Abstract
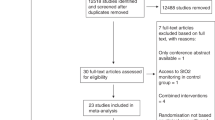
Patients undergoing cardiological procedures generally have significant cardiovascular morbidity, and therefore these patients might be at risk for major periprocedural complications. The ability to closely monitor the hemodynamic status would present a major advantage to optimize patient care in this setting. The aim of this review is to assess the available evidence for the use of near-infrared spectroscopy (NIRS) in the care of patients during cardiological procedures. A systematic literature search was conducted using electronic bibliographic databases (MEDLINE, PubMed, EMBASE) from their first available date using the following search strategy: (spectroscopy, near-infrared OR infrared spectroscopy OR NIRS OR cerebral oxygen*) AND (interventional OR electrophysiological OR catheterization OR ablation OR ICD OR defibrillator). Inclusion criteria were limited to human studies, English language and cardiac patients. All manuscripts concerning the use of NIRS in every area of catheterization and electrophysiology were included. The literature search yielded eleven observational studies and five case reports concerning the research question. No randomized trials could be retrieved. Six studies evaluated NIRS during supraventricular and ventricular arrhythmias, one during transcatheter aortic valve implantations, and four studies assessed the use of NIRS in pediatric catheterization procedures. Overall, the studies demonstrated that NIRS provides a very quick representation of cerebral oxygen saturation and that it might identify changes that could not be predicted from standard hemodynamic monitoring. However, the evidence is currently too low to conclude that NIRS can optimize patient care during cardiological procedures.

Similar content being viewed by others
References
Ermis P, Franklin W, Mulukutla V, Parekh D, Ing F. Left ventricular hemodynamic changes and clinical outcomes after transcatheter atrial septal defect closure in adults. Congenit Heart Dis. 2015;10:E48–53.
Jobsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
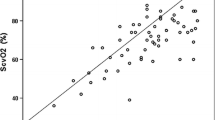
Moerman A, Vandenplas G, Bové T, Wouters P, De Hert S. Relation between mixed venous oxygen saturation and cerebral oxygen saturation measured by absolute and relative near-infrared spectroscopy during off-pump coronary artery bypass grafting. Br J Anaesth. 2013;110:258–65.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM 3rd, Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K, Parr GV. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87:36–44.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Dreyer N, Velentgas P, Westrich K, Dubois R. The GRACE checklist for rating the quality of observational studies of comparative effectiveness: a tale of hope and caution. J Manag Care Pharm. 2014;20:301–8.
Harbour R, Miller J, Scottish Intercollegiate Guidelines Network Grading Review Group. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–6.
de Vries JW, Visser GH, Bakker PFA. Neuromonitoring in defibrillation threshold testing. A comparison between EEG, near-infrared spectroscopy and jugular bulb oximetry. J Clin Monit. 1997;13:303–7.
McNeill E, Gagnon RE, Potts JE, Yeung-Lai-Wah JA, Kerr CR, Sanatani S. Cerebral oxygenation during defibrillator threshold testing of implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2005;28:528–33.
Singer I, Edmonds H. Changes in cerebral perfusion during third-generation implantable cardioverter defibrillator testing. Am Heart J. 1994;127:1052–7.
Smith DS, Levy W, Maris M, Chance B. Reperfusion hyperoxia in brain after circulatory arrest in humans. Anesthesiology. 1990;73:12–9.
Wutzler A, Otto N, Gräser S, Boldt LH, Huemer M, Parwani A, Haverkamp W, Storm C. Acute decrease of cerebral oxygen saturation during rapid ventricular and supraventricular rhytm: a pilot study. Pacing Clin Electrophysiol. 2014;37:1159–65.
Wutzler A, Nee J, Boldt L-H, Kühnle Y, Gräser S, Schröder T, Haverkamp W, Storm C. Improvement of cerebral oxygen saturation after successful electrical cardioversion of atrial fibrillation. Europace. 2014;16:189–94.
Paarmann H, Heringlake M, Heinze H, Hanke T, Sier H, Karsten J, Schön J. Non-invasive cerebral oxygenation reflects mixed venous oxygen saturation during the varying haemodynamic conditions in patients undergoing transapical transcatheter aortic valve implantation. Interact CardioVasc Thorac Surg. 2012;14:268–72.
