Abstract
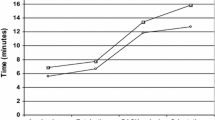
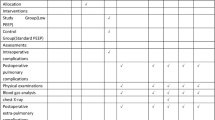
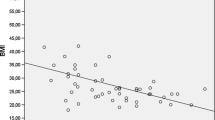
Obesity affects respiratory and hemodynamic function in anesthetized patients. The aim of this study was to evaluate the influence of the body mass index (BMI) on pulmonary changes in a permanent 45° steep Trendelenburg position (STP) during robotic-assisted laparoscopic prostatectomy (RALP). 51 patients undergoing RALP under standardized anesthesia were included. Perioperative pulmonary function and oxygenation were measured in awake patients (T0), 20 min after the induction of anesthesia (T1), after insufflation of the abdomen in supine position (T2), after 30 min in STP (T3), when controlling Santorini’s plexus in STP (T4), before awakening while supine (T5), and after 45 min in the recovery room (T6). Patient-specific and time-dependent factor on ventilation and predicted peak inspiratory pressure (PIP), driving pressure (Pdriv) and lung compliance (LC) in a linear regression model were calculated. PIP and Pdriv increased significantly after induction of capnoperitoneum (T2–4) (p < 0.0001). In univariate mixed effects models, BMI was found to be a significant predictor for PIP and Pdriv increase and LC decrease. Obese patients a BMI > 31 kg/m2 reached critical PIP values ≥ 35 cmH2O. Postoperative oxygenation represented by the PaO2/FiO2 ratio was significantly decreased compared to T0 (p < 0.0001). Obesity in combination with STP and capnoperitoneum during RALP has a profound effect on pulmonary function. Increased PIP and Pdriv and decreased LC are directly correlated with a high BMI. Changes in PIP, Pdriv and LC during RALP may be predicted in relation to patient’s BMI for consideration in the preoperative setting. Trial registration number Z-2014-0387-6. Registered on 8 July 2014.



Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesia
- BE:
-
Base excess
- BMI:
-
Body mass index
- etCO2 :
-
End tidal CO2
- FiO2 :
-
Inspiratory fraction of oxygen
- LC:
-
Lung compliance
- MAP:
-
Mean arterial blood pressure
- MV:
-
Minute ventilation
- PaCO2 :
-
Partial arterial carbon dioxide fraction
- PaO2 :
-
Partial arterial oxygen fraction
- Pdriv :
-
Driving pressure
- PEEP:
-
Positive end-expiratory pressure
- PIP:
-
Peak inspiratory pressure
- RALP:
-
Robotic-assisted laparoscopic prostatectomy
- STP:
-
Steep Trendelenburg position
- TIVA:
-
Total intravenous anesthesia
- TOF:
-
Train-of-four
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2009;55:1037–63.
Porpiglia F, Morra I, Lucci Chiarissi M, Manfredi M, Mele F, Grande S, et al. Randomised controlled trial comparing laparoscopic and robot-assisted radical prostatectomy. Eur Urol. 2013;63:606–14.
Novara G, Ficarra V, Rosen RC, Artibani W, Costello A, Eastham JA, et al. Systematic review and meta-analysis of perioperative outcomes and complications after robot-assisted radical prostatectomy. Eur Urol. 2012;62:431–52.
Gainsburg DM. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012;78:596–604.
Consultation on Obesity. Obesity: preventing and managing the global epidemic: report of a WHO consultation. Geneva: WHO; 2000.
Mensink GBM, Schienkiewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. Ubergewicht und Adipositas in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:786–94.
Schmidt AM. The growing problem of obesity: mechanisms, consequences, and therapeutic approaches. Arterioscler Thromb Vasc Biol. 2015;35:e19–23.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38.
Rodriguez C, Patel AV, Calle EE, Jacobs EJ, Chao A, Thun MJ. Body mass index, height, and prostate cancer mortality in two large cohorts of adult men in the United States. Cancer Epidemiol Biomark Prev. 2001;10:345–53.
