Abstract
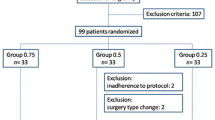
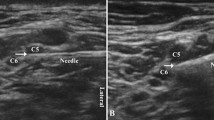
This randomized double-blind controlled trial compared the block characteristics of three low-dose local anesthetics at different roots in an ultrasound-guided interscalene block, using thermal quantitative sensory testing for assessing the functioning of cutaneous small nerve fibres. A total of 37 adults scheduled to undergo shoulder arthroscopy were randomized to receive 5 mL of either 0.5% levobupivacaine with and without epinephrine 1/200,000 or 0.75% ropivacaine in a single-shot interscalene block. Thermal quantitative sensory testing was performed in the C4, C5, C6 and C7 dermatomes. Detection thresholds for cold/warm sensation and cold/heat pain were measured before and at 30 min, 6, 10 and 24 h after infiltration around C5. The need for rescue medication was recorded. No significant differences between groups were found for any sensation (lowest P = 0.28). At 6 h, the largest differences in sensory thresholds were observed for the C5 dermatome. The increase in thresholds were less in C4 and C6 and minimal in C7 for all sensations. The analgesic effect lasted the longest in C5 (time × location mixed model P < 0.001 for all sensory tests). The time to rescue analgesia was significantly shorter with 0.75% ropivacaine (P = 0.02). The quantitative sensory findings showed no difference in intensity between the local anesthetics tested. A decrease in block intensity, with minimal changes in pain detection thresholds, was observed in the roots adjacent to C5, with the lowest block intensity in C7. A clinically relevant shorter duration was found with 0.75% ropivacaine compared to the other groups. Trial registration NCT 02691442.



Similar content being viewed by others
Availability of data
Data sharing: original, de-identified, data are available upon request.
References
Kapral S, Greher M, Huber G, Willschke H, Kettner S, Kdolsky R, Marhofer P. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33(3):253–8.
Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38(4):289–97.
Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009;34(5):498–502.
Plante T, Rontes O, Bloc S, Delbos A. Spread of local anesthetic during an ultrasound-guided interscalene block: does the injection site influence diffusion? Acta Anaesthesiol Scand. 2011;55(6):664–9.
Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996(330):202–7.
Bonica JJ. Importance of effective pain control. Acta Anaesthesiol Scand Suppl. 1987;85:1–16.
Cousins MJ: John J. Bonica distinguished lecture. Acute pain and the injury response: immediate and prolonged effects. Reg Anesth. 1989;14(4):162–79.
Bonica JJ. Postoperative pain. 2 ed. Vol. 1. Philadelphia: Lea & Febiger; 1990.
Bonica JJ. Anatomic and physiologic basis of nociception. 2 ed. Vol. 1. Philadelphia: Lea & Febiger; 1990.
Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001;95(4):875–80.
Gautier P, Vandepitte C, Ramquet C, DeCoopman M, Xu D, Hadzic A. The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg. 2011;113(4):951–5.
McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, Holtby RM, McCartney CJ. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth. 2011;106(1):124–30.
Sermeus LA, Hans GH, Schepens T, Bosserez NM, Breebaart MB, Smitz CJ, Vercauteren MP. Thermal quantitative sensory testing to assess the sensory effects of three local anesthetic solutions in a randomized trial of interscalene blockade for shoulder surgery. Can J Anaesth. 2016;63(1):46–55.
Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A, Binder A, Birbaumer N, Birklein F, Botefur IC, et al. Quantitative sensory testing in the German research network on neuropathic pain (DFNS): standardized protocol and reference values. Pain. 2006;123(3):231–43.
Heldestad V, Linder J, Sellersjo L, Nordh E. Reproducibility and influence of test modality order on thermal perception and thermal pain thresholds in quantitative sensory testing. Clin Neurophysiol. 2010;121(11):1878–85.
Lauria G. Small fibre neuropathies. Curr Opin Neurol. 2005;18:591–7.
