Abstract
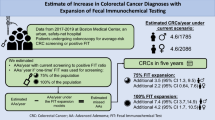
Colorectal cancer (CRC) is a leading cause of cancer-related deaths in the United States. Delays in access to colonoscopy following positive fecal immunochemical test (FIT) contribute to increased CRC incidence and mortality. To evaluate intervals from positive FIT result to receipt of colonoscopy among underserved safety-net populations. We retrospectively evaluated all average CRC risk adults who had positive FIT results from 2012 to 2015 at an ethnically diverse safety-net hospital system. Interval from positive FIT to receipt of colonoscopy was evaluated with Kaplan Meier methods and multivariate Cox proportional hazards models. Among 467 patients with positive FIT (48.4 % men, 39.5 % black, 22.5 % white, 17.4 % Asian, 9.7 % Hispanic, mean age 59.5 ± 9.8 years), mean time from positive FIT to receipt of colonoscopy was 220.5 days (SD 158.5). Compared to men, there was a trend towards longer time from FIT positive to colonoscopy among women (237.1 vs. 198.7 days, p = 0.07). No race/ethnicity-specific disparities in time to colonoscopy were observed. Compared to 2012–2013, there was a 27.2 % reduction in time from FIT positive to colonoscopy in 2014–2015 (173.9 vs. 238.8 days, p < 0.01). Among patients undergoing colonoscopy, 46.3 % had adenomatous polyps, 27.4 % had high risk adenomatous polyps, and 5.6 % had CRC. Among an ethnically diverse safety-net hospital system, improvements in access to colonoscopy after positive FIT were observed. However, patients still waited nearly 6 months from time of positive FIT to undergoing colonoscopy. Delays in receipt of colonoscopy are complex and reflect system-level and individual patient-level barriers.


Similar content being viewed by others
References
Siegel, R. L., Miller, K. D., & Jemal, A. (2016). Cancer statistics, 2016. CA: A Cancer Journal for Clinicians, 66(1), 7–30. doi:10.3322/caac.21332.
Amri R, Bordeianou LG, Sylla P, Berger DL. (2013). Impact of screening colonoscopy on outcomes in colon cancer surgery. JAMA Surgery, 148(8), 747–754. doi:10.1001/jamasurg.2013.8.
FORCE USPST, Bibbins-Domingo, K., Grossman, D. C., et al. (2016). Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA, 315(23), 2564–2575. doi:10.1001/jama.2016.5989.
Knudsen AB, Zauber AG, Rutter CM, et al. (2016). Estimation of benefits, burden, and harms of colorectal cancer screening strategies: Modeling study for the US preventive services task force. JAMA, 315(23), 2595–2609. doi:10.1001/jama.2016.6828.
FORCE USPST (2008). Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine, 149(9), 627–637.
Meester RG, Zauber AG, Doubeni CA, et al. (2016). Consequences of increasing time to colonoscopy examination following positive result from fecal colorectal cancer screening test. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association. doi:10.1016/j.cgh.2016.05.017.
Chubak J, Garcia MP, Burnett-Hartman AN, et al. (2016). Time to colonoscopy after positive fecal blood test in four U.S. Health Care Systems. Cancer epidemiology, biomarkers & prevention: A publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 25(2), 344–350. doi:10.1158/1055-9965.EPI-15-0470.
Gellad ZF, Almirall D, Provenzale D, Fisher DA. (2009). Time from positive screening fecal occult blood test to colonoscopy and risk of neoplasia. Digestive Diseases and Sciences, 54(11), 2497–2502. doi:10.1007/s10620-008-0653-8.
Oluloro A, Petrik AF, Turner A, et al. (2016). Timeliness of colonoscopy after abnormal fecal test results in a safety net practice. Journal of Community Health, 41(4):864–870. doi:10.1007/s10900-016-0165-y.
Millas, S. G., Alawadi, Z. M., Wray, C. J., et al. (2015). Treatment delays of colon cancer in a safety-net hospital system. The Journal of Surgical Research, 198(2), 311–316. doi:10.1016/j.jss.2015.03.078.
Lumpkins, C., Cupertino, P., Young, K., Daley, C., Yeh, H., & Greiner, K. (2013). Racial/ethnic variations in colorectal cancer screening self-efficacy, fatalism and risk perception in a safety-net clinic population: Implications for tailored interventions. Journal of Community Medicine & Health Education, 3.
Jerant, A. F., Fenton, J. J., & Franks, P. (2008). Determinants of racial/ethnic colorectal cancer screening disparities. Archives of Internal Medicine, 168(12), 1317–1324. doi:10.1001/archinte.168.12.1317.
Correia A, Rabeneck L, Baxter NN, et al. (2015). Lack of follow-up colonoscopy after positive FOBT in an organized colorectal cancer screening program is associated with modifiable health care practices. Preventive Medicine, 76, 115–122. doi:10.1016/j.ypmed.2015.03.028.
Etzioni, D. A., Yano, E. M., Rubenstein, L. V., et al. (2006). Measuring the quality of colorectal cancer screening: The importance of follow-up. Diseases of the Colon and Rectum, 49(7), 1002–1010. doi:10.1007/s10350-006-0533-2.
Powell, A. A., Gravely, A. A., Ordin, D. L., Schlosser, J. E., & Partin, M. R. (2009). Timely follow-up of positive fecal occult blood tests strategies associated with improvement. American Journal of Preventive Medicine, 37(2), 87–93. doi:10.1016/j.amepre.2009.05.013.
Ferrat, E., Le Breton, J., Veerabudun, K., et al. (2013). Colorectal cancer screening: Factors associated with colonoscopy after a positive faecal occult blood test. British Journal of Cancer, 109(6), 1437–1444. doi:10.1038/bjc.2013.476.
Gupta S, Halm EA, Rockey DC, et al. (2013). Comparative effectiveness of fecal immunochemical test outreach, colonoscopy outreach, and usual care for boosting colorectal cancer screening among the underserved: A randomized clinical trial. JAMA Internal Medicine, 173(18), 1725–1732. doi:10.1001/jamainternmed.2013.9294.
Humphrey, L. L., Shannon, J., Partin, M. R., O’Malley, J., Chen, Z., & Helfand, M. (2011). Improving the follow-up of positive hemoccult screening tests: An electronic intervention. Journal of General Internal Medicine, 26(7), 691–697. doi:10.1007/s11606-011-1639-3.
Powell, A. A., Nugent, S., Ordin, D. L., Noorbaloochi, S., & Partin, M. R. (2011). Evaluation of a VHA collaborative to improve follow-up after a positive colorectal cancer screening test. Medical Care, 49(10), 897–903. doi:10.1097/MLR.0b013e3182204944.
Singh H, Kadiyala H, Bhagwath G, et al. (2009). Using a multifaceted approach to improve the follow-up of positive fecal occult blood test results. The American Journal of Gastroenterology, 104(4), 942–952. doi:10.1038/ajg.2009.55.
Stock, D., Rabeneck, L., Baxter, N. N., et al. (2015). Mailed participant reminders are associated with improved colonoscopy uptake after a positive FOBT result in Ontario’s ColonCancerCheck program. Implementation Science: IS, 10, 35. doi:10.1186/s13012-015-0226-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors of this manuscript have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Thamarasseril, S., Bhuket, T., Chan, C. et al. The Need for an Integrated Patient Navigation Pathway to Improve Access to Colonoscopy After Positive Fecal Immunochemical Testing: A Safety-Net Hospital Experience. J Community Health 42, 551–557 (2017). https://doi.org/10.1007/s10900-016-0287-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-016-0287-2