Abstract
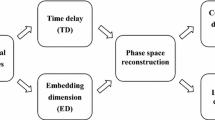
Detection of hypovolemia prior to overt hemodynamic decompensation remains an elusive goal in the treatment of critically injured patients in both civilian and combat settings. Monitoring of heart rate variability has been advocated as a potential means to monitor the rapid changes in the physiological state of hemorrhaging patients, with the most popular methods involving calculation of the R–R interval signal’s power spectral density (PSD) or use of fractal dimensions (FD). However, the latter method poses technical challenges, while the former is best suited to stationary signals rather than the non-stationary R–R interval. Both approaches are also limited by high inter- and intra-individual variability, a serious issue when applying these indices to the clinical setting. We propose an approach which applies the discrete wavelet transform (DWT) to the R–R interval signal to extract information at both 500 and 125 Hz sampling rates. The utility of machine learning models based on these features were tested in assessing electrocardiogram signals from volunteers subjected to lower body negative pressure induced central hypovolemia as a surrogate of hemorrhage. These machine learning models based on DWT features were compared against those based on the traditional PSD and FD, at both sampling rates and their performance was evaluated based on leave-one-subject-out fold cross-validation. Results demonstrate that the proposed DWT-based model outperforms individual PSD and FD methods as well as the combination of these two traditional methods at both sample rates of 500 Hz (p value <0.0001) and 125 Hz (p value <0.0001) in detecting the degree of hypovolemia. These findings indicate the potential of the proposed DWT approach in monitoring the physiological changes caused by hemorrhage. The speed and relatively low computational costs in deriving these features may make it particularly suited for implementation in portable devices for remote monitoring.




Similar content being viewed by others
References
Kelly JF, Ritenour AE, McLaughlin DF, Bagg KA, Apodaca AN, Mallak CT, Pearse L, Lawnick MM, Champion HR, Wade CE, Holcomb JB. Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003–2004 versus 2006. J Trauma. 2008;64:S21–6.
Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, Browder T, Noguchi TT, Demetriades D. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007;63:1338–46.
Alam HB, Burris D, DaCorta JA. Hemorrhage control in the battlefield: role of new hemostatic agents. Mil Med. 2005;170(1):63–9.
Weil MH, Becker L, Budinger T, Kern K, Nichol G, Shechter I, Traystman R, Wiedemann H, Wise R, Weisfeldt M, Sopko G. Post resuscitative and initial utility in life saving efforts (pulse): a workshop executive summary. Resuscitation. 2001;50(1):23–5.
Convertino VA, Ryan KL, Rickards CA, Salinas J, McManus JG, Cooke WH, Holcomb JB. Physiological and medical monitoring for en route care of combat casualties. J Trauma. 2008;64:S342–53.
Schwartz PJ, Priori SG. Sympathetic nervous system and cardiac arrhythmias. In: Zipes DP, Jalife J, editors. Cardiac electrophysiology. Philadelphia: WB Saunders Company; 1990.
Task Force of the European Society of Cardiology, the North American Society of Pacing, and Electrophysiology. Heart rate variability, standards of measurement, physiological interpretation and clinical use. Circulation. 1996;96:1043–65.
Cooke WH, Salinas J, Convertino VA, Ludwig DA, Hinds D, Duke JH, Moore FA, Holcomb JB. Heart rate variability and its association with mortality in prehospital trauma patients. J Trauma. 2006;60:363–70.
Cooke WH, Salinas J, McManus JG, Ryan KL, Rickards CA, Holcomb JB, Convertino VA. Heart period variability in trauma patients may predict mortality and allow remote triage. Aviat Space Environ Med. 2006;77:1107–12.
Rapenne T, Moreau D, Lenfant F, Vernet M, Boggio V, Cottin Y, Freysz M. Could heart rate variability predict outcome in patients with severe head injury? A pilot study. J Neurosurg Anesthesiol. 2001;13:260–8.
