Abstract
Objective
Immunodeficiency, centromeric instability, and facial anomalies (ICF) syndrome is a rare autosomal recessive primary immunodeficiency. Hypogammaglobulinemia is a major manifestation of ICF syndrome, but immunoglobulin replacement therapy does not seem to be effective for some ICF patients. Therefore, we aimed to reassess the immunological characteristics of this syndrome.
Methods
Eleven Japanese patients with ICF syndrome were enrolled. We performed whole-exome sequencing in four cases and homozygosity mapping using SNP analysis in two. We evaluated their clinical manifestations and immunological status.
Results
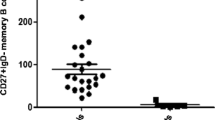
We newly diagnosed six ICF patients who had tentatively been diagnosed with common variable immunodeficiency. We identified two novel mutations in the DNMT3B gene and one novel mutation in the ZBTB24 gene. All patients showed low serum IgG and/or IgG2 levels and were treated by periodic immunoglobulin replacement therapy. Three of the six patients showed worse results of the mitogen-induced lymphocyte proliferation test. Analyses of lymphocyte subpopulations revealed that CD19+CD27+ memory B cells were low in seven of nine patients, CD3+ T cells were low in three patients, CD4/8 ratio was inverted in five patients, CD31+ recent thymic emigrant cells were low in two patients, and CD19+ B cells were low in four patients compared with those in the normal controls. ICF2 patients showed lower proportions of CD19+ B cells and CD16+56+ NK cells and significantly higher proportions of CD3+ T cells than ICF1 patients. T cell receptor excision circles were undetectable in two patients. Despite being treated by immunoglobulin replacement therapy, three patients died of influenza virus, fatal viral infection with persistent Epstein–Barr virus infection, or JC virus infection. One of three dead patients showed normal intelligence with mild facial anomaly. Two patients presented with autoimmune or inflammatory manifestations. Infectious episodes decreased in three patients who were started on trimethoprim–sulfamethoxazole and/or antifungal drugs in addition to immunoglobulin replacement therapy. These patients might have suffered from T cell immunodeficiency.
Conclusion
These results indicate that patients with ICF syndrome have a phenotype of combined immunodeficiency. Thus, to achieve a better prognosis, these patients should be treated as having combined immunodeficiency in addition to receiving immunoglobulin replacement therapy.



Similar content being viewed by others
Abbreviations
- CDCA7:
-
Cell division cycle-associated protein 7
- Con A:
-
Concanavalin A
- DNMT3B:
-
DNA methyltransferase 3B gene
- HELLS:
-
Helicase, lymphoid-specific
- HSCT:
-
Hematopoietic stem cell transplantation
- ICF:
-
Immunodeficiency, centromeric instability, and facial anomalies
- KREC:
-
Kappa-deleting recombination excision circles
- NGS:
-
Next-generation sequencing
- PCR:
-
Polymerase chain reaction
- PHA:
-
Phytohemagglutinin
- PML:
-
Progressive multifocal leukoencephalopathy
- RTE:
-
Recent thymic emigrant cells
- TREC:
-
T cell receptor excision circles
- ZBTB24:
-
Zinc finger and BTB domain-containing 24 gene
References
Ehrlich M, Jackson K, Weemaes C. Immunodeficiency, centromeric region instability, facial anomalies syndrome (ICF). Orphanet J Rare Dis. 2006;1:2.
Hagleitner MM, Lankester A, Maraschio P, Hultén M, Fryns JP, Schuetz C, et al. Clinical spectrum of immunodeficiency, centromeric instability and facial dysmorphism (ICF syndrome). J Med Genet. 2008;45:93–9.
Weemaes CM, van Tol MJ, Wang J, et al. Heterogeneous clinical presentation in ICF syndrome: correlation with underlying gene defects. Eur J Hum Genet. 2013;21:1219–25.