MacInnis RJ, English DR. Body size and composition and prostate cancer risk: systematic review and meta-regression analysis. Cancer Causes Control. 2006;17:989–1003.
Pelosi P, Croci M, Ravagnan I, Vicardi P, Gattinoni L. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest 1996;109:144–51.
Mandal S, Hart N. Respiratory complications of obesity. Clin Med. 2012;12:75–8.
Melo LC, Silva, MAMd, Calles ACdN. Obesity and lung function: a systematic review. Einstein. 2014;12:120–5.
Gabrielsen A-M, Lund MB, Kongerud J, Viken KE, Røislien J, Hjelmesæth J. The relationship between anthropometric measures, blood gases, and lung function in morbidly obese white subjects. Obes Surg. 2011;21:485–91.
Hodgson LE, Murphy PB, Hart N. Respiratory management of the obese patient undergoing surgery. J Thorac Dis. 2015;7:943–52.
Pelosi P, Croci M, Ravagnan I, Tredici S, Pedoto A, Lissoni A, Gattinoni L. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87:654–60.
Meininger D, Westphal K, Bremerich DH, Runkel H, Probst M, Zwissler B, Byhahn C. Effects of posture and prolonged pneumoperitoneum on hemodynamic parameters during laparoscopy. World J Surg. 2008;32:1400–5.
Hanberger H, Walther S, Leone M, Barie PS, Rello J, Lipman J, et al. Increased mortality associated with methicillin-resistant Staphylococcus aureus (MRSA) infection in the intensive care unit: results from the EPIC II study. Int J Antimicrob Agents. 2011;38:331–5.
Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31:922–6.
Prost N de, Ricard J-D, Saumon G, Dreyfuss D. Ventilator-induced lung injury: historical perspectives and clinical implications. Ann Intensive Care. 2011;1:28.
Holm BA, Finkelstein JN, Notter RH, editors. Lung injury: mechanisms, pathophysiology, and therapy. Boca Raton: Taylor & Francis; 2005.
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4:272–80.
Ladha K, Vidal Melo MF, McLean DJ, Wanderer JP, Grabitz SD, Kurth T, Eikermann M. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ. 2015;351:h3646.
Blecha S, Harth M, Schlachetzki F, Zeman F, Blecha C, Flora P, et al. Changes in intraocular pressure and optic nerve sheath diameter in patients undergoing robotic-assisted laparoscopic prostatectomy in steep 45 degrees Trendelenburg position. BMC Anesthesiol. 2017;17:40.
Kilic OF, Borgers A, Kohne W, Musch M, Kropfl D, Groeben H. Effects of steep Trendelenburg position for robotic-assisted prostatectomies on intra- and extrathoracic airways in patients with or without chronic obstructive pulmonary disease. Br J Anaesth. 2014;114:70–6.
Lestar M, Gunnarsson L, Lagerstrand L, Wiklund P, Odeberg-Wernerman S. Hemodynamic perturbations during robot-assisted laparoscopic radical prostatectomy in 45 degrees Trendelenburg position. Anesth Analg. 2011;113:1069–75.
Kalmar AF, Foubert L, Hendrickx JFA, Mottrie A, Absalom A, Mortier EP, Struys MMRF. Influence of steep Trendelenburg position and CO(2) pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433–9.
Suh MK, Seong KW, Jung SH, Kim SS. The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol. 2010;59:329–34.
Kadono Y, Yaegashi H, Machioka K, Ueno S, Miwa S, Maeda Y, et al. Cardiovascular and respiratory effects of the degree of head-down angle during robot-assisted laparoscopic radical prostatectomy. Int J Med Robot. 2013;9:17–22.
Nestler C, Simon P, Petroff D, Hammermüller S, Kamrath D, Wolf S, et al. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth. 2017;119:1194–205.
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–55.
Hemmes SNT, Gama de Abreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384:495–503.
