quantization. The proposed method is highly viable and capable of detecting the severity of OSA. It can assist doctors in pre-diagnosis of OSA before running the formal PSG test, thereby enabling the more effective use of medical resources.






Similar content being viewed by others
References
Young, T., Palta, M., Dempsey, J., Skatrud, J., Weber, S., and Badr, S., The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 328(17):1230–1235, 1993.
Wright, J., Johns, R., Watt, I., Melville, A., and Sheldon, T., Health effects of obstructive sleep apnea and the effectiveness of continuous positive airway pressure: a systematic review of the research evidence. Br. Med. J. 314:851–860, 1997.
Tan, A. C., and Gilbert, D., Ensemble machine learning on gene expression data for cancer classification. Appl. Bioinform. 2:S75–83, 2003.
Chattopadhyay, S., and Acharya, U. R., A novel mathematical approach to diagnose premenstrual syndrome. J. Med. Syst. 36(4):2177–2186, 2012.
Demsar, J., Zupan, B., Aoki, N., Wall, M. J., Granchi, T. H., and Beck, J. R., Feature mining and predictive model construction from severe trauma patient’s data. Int. J. Med. Inform. 63(1–2):41–50, 2001.
Goker, I., Osman, O., Ozekes, S., Baslo, M. B., Ertas, M., and Ulgen, Y., Classification of juvenile myoclonic epilepsy data acquired through scanning electromyography with machine learning algorithms. J. Med. Syst. 36(5):2705–2711, 2012.
Oztekin, A., Delen, D., and Kong, Z. Y., Predicting the graft survival for heart-lung transplantation patients: an integrated data mining methodology. Int. J. Med. Inform. 78(12):E84–E96, 2009.
Wu, X. D., Kumar, V., Quinlan, J. R., Ghosh, J., Yang, Q., Motoda, H., McLachlan, G. J., Ng, A., Liu, B., Yu, P. S., Zhou, Z. H., Steinbach, M., Hand, D. J., and Steinberg, D., Top 10 algorithms in data mining. Knowl. Inf. Syst. 14(1):1–37, 2008.
Quinlan, J. R., C4.5: programs for machine learning. Morgan Kaufmann, Los Altos, 1993.
De, S. K., Biswas, R., and Roy, A. R., An application of intuitionistic fuzzy sets in medical diagnosis. Fuzzy Sets Syst. 117(2):209–213, 2001.
Naghibi, S., Teshnehlab, M., and Shoorehdeli, M. A., Breast cancer classification based on advanced multi-dimensional fuzzy neural network. J. Med. Syst. 36(5):2713–2720, 2012.
Zadeh, L., A fuzzy sets. Inform. Comput. 8:338–353, 1965.
Desai, A. V., Ellis, E., Wheatley, J. R., and Grunstein, R. R., Fatal distraction: a case of fatal fall-asleep road accidents and their medicolegal outcomes. Med. J. Austral. 178:396–399, 2003.
Barthel, S. W., and Strome, M. S., Obstructive sleep apnea and surgery. Med. Clin. N. Am. 83(1):85–96, 1999.
Hillman, D., Murphy, A., and Pezzullo, L., The economic cost of sleep disorders. Sleep 29(3):299–305, 2006.
Rowley, J. A., Aboussouan, L. S., and Badr, M. S., The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. NCBI 23:929–938, 2000.
Ryan, P. J., Hilton, M. F., Boldy, D. A., Evans, A., Bradbury, S., Sapiano, S., Prowse, K., and Cayton, R. M., Validation of british thoracic society guidelines for the diagnosis of the sleep apnoea/hypopnoea syndrome: Can polysomnography be avoided. Chest 50:972–975, 1995.
Yamashiro, Y., and Kryger, M. H., Nocturnal oximetry: is it a screening tool for sleep disorders. Sleep 18:167–171, 1999.
Rosenthal, L. D., and Diana, D. C., The epworth sleepiness scale in the identification of obstructive sleep apnea. J. Nerv. Ment. Dis. 196:429–431, 2008.
Jacob, S. V., Morielli, A., Mograss, M. A., Ducharme, F. M., Schloss, M. D., and Brouillette, R. T., Home testing for pediatric obstructive sleep apnea syndrome secondary to adenotonsillar hypertrophy. Pediatr. Pulmonol. 20:241–252, 1995.
Gurubhagavatula, I., and Maislin, G., An algorithm to stratify sleep apnea risk in a sleep sisorders clinic population. Am. J. Respir. Crit. Care Med. 170:371–376, 2001.
Huang, S. H., Teng, N. C., Wang, K. J., Chen. K. H., Lee, H. C., and Wang, P. C., Use of oximetry as a screening tool for obstructive sleep apnea: a ca,e study in Taiwan. J. Med. Syst. In press, 2015.