Tanidir IC, Ozturk E, Ozyilmaz I, Saygi M, Kiplapinar N, Haydin S, Guzeltas A, Odemis E. Near infrared spectroscopy monitoring in the pediatric cardiac catheterization laboratory. Artif Organs. 2014;38:838–44.
de Vries JW, Hoorntje TM, Sreeram N. Neurophysiological effects of pediatric balloon dilatation procedures. Pediatr Cardiol. 2000;21:461–4.
Van der Laan ME, Verhagen EA, Bos AF, Berger RMF, Kooi EMW. Effect of balloon atrial septostomy on cerebral oxygenation in neonates with transposition of the great arteries. Pediatr Res. 2011;73:62–7.
Hershenson JA, Ro PS, Miao Y, Tobias JD, Olshove V, Naguib AN. Changes in hemodynamic parameters and cerebral saturation during supraventricular tachycardia. Pediatr Cardiol. 2012;33:286–9.
de Vries JW, Haanschoten M. Resuscitation in pediatric balloon valvuloplasty: effects on cerebral perfusion and oxygenation. J Cardiothorac Vasc Anesth. 2000;14:581–3.
Jinnouchi Y, Kawahito S, Kitahata H, Tanaka K, Nozaki J, Oshita S. Anesthetic management of a patient undergoing cardioverter defibrillator implantation: usefulness of transesophageal echocardiography and near infrared spectroscopy. J Anesth. 2004;18:220–3.
de Vries JW, Hoorntje T, Bakker PFA. Cerebral oxygen saturation monitoring in an infant undergoing ICD implantation. J Cardiothorac Vasc Anesth. 1998;12:442–4.
Paarmann H, Heringlake M, Sier H, Schön J. The association of non-invasive cerebral and mixed venous oxygen saturation during cardiopulmonary resuscitation. Interact CardioVasc Thorac Surg. 2010;11:371–3.
Nagdyman N, Fleck T, Ewert P, Abdul-Khaliq H, Redlin M, Lange P. Cerebral oxygenation measured by near-infrared spectroscopy during circulatory arrest and cardiopulmonary resuscitation. Br J Anaesth. 2003;91:438–42.
Levy W, Levin S, Chance B. Near-infrared measurement of cerebral oxygenation. Anesthesiology. 1995;83:738–46.
Ettorre E, Cicerchia M, De Benedetto G, Fossati C, Guglielmi S, Manzon L, Servello A, Petrillo A, Marigliano V. A possible role of atrial fibrillation as a risk factor for dementia. Arch Gerontol Geriatr. 2009;49(Suppl 1):71–6.
Elbers P, Prins W, Plokker H, van Dongen E, van Iterson M, Ince C. Electrical cardioversion for atrial fibrillation improves microvascular flow independent of blood pressure changes. J Cardiothorac Vasc Anesth. 2012;26:799–803.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90:1052–9.
McQuillen PS, Hamrick SE, Perez MJ, Barkovich AJ, Glidden DV, Karl TR, Teitel D, Miller SP. Balloon atrial septostomy is associated with preoperative stroke in neonates with transposition of the great arteries. Circulation. 2006;113:280–5.
Block AJ, McQuillen PS, Chau V, Glass H, Poskitt KJ, Barkovich AJ, Esch M, Soulikias W, Azakie A, Campbell A, Miller SP. Clinically silent preoperative brain injuries do not worsen with surgery in neonates with congenital heart disease. J Thorac Cardiovasc Surg. 2010;140:550–7.
Murkin JM, Baird DL, Martzke JS, Yee R. Cognitive dysfunction after ventricular fibrillation during implantable cardiovertor/defibrillator procedures is related to duration of the reperfusion interval. Anesth Analg. 1997;84:1186–92.
Scott JP, Hoffman GM. Near-infrared spectroscopy: exposing the dark (venous) side of the circulation. Paediatr Anaesth. 2014;24:74–88.
Scheeren TWL, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Pedersen T, Nicholson A, Hovhannisyan K, Moller AM, Smith AF, Lewis SR. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2014;3:CD002013. doi:10.1002/14651858.CD002013.pub3.
Dreyer N. Making observational studies count. Shaping the future of comparative effectiveness research. Epidemiology. 2011;22:295–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Moerman, A., Meert, F. & De Hert, S. Cerebral near-infrared spectroscopy in the care of patients during cardiological procedures: a summary of the clinical evidence. J Clin Monit Comput 30, 901–909 (2016). https://doi.org/10.1007/s10877-015-9791-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9791-7