Batchinsky AI, Cancio LC, Salinas J, Kuusela T, Cooke WH, Wang JJ, Boehme M, Convertino VA, Holcomb JB. Prehospital loss of R-to-R interval complexity is associated with mortality in trauma patients. J Trauma. 2007;63:512–8.
Cancio LC, Batchinsky AI, Salinas J, Kuusela T, Convertino VA, Wade CE, Holcomb JB. Heart-rate complexity for prediction of prehospital lifesaving interventions in trauma patients. J Trauma. 2008;65:813–9.
Gang Y, Malik M. Heart rate variability in critical care medicine. Curr Opin Crit Care. 2002;8:371–5.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–2.
Cooke WH, Convertino VA. Heart rate variability and spontaneous baroreflex sequences: implications for autonomic monitoring during hemorrhage. J Trauma. 2005;58:798–805.
Cooke WH, Rickards CA, Ryan KL, Convertino VA. Autonomic compensation to simulated hemorrhage monitored with heart period variability. Crit Care Med. 2008;36:1892–9.
Ryan KL, Rickards CA, Ludwig DA, Convertino VA. Tracking central hypovolemia with ECG in humans: cautions for the use of heart period variability in patient monitoring. Shock. 2010;33(6):583–9.
Cooke WH, Ryan KL, Convertino VA. Lower body negative pressure as a model to study progression to acute hemorrhagic shock in humans. J Appl Physiol. 2004;96:1249–61.
Bennett T. Cardiovascular responses to central hypovolaemia in man: physiology and pathophysiology. Physiologist. 1987;30:S143–6.
Murray RH, Thompson LJ, Bowers JA, Albright CD. Hemodynamic effects of graded hypovolemia and vasodepressor syncope induced by lower body negative pressure. Am Heart J. 1968;76:799–811.
van Hoeyweghen R, Hanson J, Stewart MJ, Dethune L, Davies I, Little RA, Horan MA, Kirkman E. Cardiovascular response to graded lower body negative pressure in young and elderly man. Exp Physiol. 2001;86(03):427–35.
Pomeranz B, Macaulay RJ, Caudill MA, Kutz I, Adam D, Gordon D, Kilborn KM, Barger AC, Shannon DC, Cohen RJ. Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol. 1985;248:H151–3.
Esteller R, Vachtsevanos G, Echauz J, Litt B. A comparison of waveform fractal dimension algorithms. IEEE Trans Circuits Syst I. 2001;48(2):177–83.
Batchinsky AI, Cooke WH, Kuusela TA, Jordan BS, Wang JJ, Cancio LC. Sympathetic nerve activity and heart rate variability during severe hemorrhagic shock in sheep. Auton Neurosci. 2007;136(1–2):43–51.
Acharya UR, Joseph KP, Kannathal N, Lim CM, Suri JS. Heart rate variability: a review. Med Biol Eng Comput. 2006;44:1031–51.
Acharya UR, Subbanna BP, Kannathal N, Rao A, Lim CM. Analysis of cardiac health using fractal dimension and wavelet transformation. ITBM-RBM. 2005;26(2):133–9.
Yeragani VK, Srinivasan K, Vempati S, Pohl R, Balon R. Fractal dimension of heart rate time series, an effective measure of autonomic function. J Appl Physiol. 1993;75(6):2429–38.
Carlin M. Measuring the complexity of non-fractal shapes by a fractal method. Pattern Recogn Lett. 2000;21(11):1013–7.
Accardo A, Affinito M, Carrozzi M, Bouquet F. Use of the fractal dimension for the analysis of electroencephalographic time series. Biol Cybern. 1997;77:339–50.
Meyer Y. Wavelets: algorithms and applications. SIAM; 1993, translated and revised by R. D. Ryan.
Unser M, Aldroubi A. A review of wavelets in biomedical applications. Proc IEEE. 1996;84(4):626–38.
Addison PS. Wavelet transforms and the ECG: a review. Physiol Meas. 2005;26:R155–99.
Aldroubi A, Unser M, editors. Wavelets in medicine and biology. Boca Raton: CRC Press; 1996.
