Abstract
Continuous monitoring of tissue perfusion in patients with hemodynamic instability remains challenging because of the lack of tools available. Through using urethral photoplethysmography, the urethral perfusion index (uPI) could allow tissue perfusion monitoring through a modified urinary catheter. The first objective of our study was to evaluate the feasibility and safety of the IKORUS UP (Advanced Perfusion Diagnostics, Villeurbanne, France), a new device in the field. The secondary objectives were to evaluate the performance (duration and signal quality) of the IKORUS UP probe and to assess the uPI variations during hemodynamic events during major abdominal surgery. “STEP UP” was a prospective, multicenter, observational study. The inclusion criteria were age 18 years or older with signed informed consent and admitted to intensive care unit (ICU) with hemodynamic instability or high-risk surgical patient. Thirty patients were included in the study, 26 in the operating room, and four in the ICU. Of these patients, 28 were analyzed. For the primary outcome, six (21%) patients had pain scores assessed at insertion of and 22 (79%) at withdrawal of the catheter. The mean EVA score was 1.5 (IQ 1–2) and 0.7 (IQ 0–1), respectively, with the highest score being 3. One (4%) minor urethral bleeding and one (4%) catheter-associated urinary tract infection were reported. The IKORUS UP probe remained in the urethra for an average of 172 h (IQ40–328). The median signal measurement time was 33 h (IQ 5.2–46). The signal quality was recorded as good or excellent for 99% (IQ 82–100) of the insertion duration. The signal quality index was 93% (IQ 87–96) with a signal-to-noise ratio of 26 (IQ 21–36). We observed clinically relevant variations in the uPI over time during hemodynamic events or therapeutic interventions, with a strong cross-correlation with macrohemodynamic variables in some patients, while others did not display macrohemodynamic changes. The IKORUS UP probe was well tolerated and allowed urethral perfusion monitoring. Clinically relevant changes in tissue perfusion could be recorded during the observational period. Trial Registration: (www.clinicaltrials.gov NCT03410069) registered January 25, 2018.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive care unit
- BMI:
-
Body mass index
- SV:
-
Stroke volume
- IQ:
-
Interquartile
- cvAUC:
-
Area under the receiver operating characteristics curve
- RRT:
-
Renal replacement therapy
- PI:
-
Perfusion index
- uPI:
-
Urethral perfusion index
References
Vincent J-L, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34.
Hernández G, Ospina-Tascón GA, Damiani LP, Estenssoro E, Dubin A, Hurtado J, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: the ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA. 2019;321:654.
Dubin A, Henriquez E, Hernández G. Monitoring peripheral perfusion and microcirculation. Curr Opin Crit Care. 2018;24:173–80.
Robert B, Poon MW, Stewart SC. Effect of cardiopulmonary bypass on urethral blood flow as measured by laser doppler flowmetry. J Urol. 1998;160(6):2030–2.
Talja M, Schröder T, Lehtola A, Nuutinen P, Ruutu M, Alfthan O. Blood circulation in the urethra during hypovolemia ? An experimental study. Urol Res. 1986;14(5):267–70. https://doi.org/10.1007/BF00256572.
Toulouse E, Masseguin C, Lafont B, McGurk G, Harbonn A, Roberts JA, et al. French legal approach to clinical research. Anaesth Crit Care Pain Med. 2018;37:607–14.
Lima AP, Beelen P, Bakker J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med. 2002;30:1210–3.
Chen T, Clifford G, Mark R. The effect of signal quality on six cardiac output estimators. Comput Cardiol. 2009;2009:197–200.
Ono M, Arnaoutakis GJ, Fine DM, Brady K, Easley RB, Zheng Y, et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med. 2013;41:464–71.
Brown CH, Neufeld KJ, Tian J, Probert J, LaFlam A, Max L, et al. Effect of targeting mean arterial pressure during cardiopulmonary bypass by monitoring cerebral autoregulation on postsurgical delirium among older patients: a nested randomized clinical trial. JAMA Surg. 2019. https://doi.org/10.1001/jamasurg.2019.1163.
Pasanen L, Holmström L. Scale space multiresolution correlation analysis for time series data. Comput Stat. 2017;32:197–218.
Hollingsworth JM, Rogers MAM, Krein SL, Hickner A, Kuhn L, Cheng A, et al. Determining the noninfectious complications of indwelling urethral catheters: a systematic review and meta-analysis. Ann Intern Med. 2013;159:401.
Saint S, Trautner BW, Fowler KE, Colozzi J, Ratz D, Lescinskas E, et al. A multicenter study of patient-reported infectious and noninfectious complications associated with indwelling urethral catheters. JAMA Intern Med. 2018;178:1078.
Zugail AS, Pinar U, Irani J. Evaluation of pain and catheter-related bladder discomfort relative to balloon volumes of indwelling urinary catheters: a prospective study. Investig Clin Urol. 2019;60:35–9.
