Abstract
Purpose
Complete DiGeorge syndrome (cDGS) describes a subset of patients with DiGeorge syndrome that have thymic aplasia, and thus are at risk for severe opportunistic infections. Patients with cDGS and mycobacterial infection have not previously been described. We present this case to illustrate that patients with cDGS are at risk for nontuberculous mycobacterial infections and to discuss further antimicrobial prophylaxis prior to thymic transplantation.
Methods
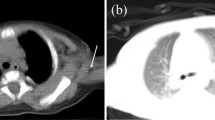
A 13-month old male was identified as T cell deficient by the T cell receptor excision circle (TREC) assay on newborn screening, and was subsequently confirmed to have cDGS. He presented with fever and cough, and was treated for chronic aspiration pneumonia as well as Pneumocystis jirovecii infection without significant improvement. It was only after biopsy of mediastinal lymph nodes seen on CT that the diagnosis of disseminated Mycobacterium kansasii was made. We reviewed the literature regarding atypical mycobacterial infections and prophylaxis used in other immunocompromised patients, as well as the current data regarding cDGS detection through TREC newborn screening.
Results
Multiple cases of cDGS have been diagnosed via TREC newborn screening, however this is the first patient with cDGS and disseminated mycobacterial infection to be reported in literature. Thymic transplantation is the definitive treatment of choice for cDGS. Prophylaxis with either clarithromycin or azithromycin has been shown to reduce mycobacterial infections in children with advanced human immunodeficiency virus infection.
Conclusions
Children with cDGS should receive thymic transplantion as soon as possible, but prior to this are at risk for nontuberculous mycobacterial infections. Severe, opportunistic infections may require invasive testing for diagnosis in patients with cDGS. Antimicrobial prophylaxis should be considered to prevent disseminated mycobacterial infection in these patients.


Similar content being viewed by others
References
Davies EG. Immunodeficiency in DiGeorge syndrome and options for treating cases with complete athymia. Front Immunol. 2013;4:322.
Markert ML, Devlin BH, Alexieff MJ, Li J, McCarty EA, Gupton SE, et al. Review of 54 patients with DiGeorge anomoly enrolled in protocols for thymus transplantation: outcome of 44 consecutive transplants. Blood. 2007;109:4639–47.
Kwan A, Church JA, Cowan MJ, Agarwal R, Kapoor N, Kohn DB, et al. Newborn screening for severe combined immunodeficiency and T-cell lymphopenia in California: results of the first 2 years. J Allergy Clin Immunol. 2013;132:140–50.
Bassett AS, McDonald-McGinn DM, Devriendt K, Digilio MC, Goldenberg P, Habel A, et al. Practical guidelines for managing patients with 22q11.2 deletion syndrome. J Pediatr. 2011;159:332–9.e1.
Frame JL, Borte S, von Dobelin U, Hammarstrom L, Oskarsdottir S. Retrospective analysis of TREC based newborn screening results and clinical phenotypes in infancts wthe the 22q11 deletion syndrome. J Clin Immunol. 2014;34:514–9.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416.
To M, Yazawa J, Hitani A, Sagara H, Kano I, Haruki K. Clinical and microbiological features of patients with pulmonary nontuberculous mycobacterial infection. Rinsho Byori Jpn J Clin Pathol. 2013;61(8):671–8.
Johnson MM, Odell JA. Nontuberculous mycobacterial pulmonary infections. J Thorac Dis. 2014;6:210–20.
Panel on Opportunistic Infections in HIV-Exposed and HIV-Infected Children. In: Guidelines for the prevention and treatment of opportunistic infections in HIV-exposed and HIV-infected children. Department of Health and Human Services. 2013. http://aidsinfo.nih.gov/contentfiles/lvguidelines/oi_guidelines_pediatrics.pdf. Accessed 7 Sept 2014.
Uthman MM, Uthman OA, Yahaya I. Interventions for the prevention of mycobacterium avium complex in adults and children with HIV. Cochrane Database Syst Rev. 2013;4:Cd007191.
Agada NO, Yin SM, Tam JS, Kelly MS, Markert ML. Disseminated atypical Mycobacterial Infection in three patients with complete digeroge anomaly. Poster presented at American Academy of Allergy, Asthma, and Immunology 2015 Annual Meeting; 2015 Feb 21; Houston, TX.
Author information
Authors and Affiliations
Corresponding author
Additional information
This manuscript presents original research conducted by the authors.
The material in this manuscript is not under consideration by any other journal.
All authors contributed in a substantive and intellectual manner to the research being presented.
Rights and permissions
About this article
Cite this article
Yin, S.M., Ferdman, R.M., Wang, L. et al. Disseminated Mycobacterium kansasii Disease in Complete DiGeorge Syndrome. J Clin Immunol 35, 435–438 (2015). https://doi.org/10.1007/s10875-015-0171-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-015-0171-3