Stiles MK, Clifton D, Grubb NR, Watson JN, Addison PS. Wavelet-based analysis of heart-rate-dependent ECG features. Ann Noninvasive Electrocardiol. 2004;9:316–22.
Burri H, Chevalier P, Arzi M, Rubel P, Kirkorian G, Touboul P. Wavelet transform for analysis of heart rate variability preceding ventricular arrhythmias in patients with ischemic heart disease. Int J Cardiol. 2006;109(1):101–7.
Hilton MF, Bates RA, Godfrey KR, Chappell MJ, Cayton RM. Evaluation of frequency and time-frequency spectral analysis of heart rate variability as a diagnostic marker of the sleep apnoea syndrome. Med Biol Eng Comput. 1999;37:760–9.
Tan BH, Shimizu H, Hiromoto K, Furukawa Y, Ohyanagi M, Iwasaki T. Wavelet transform analysis of heart rate variability to assess the autonomic changes associated with spontaneous coronary spasm of variant angina. J Electrocardiol. 2003;36:117–24.
Ji SY, Chen W, Ward K, Ryan K, Rickards C, Convertino V, Najarian K. Wavelet based analysis of physiological signals for prediction of severity of hemorrhagic shock. In Proceedings of IEEE international conference on complex medical engineering (CME); 2009. p. 1–6.
Ji SY, Soo-Yeon. Computer-aided trauma decision making using machine learning and signal processing. PhD dissertation, VCU digital archives, 2008.
Gomez C, Mediavilla A, Hornero R, Abasolo D, Fernandez A. Use of the Higuchi’s fractal dimension for the analysis of MEG recordings from Alzheimer’s disease patients. Med Eng Phys. 2009;31:306–13.
Najarian K. Fixed-distribution PAC learning theory for neural FIR models. J Intell Inform Syst. 2005;25(30):275–91.
Najarian K. Learning-based complexity evaluation of radial basis function networks. Neural Process Lett. 2002;16(2):137–50.
Suykens JAK, Vandewalle JPL. Least squares support vector machine classifiers. Neural Process Lett. 1999;9(3):293–300.
Candelieri A, Conforti D. A hyper-solution framework for SVM classification: application for predicting destabilizations in chronic heart failure patients. Open Med Inform J. 2010;4:136–40.
Ducla-Soares JL, Santos-Bento M, Laranjo S, Andrade A, Ducla-Soares E, Boto JP, Silva-Carvalho L, Rocha IJL. Wavelet analysis of autonomic outflow of normal subjects on head-up tilt, cold pressor test, Valsalva manoeuvre and deep breathing. Exp Physiol. 2007;92(4):677–86.
Kohavi R. A study of cross-validation and bootstrap for accuracy estimation and model selection. In: Proceedings of international joint conference on AI; 1995. p. 1137–1145.
Ji SY, Bsoul AR, Ward K, Ryan K, Rickards C, Convertino V, Najarian K. Incorporating physiological signals to blood loss prediction based on discrete wavelet transformation. Circulation. 2009;120:1483.
Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MS, Go AS, Harrell FE, Hong Y Jr, Howard BV, Howard VJ, Hsue PY, Kramer CM, McConnell JP, Normand SL, O’Donnell CJ, Smith SC Jr, Wilson PW. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–16.
Pan J, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng. 1985;32:230–6.
Acknowledgments
This material is based upon work supported by the National Science Foundation under Grant No. IIS0758410 and by the U.S. Army Medical Research and Material Command Combat Casualty Care Research Program (Grant: 05-0033-02). The opinions expressed herein are the personal opinions of the authors and are not to be construed as representing those of the Department of Defense, the Department of the Army, or the United States Army.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
This section explains the process of QRS detection performed prior to feature extraction. Construction of the RR signal using the RR intervals in the ECG signal first requires that the R-waves be identified, which is done via QRS detection. The most common technique is the Pan-Tompkins algorithm [49], which detects QRS complexes based on analysis of their slope, amplitude and width. This method consists of four stages: band-pass filtering, differentiation, squaring, and windowing. The first stage applies the same filter as described in Sect. 2.2. The signal is then passed through a differentiator which suppresses the low-frequency P and T wave components and emphasizes the steep slopes of the QRS complex. The QRS complex also displays high amplitude, which is emphasized by applying a squaring operator. The next stage uses a moving average window to smooth the signal and reduce noise. The final step is to select a threshold that detects the QRS peaks in the waveform.