Xu GL, Bestor TH, Bourc’his D, Hsieh CL, Tommerup N, Bugge M, et al. Chromosome instability and immunodeficiency syndrome caused by mutations in a DNA methyltransferase gene. Nature. 1999;402:187–91.
Hansen RS, Wijmenga C, Luo P, Stanek AM, Canfield TK, Weemaes CMR, et al. The DNMT3B DNA methyltransferase gene is mutated in the ICF immunodeficiency syndrome. Proc Natl Acad Sci U S A. 1999;96:14412–7.
de Greef JC, Wang J, Balog J, den Dunnen J, Frants RR, Straasheijm KR, et al. Mutations in ZBTB24 are associated with immunodeficiency, centromeric instability, and facial anomalies syndrome type 2. Am J Hum Genet. 2011;88:796–804.
Thijssen PE, Ito Y, Grillo G, Wang J, Velasco G, Nitta H, et al. Mutations in CDCA7 and HELLS cause immunodeficiency-centromeric instability-facial anomalies syndrome. Nat Commun. 2015;6:7870.
Sterlin D, Velasco G, Moshous D, Touzot F, Mahlaoui N, Fischer A, et al. Genetic, cellular and clinical features of ICF syndrome: a French national survey. J Clin Immunol. 2016;36:149–59.
Blanco-Betancourt CE, Moncla A, Milili M, Jiang YL, Viegas-Péquignot EM, Roquelaure B, et al. Defective B-cell-negative selection and terminal differentiation in the ICF syndrome. Blood. 2004;103:2683–90.
Nitta H, Unoki M, Ichiyanagi K, Kosho T, Shigemura T, Takahashi H, et al. Three novel ZBTB24 mutations identified in Japanese and Cape Verdean type 2 ICF syndrome patients. J Hum Genet. 2013;58:455–60.
Pezzolo A, Prigione I, Facchetti P, Castellano E, Viale M, Gimelli G, et al. T-cell apoptosis in ICF syndrome. J Allergy Clin Immunol. 2001;108:310–2.
Rechavi E, Lev A, Eyal E, Barel O, Kol N, Barhom SF, et al. A novel mutation in a critical region for the methyl donor binding in DNMT3B causes immunodeficiency, centromeric instability, and facial anomalies syndrome (ICF). J Clin Immunol. 2016;36:801–9.
von Bernuth H, Ravindran E, Du H, et al. Combined immunodeficiency develops with age in immunodeficiency-centromeric instability-facial anomalies syndrome 2 (ICF2). Orphanet J Rare Dis. 2014;9:116.
Gennery AR, Slatter MA, Bredius RG, Hagleitner MM, Weemaes C, Cant AJ, et al. Hematopoietic stem cell transplantation corrects the immunologic abnormalities associated with immunodeficiency-centromeric instability-facial dysmorphism syndrome. Pediatrics. 2007;120:e1341–4.
Gössling KL, Schipp C, Fischer U, Babor F, Koch G, Schuster FR, et al. Hematopoietic stem cell transplantation in an infant with immunodeficiency, centromeric instability, and facial anomaly syndrome. Front Immunol. 2017;8:773.
Stiehm ER, Fudenberg HH. Serum levels of immune globulins in health and disease: a survey. Pediatrics. 1966;37:715–27.
Shirohzu H, Kubota T, Kumazawa A, Sado T, Chijiwa T, Inagaki K, et al. Three novel DNMT3B mutations in Japanese patients with ICF syndrome. Am J Med Genet. 2002;112:31–7.
Takashima T, Okamura M, Yeh TW, Okano T, Yamashita M, Tanaka K, et al. Multicolor flow cytometry for the diagnosis of primary immunodeficiency diseases. J Clin Immunol. 2017;37:486–95.
Shearer WT, Rosenblatt HM, Gelman RS, Oyomopito R, Plaeger S, Stiehm ER, et al. Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol. 2003;112:973–80.