Hariri G, Joffre J, Leblanc G, Bonsey M, Lavillegrand J-R, Urbina T, et al. Narrative review: clinical assessment of peripheral tissue perfusion in septic shock. Ann Intensive Care. 2019;9(1):37. https://doi.org/10.1186/s13613-019-0511-1.
Thooft A, Favory R, Salgado D, Taccone FS, Donadello K, De Backer D, et al. Effects of changes in arterial pressure on organ perfusion during septic shock. Crit Care. 2011;15:R222.
Bouattour K, Teboul J-L, Varin L, Vicaut E, Duranteau J. Preload dependence is associated with reduced sublingual microcirculation during major abdominal surgery. Anesthesiology. 2019;130:541–9.
Asfar P, Meziani F, Hamel J-F, Grelon F, Megarbane B, Anguel N, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370:1583–93.
LeDoux D, Astiz ME, Carpati CM, Rackow EC. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med. 2000;28:2729–32.
Bourgoin A, Leone M, Delmas A, Garnier F, Albanèse J, Martin C. Increasing mean arterial pressure in patients with septic shock: effects on oxygen variables and renal function. Crit Care Med. 2005;33:780–6.
Mayevsky A, Blum Y, Dekel N, Deutsch A, Halfon R, Kremer S, et al. The CritiView: a new fiber optic based optical device for the assessment of tissue vitality. In: Gannot I, editor. Optical fibers and sensors for medical diagnostics and treatment applications. San Jose: SPIE; 2006. p. 60830Z.
Mayevsky A, Tolmasov M, Mandelbaum M. Perioperative cardiovascular evaluation of patients oxygen balance and tissue metabolic score (TMS). Am J Cardiovasc Thorac Surg. 2018;3:1–17.
Galvin EM, Niehof S, Verbrugge SJ, Maissan I, Jahn A, Klein J, et al. Peripheral flow index is a reliable and early indicator of regional block success. Anesth Analg. 2006;103:239–43.
Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, et al. Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia. Acta Anaesthesiol Scand. 2009;53:1018–26.
van Genderen ME, Bartels SA, Lima A, Bezemer R, Ince C, Bakker J, et al. Peripheral perfusion index as an early predictor for central hypovolemia in awake healthy volunteers. Anesth Analg. 2013;116:351–6.
De Backer D, Foulon P. Minimizing catecholamines and optimizing perfusion. Crit Care Lond Engl. 2019;23:149.
Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care Lond Engl. 2015;19(Suppl 3):S8.
Trzeciak S, McCoy JV, Phillip Dellinger R, Arnold RC, Rizzuto M, Abate NL, et al. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med. 2008;34:2210–7.
Leone M, Blidi S, Antonini F, Meyssignac B, Bordon S, Garcin F, et al. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology. 2009;111:366–71.
Coutrot M, Joachim J, Dépret F, Millasseau S, Nougué H, Matéo J, et al. Non-invasive continuous detection of arterial hypotension during induction of anaesthesia using a photoplethysmographic signal: proof of concept. Br J Anaesth. 2019;122(5):605–12.
Edul VSK, Ince C, Navarro N, Previgliano L, Risso-Vazquez A, Rubatto PN, et al. Dissociation between sublingual and gut microcirculation in the response to a fluid challenge in postoperative patients with abdominal sepsis. Ann Intensive Care. 2014;4(1):39.
On behalf of the Cardiovascular Dynamics Section of the ESICM, Ince C, Boerma EC, Cecconi M, De Backer D, Shapiro NI, et al. Second consensus on the assessment of sublingual microcirculation in critically ill patients: results from a task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2018;44(3):281–99. https://doi.org/10.1007/s00134-018-5070-7.
Clavijo JA, van Bastelaar J, Pinsky MR, Puyana JC, Mayevsky A. Minimally invasive real time monitoring of mitochondrial NADH and tissue blood flow in the urethral wall during hemorrhage and resuscitation. Med Sci Monit Int Med J Exp Clin Res. 2008;14:BR175–82.
Evans RG, Smith JA, Wright C, Gardiner BS, Smith DW, Cochrane AD. Urinary oxygen tension: a clinical window on the health of the renal medulla? Am J Physiol-Regul Integr Comp Physiol. 2014;306:R45–50.
Clavijo-Alvarez JA, Sims CA, Menconi M, Shim I, Ochoa C, Puyana JC. Bladder mucosa pH and Pco2 as a minimally invasive monitor of hemorrhagic shock and resuscitation. J Trauma Inj Infect Crit Care. 2004;57:1199–210.
Dubin A, Pozo MO, Edul VSK, Murias G, Canales HS, Barán M, et al. Urinary bladder partial carbon dioxide tension during hemorrhagic shock and reperfusion: an observational study. Crit Care Lond Engl. 2005;9:R556–61.
Morgaz J, Espigares-Rodríguez L, Muñoz-Rascón P, Navarrete R, Fernández-Sarmiento JA, del Granados Machuca MD. Evaluation of gastric and bladder tonometry as indicators of tissue perfusion in induced hypotension in dogs: gastric and vesical tonometry in dogs. J Vet Emerg Crit Care. 2017;27:532–8.