Chawla, N. V., Bowyer, K. W., Hall, L. O., and Kegelmeyer, W. P., SMOTE: Synthetic minor-ity over-sampling technique. J. Artif. Intell. Res. 16:321–357, 2002.
Chawla, N.V., Lazarevic, A., Hall, L.O., and Bowyer, K.W., SMOTE Boost: improving pre-diction of the minority class in boosting. Proc. 7th Europ.Conf. Principles Pract. Knowledge Discov.Database. 107–119, 2003.
Lazarevic, A., Srivastava, J., and Kumar, V., Tutorial: data mining for analysis ofrare events: a case study in security, financial and medical applications. Proc. Pacific-Asia Conf. Knowledge Discov. Data Mining, 2004.
Kubat, M., and Matwin, S., Addressing the curse of imbalanced training set: one-sided selection. Proc. 14th Int Conf. Mach. Learn, (ICML’97), 1997.
Anonymous, Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Rep. Am. Acad. Sleep Med. Task Force. Sleep 22:667–689, 1999.
Stone, M., Cross-validatory choice and assessment of statistica predictions. J. R. Stat. Soc. 36:111–147, 1974.
Geisser, S., The predictive sample reuse method with applications. J. Am. Stat. Assoc. 70:320–328, 1975.
Larson, S., The shrinkage of the coefficient of multiple correlation. J. Educ. Psychol. 22:45–55, 1931.
Mosteller, F., and Turkey, J. W., Data analysis, including statistics. handbook of social psychology. Addison-Wesley, Reading, 1968.
Mosteller, F., and Wallace, D. L., Inference in an authorship problem. J. Am. Stat. Assoc. 58:275–309, 1963.
Zimmermann, H. J., Fuzzy sets, decision making, and expert systems (Vol. 10). Springer Science & Business Media, 2012.
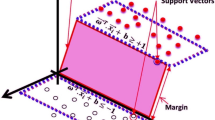
Corinna, C., and Vapnik, V. N., Support vector networks. Mach. Learn. 20:1–25, 1995.
LIBSVM., http://www.csie.ntu.edu.tw/~cjlin/libsvm/, 2015.
See5., https://www.rulequest.com/see5-info.html, 2015.
Pattaraintakorna, P., and Cerconeb, N., Integrating rough set theory and medical applications. Appl. Math. Lett. 21:400–403, 2008.
Vogt, A., and Bared, J. G., Accident models for two-lane rural roads: segments and intersections. Transport. Res. Board Nationl. Acad. 1635:18–29, 1998.
Huang, S. J., and Chiu, N. H., Optimization of analogy weights by genetic algorithm for software effort estimation. Inf. Softw. Technol. 48:1034–1045, 2006.
John, B. D., Linda, M. S., and Brien, P. E., Predicting sleep apnea and excessive day sleepiness in the severely obese. Chest 123:1134–1141, 2003.
Sharma, S. K., Malik, V., Vasudev, C., Banga, A., Mohan, A., Handa, K. K., et al., Prediction of obstructive sleep apnea in patients presenting to a tertiary care center. Sleep Breath 10:147–154, 2006.
The Huffington Post., 8 things that increase sleep apnea risk. Available from Internet:http://www.huffingtonpost.com/2013/10/06/sleep-apnea-risk_n_4018460.html, 2013.
Bixler, E. O., Vgontzas, A. N., Kathy Tyson, T. T. H., and Kales, A., Effects of age on sleep apnea in men. Am. J. Respir. Crit. Care Med. 157(1):144–148, 1998.
Hla, K. M., Young, T. B., Bidwell, T., Palta, M., Skatrud, J. B., and Dempsey, J., Sleep apnea and hypertension-A population-based study. Ann. Intern. Med. 120:382–388, 1994.
Hader, C., Schroeder, A., Hinz, M., Micklefield, G. H., and Rasche, K., Sleep disordered breathing in the elderly: comparison of women and men. J. Physiol. Pharmacol. 56(4):85–91, 2005.
Acknowledgments
This work is partially supported by the National Science Council, R.O.C. (Taiwan), and National Taiwan University of Science and Technology - Taipei Medical University Joint Research Program (TMU-NTUST-102-06 & TMU-NTUST-101-07). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
This study has no conflict of interest to any parties/agencies.
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
About this article
Cite this article
Wang, KJ., Chen, KH., Huang, SH. et al. A Prognosis Tool Based on Fuzzy Anthropometric and Questionnaire Data for Obstructive Sleep Apnea Severity. J Med Syst 40, 110 (2016). https://doi.org/10.1007/s10916-016-0464-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-016-0464-y