Grone E, Crispin A, Fleckenstein J, Irnich D, Treede RD, Lang PM. Test order of quantitative sensory testing facilitates mechanical hyperalgesia in healthy volunteers. J Pain. 2012;13(1):73–80.
Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: are they clinically different? Best Pract Res Clin Anaesthesiol. 2005;19(2):247–68.
Casati A, Borghi B, Fanelli G, Cerchierini E, Santorsola R, Sassoli V, Grispigni C, Torri G. A double-blinded, randomized comparison of either 0.5% levobupivacaine or 0.5% ropivacaine for sciatic nerve block. Anesth Analg. 2002;94(4):987–90. (table of contents).
Casati A, Borghi B, Fanelli G, Montone N, Rotini R, Fraschini G, Vinciguerra F, Torri G, Chelly J. Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: a randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg. 2003;96(1):253–9. (table of contents).
Eroglu A, Uzunlar H, Sener M, Akinturk Y, Erciyes N. A clinical comparison of equal concentration and volume of ropivacaine and bupivacaine for interscalene brachial plexus anesthesia and analgesia in shoulder surgery. Reg Anesth Pain Med. 2004;29(6):539–43.
Kaur A, Singh RB, Tripathi RK, Choubey S. Comparision between bupivacaine and ropivacaine in patients undergoing forearm surgeries under axillary brachial plexus block: a prospective randomized study. J Clin Diagn Res. 2015;9(1):UC01–6.
Borgeat A, Ekatodramis G, Blumenthal S. Interscalene brachial plexus anesthesia with ropivacaine 5 mg/mL and bupivacaine 5 mg/mL: effects on electrocardiogram. Reg Anesth Pain Med. 2004;29(6):557–63.
Magerl W, Krumova EK, Baron R, Tolle T, Treede RD, Maier C. Reference data for quantitative sensory testing (QST): refined stratification for age and a novel method for statistical comparison of group data. Pain. 2010;151(3):598–605.
Burlacu CL, Buggy DJ. Update on local anesthetics: focus on levobupivacaine. Ther Clin Risk Manag. 2008;4(2):381–92.
Yarnitsky D, Sprecher E. Thermal testing: normative data and repeatability for various test algorithms. J Neurol Sci. 1994;125(1):39–45.
Bromage PR. Mechanism of action. Philadelphia: WB Saunders; 1978:119–59.
Szerb JJ, Greenberg JL, Kwofie MK, Baldridge WH, Sandeski RE, Zhou J, Wong K. Histological confirmation of needle tip position during ultrasound-guided interscalene block: a randomized comparison between the intraplexus and the periplexus approach. Can J Anaesth. 2015;62(12):1295–302.
Spence BC, Beach ML, Gallagher JD, Sites BD. Ultrasound-guided interscalene blocks: understanding where to inject the local anaesthetic. Anaesthesia. 2011;66(6):509–14.
Kreidler SM, Muller KE, Grunwald GK, Ringham BM, Coker-Dukowitz ZT, Sakhadeo UR, Baron AE, Glueck DH. GLIMMPSE: online power computation for linear models with and without a Baseline Covariate. J Stat Softw 2013, 54(10).
Thiebaut R, Jacqmin-Gadda H. Mixed models for longitudinal left-censored repeated measures. Comput Methods Programs Biomed. 2004;74(3):255–60.
Hansson P, Backonja M, Bouhassira D. Usefulness and limitations of quantitative sensory testing: clinical and research application in neuropathic pain states. Pain. 2007;129(3):256–9.
Reinhart DJ, Wang W, Stagg KS, Walker KG, Bailey PL, Walker EB, Zaugg SE. Postoperative analgesia after peripheral nerve block for podiatric surgery: clinical efficacy and chemical stability of lidocaine alone versus lidocaine plus clonidine. Anesth Analg. 1996;83(4):760–5.
Defrin RO, Ohry A, Blumen N, Urca G. Sensory determinants of pain. Brain. 2002;125:501–10.
Wilder-Smith OHT, Crul E, Ben JP, Arendt-Nielsen L. Quantitative sensory testing and human surgery: effects of analgesic management on postoperative neuroplasticity. Anesthesiology. 2003;98:1214–22.