Bluth T, Teichmann R, Kiss T, Bobek I, Canet J, Cinnella G, et al. Protective intraoperative ventilation with higher versus lower levels of positive end-expiratory pressure in obese patients (PROBESE): study protocol for a randomized controlled trial. Trials. 2017;18:202.
Tomescu DR, Popescu M, Dima SO, Bacalbasa N, Bubenek-Turconi S. Obesity is associated with decreased lung compliance and hypercapnia during robotic assisted surgery. J Clin Monit Comput. 2017;31:85–92.
Wiltz AL, Shikanov S, Eggener SE, Katz MH, Thong AE, Steinberg GD, et al. Robotic radical prostatectomy in overweight and obese patients: oncological and validated-functional outcomes. Urology. 2009;73:316–22.
Mikhail AA, Stockton BR, Orvieto MA, Chien GW, Gong EM, Zorn KC, et al. Robotic-assisted laparoscopic prostatectomy in overweight and obese patients. Urology. 2006;67:774–9.
Jaber S, Delay J-M, Chanques G, Sebbane M, Jacquet E, Souche B, et al. Outcomes of patients with acute respiratory failure after abdominal surgery treated with noninvasive positive pressure ventilation. Chest 2005;128:2688–95.
de Llano LAP, Golpe R, Piquer MO, Racamonde AV, Caruncho MV, Muinelos OC, Carro CA. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest 2005;128:587–94.
Slutsky AS. Lung injury caused by mechanical ventilation. Chest 1999;116:9S–15S.
Weg JG, Anzueto A, Balk RA, Wiedemann HP, Pattishall EN, Schork MA, Wagner LA. The relation of pneumothorax and other air leaks to mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:341–6.
Danic MJ, Chow M, Alexander G, Bhandari A, Menon M, Brown M. Anesthesia considerations for robotic-assisted laparoscopic prostatectomy: a review of 1,500 cases. J Robot Surg. 2007;1:119–23.
Phong SVN, Koh LKD. Anaesthesia for robotic-assisted radical prostatectomy: considerations for laparoscopy in the Trendelenburg position. Anaesth Intensive Care. 2007;35:281–5.
Díaz FJ, de La Peña E, Hernández V, López B, de La Morena JM, Martín MD, et al. Optimization of an early discharge program after laparoscopic radical prostatectomy. Actas Urol Esp. 2014;38:355–60.
Availability of data and material
All data generated or analyzed during this study are included in this published article and are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SB: Ethics approval, study design, data collection and analysis, drafted the manuscript and reviewed it for important intellectual content; MH: Idea for study, study design, patient recruitment, data collection and finally reviewed the manuscript for important intellectual content; FZ: Data analysis and interpretation, finally reviewed the manuscript for important intellectual content; TS: Made acquisitions, interpret data and finally reviewed the manuscript for important intellectual content; ML: Made acquisitions, interpret data and finally reviewed the manuscript for important intellectual content; MB: Made acquisitions, interpret data and finally reviewed the manuscript for important intellectual content; SD: Made acquisitions and interpret of data and finally reviewed the manuscript for important intellectual content; MP: Idea for study, study design, data collection and interpretation, patient recruitment and finally reviewed the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no competing interest in relation to this paper.
Ethics approval
This study was approved by the local institutional review board of the University of Regensburg (Protocol No. 14-101-0107) and registered at the local Center for Clinical Studies (Z-2014-0387-6. Registered on 8 July 2014).
Informed consent
After detailed explanation, written informed consent was obtained from 51 patients scheduled for elective prostatectomy at the Department of Urology in Regensburg.
Rights and permissions
About this article
Cite this article
Blecha, S., Harth, M., Zeman, F. et al. The impact of obesity on pulmonary deterioration in patients undergoing robotic-assisted laparoscopic prostatectomy. J Clin Monit Comput 33, 133–143 (2019). https://doi.org/10.1007/s10877-018-0142-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0142-3