Abstract
Objective
In a recent clinical study on the reliability of a point-of-care (POC) analyzer, we described a downward bias in hematocrit measurement during cardiopulmonary bypass leading potentially to overtreatment with packed red cells. We hypothesized that the detected deviation is caused by variations in electrolyte concentration rather than by colloids used.
Methods
Blood was sampled from patients before cardiac surgery to obtain undiluted anticoagulated whole blood samples (n = 53). From each sample, four dilution series covering a hematocrit range of 15–30% were made using NaCl (0.9%), modified gelatine (4%), hydroxyethylstarch (6%), or a potassium-based (16 mEq/l) solution, respectively. In each dilution series, hematocrit was measured by POC and via the “golden standard” microcentrifugal method to determine whether the deviation of the POC-analyzer to the microcentrifuge was dependent on the type and dilution level of the solution used.
Results
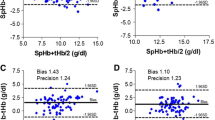
In contrast to the colloid-based dilution series, the crystalloids revealed a significant downward bias of the POC-analyzer with respect to the microcentrifuge (p < 0.05). Due to the correction algorithm for sodium in the POC-analyzer, this deviation was nearly constant for NaCl (mean of difference: −1.8 ± 0.1%), but increased significantly in case of the potassium-based solution (up to −8.2 ± 0.4% after 1.5-times dilution). The starch- and gelatine-based solutions led to a significant upward bias (p < 0.05) that increased with progressing dilution (up to 1.2 ± 0.1% for hydroxyethylstarch and up to 1.3 ± 0.1% for modified gelatine after 1.5-times dilution).
Conclusions
Conductivity-based POC hematocrit measurement suffers from biases due to changes of the plasma constituents. The downward bias in hematocrit as often seen during cardiopulmonary bypass is driven by changes of different electrolyte concentration rather than by colloids used per se.
Similar content being viewed by others
References
Steinfelder-Visscher J, Weerwind PW, Teerenstra S, Brouwer MH (2006) Reliability of point-of-care hematocrit, blood gas, electrolyte, lactate and glucose measurement during cardiopulmonary bypass. Perfusion 21:33–37
Stott RAW, Hortin GL, Wilhite TR, Miller SB, Smith CH, Landt M (1995) Analytical artifacts in hematocrit measurements by whole-blood chemistry analyzers. Clin Chem 41:306–311
Fuller HD (1991) The electrical impedance of plasma: a laboratory simulation of the effect of changes in chemistry. Ann Biomed Eng 19:123–129
McNulty SE, Sharkey SJ, Asam B, Lee JH (1993) Evaluation of stat-crit(r) hematocrit determination in comparison to coulter and centrifuge – the effects of isotonic hemodilution and albumin administration. Anesth Analg 76:830–834
Hopfer SM, Nadeau FL, Sundra M, Makowski GS (2004) Effect of protein on hemoglobin and hematocrit assays with a conductivity-based point-of-care testing device: Comparison with optical methods. Ann Clin Lab Sci 34:75–82
McNulty SE, Sharkey SJ, Schieren H (1994) Bedside hemoglobin measurements: sensitivity to changes in serum protein and electrolytes. J Clin Monit 10:377–381
Vedrinne JM, Motin J (1991) Colloids and hematocrit measurement by conductivity. Anesth Analg 72:840
Connelly NR, Magee M, Kiessling B (1996) The use of the iSTAT portable analyzer in patients undergoing cardiopulmonary bypass. J Clin Monit 12:311–315
Beneteau-Burnat B, Bocque MC, Lorin A, Martin C, Vaubourdolle M (2004) Evaluation of the blood gas analyzer GEM (R) PREMIER 3000. Clin Chem Lab Med 42:96–101
Visser KR (1992) Electric conductivity of stationary and flowing human blood at low frequencies. Med Biol Eng Comput 30:636–640
Acknowledgement
The skilful assistance of Mrs. Honey Hashemi (Department of Extra-Corporeal Circulation, Radboud University Nijmegen Medical Centre, The Netherlands) in the preparation and analysis of the dilution series is highly appreciated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Steinfelder-Visscher J, Weerwind PW, Teerenstra S, Pop GAM, Brouwer MHJ. Conductivity-based hematocrit measurement during cardiopulmonary bypass.
Rights and permissions
About this article
Cite this article
Steinfelder-Visscher, J., Weerwind, P.W., Teerenstra, S. et al. Conductivity-Based Hematocrit Measurement During Cardiopulmonary Bypass. J Clin Monit Comput 21, 7–12 (2007). https://doi.org/10.1007/s10877-006-9052-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-006-9052-x