Funding
The project was carried out with the support of the Société Française d’Anesthésie Réanimation research contract SFAR 2018.
Author information
Authors and Affiliations
Contributions
FD collected data, performed the analysis and interpretation of the data, and drafted the manuscript. ML collected data, performed the analysis and interpretation of the data, and drafted the manuscript. GD collected data, performed the analysis and interpretation of the data, and drafted the manuscript. EF collected data, performed the analysis and interpretation of the data, and drafted the manuscript. MM collected data, performed the analysis and interpretation of the data, and drafted the manuscript. ML collected data, performed the analysis and interpretation of the data, and drafted the manuscript.BA designed the study, collected data, performed the analysis and interpretation of the data, and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
FDépret: research grants from the French Ministry of Health and SFAR (société française d’anesthésie réanimation). M Leone: MSD, Pfizer, Octapharma, Aspen, Orion (Lecturer) Aguettant, Amomed (Consultant). Gary Duclos: nothing to declare. Emmanuel Futier: research grants from the French Ministry of Health, consulting fees from Drager Medical, General Electric Healthcare, Edwards Lifesciences, and Orion Pharma, along with lecture fees from Fesenius Kabi, Fisher and Paykel Healthcare, and Getinge. Maxime Montagne: nothing to declare. Matthieu Legrand: research grants from the French Ministry of Health, research support from Sphingotec, lecture fees from Baxter and Fresenius, consulting fees from Novartis. Bernard Allaouchiche: Consulting fees from APD. Consultant for APPD.
Ethical approval
All patients signed an informed consent, and the study was approved by favorable opinion from an ethics committee (CPP Ouest V); the study was registered on the website www.clinicaltrials.gov under the identifier NCT03410069 and recorded under the ID-RCB number: 2017-A03466-47.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10877_2019_414_MOESM1_ESM.jpg
Supplementary material 1 (JPEG 24 kb). Supplementary data Fig. 1: Patient repartition depending on the proportion correlation time between the SV and uPI. SV: stroke volume
10877_2019_414_MOESM2_ESM.jpg
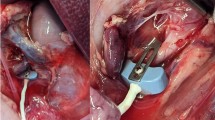
Supplementary material 2 (JPEG 65 kb). Supplementary data Fig. 2: Panel A (upper panel): IKORUS Perfusion Monitor. Panel B (middle panel): UP-distal probe variant, Panel C (lower panel): UP-proximal probe variant, The body of the probe (1), PPG sensor (2) and connector (3)
10877_2019_414_MOESM3_ESM.png
Supplementary material 3 (PNG 152 kb). Supplementary data Fig. 3: Example of a patient with a high correlation between the uPI and SV. uPI: urethral perfusion index; SVI: stroke volume indexed. Patient no 205 was a 60-year-old female with history of caustic ingestion one month before surgery. She was admitted to the OR for coloplasty because of esophagus stenosis. Invasive arterial pressure and cardiac output were recorded with EV1000 Flotrac system (Edwards Life Science, Irvine, California, United States). We observed a positive correlation between the uPI and SV (uPI = -4.4 + 0.3 × SVI, r2 = 0.84)
10877_2019_414_MOESM4_ESM.png
Supplementary material 4 (PNG 114 kb). Supplementary data Fig. 4: Examples of a patient with a high positive correlation between the uPI and MAP. Patient no 105 was a 61-year-old female with no noticeable medical history except an ovarian carcinoma with peritoneal carcinosis. She was admitted to the operative room for a cytoreduction plus intraperitoneal chemotherapy. Invasive arterial pressure and cardiac output were recorded with EV1000 Flotrac system (Edwards Life Science, Irvine, California, United States). In this case, we observed a positive correlation between the MAP and uPI (uPI = -0.22 + 0.044 x MAP, r2 = 0.966). uPI: urethral perfusion index; MAP: mean arterial pressure; SVI: stroke volume indexed
10877_2019_414_MOESM5_ESM.png
Supplementary material 5 (PNG 106 kb). Supplementary data Fig. 5: Example of a patient with a high negative correlation between the uPI and MAP. Patient no 403 was a 63-year-old female with a history of hypertension, obesity, and peritoneal pseudomyxoma. She was admitted in the OR for a surgery of cytoreduction plus intraperitoneal chemotherapy. In this case, we observed a negative correlation between the MAP and uPI (PI = 35 + -0.28 x MAP, r2 = 0.77). uPI: urethral perfusion index; MAP: mean arterial pressure; SVI: stroke volume indexed
Rights and permissions
About this article
Cite this article
Dépret, F., Leone, M., Duclos, G. et al. Monitoring tissue perfusion: a pilot clinical feasibility and safety study of a urethral photoplethysmography-derived perfusion device in high-risk patients. J Clin Monit Comput 34, 961–969 (2020). https://doi.org/10.1007/s10877-019-00414-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00414-9