This study applies a modified version of the Pan-Tompkins algorithm which incorporates an additional histogram analysis step after averaging is performed, to identify any unusual values which may cause errors in the QRS detection process. It also employs an adaptive threshold T to detect the QRS peaks, which offers more flexibility in dealing with individuals than a fixed threshold. This is calculated as \( T = \mu (S) + \hbox{max} (S)*\alpha \), where S is the filtered ECG stage segment currently being analyzed and α is an empirically-chosen weight measure. This study found α = 0.4 to be a suitable value.
In calculating the RR intervals, any single interval is compared to those previously detected using a sliding window. This process is described as follows. Let \( I_{i} \) be the estimate of the RR interval at sample i, n the total number of RR intervals detected so far, and \( \omega_{0} \), \( \omega_{1} \), and \( \omega_{2} \)be boundaries on the acceptable range of variation of the interval, chosen based on previous interval values. In order to find the new RR interval l, the following rules are followed:
The boundaries are set as \( \omega_{0} = 0.89m,\,\omega_{1} = 1.29m \) and \( \omega_{2} = 2m \), where m is the median value of the previous eight RR intervals.
Appendix 2
This section briefly explains the two other HRV analysis methods used in this study. Power spectral density (PSD) describes the distribution of the power in a signal with frequency [22]. In other words, it shows at which frequencies variations are strong and at which frequencies variations are weak. The measures of interest in this study are the powers of the high frequency (HF; 0.15–0.4 Hz), low frequency (LF; 0.04–0.15 Hz) and very low frequency (VLF; 0.003–0.04 Hz) bands, the normalized powers of the LF and HF bands, and the ratios of LF to HF and HF to LF. These are calculated by integrating the spectrum for each band. Normalization is performed by calculating
where TAP is the total average power of the RR interval [7].
Fractal analysis monitors data via fractals: sets of points that can be divided into subsets which each resemble the whole. Calculating the FD of a signal quantifies both this self-similarity and the signal’s complexity. FD is commonly used in analyzing biosignals such as electrocardiogram (ECG) and electroencephalogram (EEG) to differentiate physiological states. This study applies Higuchi’s algorithm to calculate the FD of the ECG segments recorded over each LBNP stage. Consider a signal \( X_{i} = x_{1} ,x_{2} , \ldots ,x_{n} \), consisting of n samples. This is first divided into smaller epochs, by constructing k new time series \( x_{m}^{k} \)such that
where \( m = 1, \ldots ,k \) indicates the initial time value and k is the time interval between points. For each \( x_{m}^{k} \), the average length \( L_{m} (k) \) is calculated as
where \( a = \frac{N - m}{k} \). The average length \( L(k) \)for each delay k is calculated as the mean of the k lengths \( L_{m} (k) \) for \( m = 1,2, \ldots ,k \). This is repeated for each of the k time series. The Higuchi FD is estimated as the slope of the least-squares best fit line to the curve of \( \ln [L(k)] \) versus \( \ln \left( \frac{1}{k} \right) \) for \( k = 1, \ldots ,k_{\hbox{max} } \) [23]. Calculation accuracy depends on the epoch length; this study tested lengths of 8 and 15.
Rights and permissions
About this article
Cite this article
Ji, SY., Belle, A., Ward, K.R. et al. Heart rate variability analysis during central hypovolemia using wavelet transformation. J Clin Monit Comput 27, 289–302 (2013). https://doi.org/10.1007/s10877-013-9434-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9434-9