Smet I, Vlaminck E, Vercauteren M. Randomized controlled trial of patient-controlled epidural analgesia after orthopaedic surgery with sufentanil and ropivacaine 0.165% or levobupivacaine 0.125%. Br J Anaesth. 2008;100(1):99–103.
Burckett-St Laurent D, Chan V, Chin KJ. Refining the ultrasound-guided interscalene brachial plexus block: the superior trunk approach. Can J Anaesth. 2014;61(12):1098–102.
Ivani G. Ropivacaine: is it time for children? Paediatr Anaesth. 2002;12(5):383–7.
Goveia CS, Magalhaes E. Ropivacaine in peribulbar anesthesia - vasoconstrictive properties. Rev Bras Anestesiol. 2010;60(5):495–512.
Soetens FM, Soetens MA, Vercauteren MP. Levobupivacaine-sufentanil with or without epinephrine during epidural labor analgesia. Anesth Analg. 2006;103(1):182–6. (table of contents).
Sinnott CJ, Cogswell IL, Johnson A, Strichartz GR. On the mechanism by which epinephrine potentiates lidocaine’s peripheral nerve block. Anesthesiology. 2003;98(1):181–8.
Rosenberg PH, Heinonen E. Differential sensitivity of A and C nerve fibres to long-acting amide local anaesthetics. Br J Anaesth. 1983;55(2):163–7.
Niemi G. Advantages and disadvantages of adrenaline in regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19(2):229–45.
Wittes J. Sample size calculations for randomized controlled trials. Epidemiol Rev. 2002;24(1):39–53.
Moloney NA, Hall TM, O’Sullivan TC, Doody CM. Reliability of thermal quantitative sensory testing of the hand in a cohort of young, healthy adults. Muscle Nerve. 2011;44(4):547–52.
Backonja MM, Walk D, Edwards RR, Sehgal N, Moeller-Bertram T, Wasan A, Irving G, Argoff C, Wallace M. Quantitative sensory testing in measurement of neuropathic pain phenomena and other sensory abnormalities. Clin J Pain. 2009;25(7):641–7.
Acknowledgements
Assistance with the study: Mrs. Annick Leroy for reviewing the statistical analysis. This manuscript has been edited by American Journal Experts.
Funding
Financial support and sponsorship: resources were provided from the Department of Anesthesiology only.
Author information
Authors and Affiliations
Contributions
LS conceived the study, participated in its design and coordination, performed the blocks, analyzed the QST results and wrote the manuscript. GH helped conceive the study design, performed the QST interpretation, helped in the analysis of the data, assisted in manuscript drafting and edited the various versions of the manuscript. TS helped in the analysis of the data, assisted in writing and reviewed the manuscript. SM assisted in writing and reviewing the manuscript. KW performed the statistical analysis. MB helped conceive the study design and performed a critical reading. CS performed QST testing and collected data. MV critically read the various versions of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1
: All mixed model values of nerve blockage effects over time, per dermatome and per study group. Statistical methodology and P-values of the within/between-subject effects in the censored mixed effects model. (DOCX 73 KB)
Additional file 2
: Graphics of all neurosensitive/nociceptive responses. Time course of the neurosensory changes in detection thresholds for all sensations, Cold & Warm Sensation and Cold & Heat Pain (Temperature in °C) in the different dermatomes (C4, C5, C6, C7) for the 3 anesthetic solutions (0.5%Bup, 0.5%BupEpi, 0.75%Rop) measured with quantitative sensory testing (mean, standard deviation). The increases in thresholds are significant as compared to pre-injection thresholds. Detection thresholds between the 3 local anesthetics did not differ significantly. (DOCX 436 KB)
Rights and permissions
About this article
Cite this article
Sermeus, L.A., Schepens, T., Hans, G.H. et al. A low dose of three local anesthetic solutions for interscalene blockade tested by thermal quantitative sensory testing: a randomized controlled trial. J Clin Monit Comput 33, 307–316 (2019). https://doi.org/10.1007/s10877-018-0150-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0150-3