Morinishi Y, Imai K, Nakagawa N, Sato H, Horiuchi K, Ohtsuka Y, et al. Identification of severe combined immunodeficiency by T-cell receptor excision circles quantification using neonatal Guthrie cards. J Pediatr. 2009;155:829–33.
Nakagawa N, Imai K, Kanegane H, Sato H, Yamada M, Kondoh K, et al. Quantification of κ-deleting recombination excision circles in Guthrie cards for the identification of early B-cell maturation defects. J Allergy Clin Immunol. 2011;128:223–5.e2.
Kamae C, Nakagawa N, Sato H Honma K, Mitsuiki N, Ohara O, Kanegane H, Pasic S, Pan-Hammarström Q, van Zelm MC, Morio T, Imai K, Nonoyama S. Common variable immunodeficiency classification by quantifying T-cell receptor and immunoglobulin κ-deleting recombination excision circles. J Allergy Clin Immunol 2013; 131: 1437–40.e5.
Acknowledgments
We thank Dr. Takehiro Takashima, Dr. Koichi Inagaki, Dr. Naomi Terada, Ms. Kaori Tomita, and Ms. Kimiko Gasa for their excellent technical assistance. We are grateful to the patients and their families for their participation in this study.
Authorship Contributions
C.K., K.I., H.K., and S.N. designed the study and wrote the manuscript. T.K., K.H., N.N., and T-W.Y. performed the flow cytometric analysis and collected the data. T.O., E.N., and O.O. performed the gene analysis. A.O., T.S., H.T., S.T., M.H., A.H., S.W., and T.S. cared for the patients. H.S., T.K., and T.M. contributed to the critical discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent was obtained from the parents of the pediatric patients and from the adult patients, in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics board of the National Defense Medical College and Tokyo Medical and Dental University.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Electronic Supplementary Material
Figure S1
Immunoglobulin levels of ICF patients. Serum immunoglobulin levels of patients with ICF1 (white circle) and ICF2 (black circle) are shown. (A) Serum levels of IgG. (B) Serum levels of IgG2. (C) Serum levels of IgA. (D) Serum levels of IgM. Each immunoglobulin value is expressed separately for the ICF subtypes (ICF1 or ICF2) and each age group (7–12 months old, 3–5 years old, and adult). The horizontal bars in the figures show the average value of each age group. (PPTX 90 kb). The normal values of serum level globulins were taken from Stiehm et al. [16]. We defined normal ranges of serum levels of globulins as from 10th (or − 1.28 SD) to 90th (or + 1.28 SD) [16] as shown by vertical bars.
Figure S2
Lymphocyte subpopulations of patients with ICF syndrome. Lymphocyte subpopulations of patients with ICF1 (white circle) and ICF2 (black circle) are shown. (A) Percentages of CD3+ T cells. (B) The ratios of CD4+ to CD8+ T cell lymphocytes. (C) Percentages of CD31+ recent thymic emigrant cells (RTE) among CD3+CD4+CD45RA+ cells. (D) Percentages of CD19+ B cells. (E) Percentages of CD19+CD27+ memory B cells. (F) Percentages of CD16+56+ NK cells. Each lymphocyte subpopulation is expressed separately for the ICF subtypes (ICF1 or ICF2) and each age group (2–6 years old, 7–19 years old, and adult). The horizontal bars in the figures show the average value of each age group. The normal percentages of control data were taken from the work of Takashima et al. [18]. Vertical bars indicate the range from − 1.28 standard deviations (10th) to + 1.28 standard deviations (90th) of normal controls of each age group (PPTX 121 kb)
Rights and permissions
About this article
Cite this article
Kamae, C., Imai, K., Kato, T. et al. Clinical and Immunological Characterization of ICF Syndrome in Japan. J Clin Immunol 38, 927–937 (2018). https://doi.org/10.1007/s10875-018-0559-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-018-0559-y