Abstract
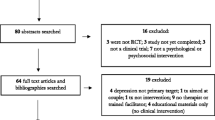
Pregnancy-specific stress (PSS) arises from the numerous changes that women experience during pregnancy and from their concerns about childbirth and the health of their offspring. Prolonged or elevated maternal stress heightens risk for poor fetal, infant, and child outcomes. The Prenatal Distress Questionnaire (PDQ) and its expanded successor, the revised Prenatal Distress Questionnaire (NuPDQ), were developed to assess PSS, but their psychometric properties and findings are not well-documented. We reviewed research using the PDQ (n = 45) or NuPDQ (n = 37). Results establish that PSS as measured by these instruments is common in pregnancy; PSS is associated with sociodemographic and obstetric characteristics, perceptions of pregnancy, health behaviors, maternal health, and birth outcomes. The NuPDQ is an especially appropriate tool to assess PSS, with demonstrated reliability and convergent, concurrent, and predictive validity. The ability to assess PSS in a reliable and valid manner is critical to advance research and improve maternal and child health.

Similar content being viewed by others
References
*Studies using the PDQ; **Studies using the NuPDQ
Accortt, E. E., & Wong, M. S. (2017). It is time for routine screening for perinatal mood and anxiety disorders in obstetrics and gynecology settings. Obstetrical & Gynecological Survey,72, 553–568.
*Alderdice, F., & Lynn, F. (2011). Factor structure of the Prenatal Distress Questionnaire. Midwifery,27, 553–559.
Alderdice, F., Lynn, F., & Lobel, M. (2012). A review and psychometric evaluation of pregnancy-specific stress measures. Journal of Psychosomatic Obstetrics and Gynecology,33, 62–77.
*Alderdice, F., Savage-McGlynn, E., Martin, C., McAuliffe, F., Hunter, A., Unterscheider, J., et al. (2013). The Prenatal Distress Questionnaire: An investigation of factor structure in a high risk population. Journal of Reproductive & Infant Psychology,31, 456–464.
*Asghari, E., Faramarzi, M., & Mohamadi, A. K. (2016). The effect of cognitive behavioural therapy on anxiety, depression and stress in women with preeclampsia. Journal of Clinical and Diagnostic Research,10, 4–7.
**Auerbach, M. V., Lobel, M., & Cannella, D. T. (2014). Psychosocial correlates of health-promoting and health-impairing behaviors in pregnancy. Journal of Psychosomatic Obstetrics & Gynecology,35, 76–83.
**Auerbach, M. V., Nicoloro-SantaBarbara, J., Rosenthal, L., Kocis, C., Weglarz, E. R., Busso, C. E., et al. (2017). Psychometric properties of the Prenatal Health Behavior Scale in mid- and late pregnancy. Journal of Psychosomatic Obstetrics & Gynecology,38, 143–151.
**Barcelona de Mendoza, V., Harville, E. W., Savage, J., & Giarratano, G. (2015). Experiences of intimate partner and neighborhood violence and their association with mental health in pregnant women. Journal of Interpersonal Violence,33, 938–959.
**Barcelona de Mendoza, V., Harville, E. W., Savage, J., & Giarratano, G. (2016). Association of complementary and alternative therapies with mental health outcomes in pregnant women living in a post-disaster recovery environment. Journal of Holistic Nursing,34, 259–270.
*Bittner, A., Peukert, J., Zimmermann, C., Junge-Hoffmeister, J., Parker, L. S., Stöbel-Richter, Y., et al. (2014). Early intervention in pregnant women with elevated anxiety and depressive symptoms: Efficacy of a cognitive-behavioral group program. The Journal of Perinatal and Neonatal Nursing,28, 185–195.
**Blair, L. M., Porter, K., Leblebicioglu, B., & Christian, L. M. (2015). Poor sleep quality and associated inflammation predict preterm birth: Heightened risk among African Americans. Sleep,38, 1259–1267.
Bödecs, T., Horváth, B., Szilágyi, E., Gonda, X., Rihmer, Z., & Sándor, J. (2011). Effects of depression, anxiety, self-esteem, and health behaviour on neonatal outcomes in a population-based Hungarian sample. European Journal of Obstetrics and Gynecology and Reproductive Biology,154, 45–50.
*Bolten, M. I., Wurmser, H., Buske-Kirschbaum, A., Papousek, M., Pirke, K. M., & Hellhammer, D. (2011). Cortisol levels in pregnancy as a psychobiological predictor for birth weight. Archives of Women’s Mental Health,14, 33–41.
*Borders, A. E., Lai, J. S., Wolfe, K., Qadir, S., Peng, J., Kim, K. Y., et al. (2017). Using item response theory to optimize measurement of chronic stress in pregnancy. Social Science Research,64, 214–225.
Brydges, C. R., Landes, J. K., Reid, C. L., Campbell, C., French, N., & Anderson, M. (2018). Cognitive outcomes in children and adolescents born very preterm: A meta-analysis. Developmental Medicine and Child Neurology,60, 452–468.
**Cannella, D., Auerbach, M., & Lobel, M. (2013). Predicting birth outcomes: Together, mother and health care provider know best. Journal of Psychosomatic Research,75, 299–304.
*Caparros-Gonzalez, R. A., Perra, O., Alderdice, F., Lynn, F., Lobel, M., García-García, I., & Peralta-Ramírez, M. I. (2019). Psychometric validation of the Prenatal Distress Questionnaire (PDQ) in pregnant women in Spain. Women & Health. https://doi.org/10.1080/03630242.2019.1584143.
*Caparros-Gonzalez, R. A., Romero-Gonzalez, B., Strivens-Vilchez, H., Gonzalez-Perez, R., Martinez-Augustin, O., & Peralta-Ramirez, M. I. (2017). Hair cortisol levels, psychological stress and psychopathological symptoms as predictors of postpartum depression. PLoS ONE,12, 1–17.
Carver, C. S., Scheier, M. F., & Segerstrom, S. C. (2010). Optimism. Clinical Psychology Review,30, 879–889.
*Chan, K. P. (2014). Effects of perinatal meditation on pregnant Chinese women in Hong Kong: A randomized controlled trial. Journal of Nursing Education and Practice,5, 1–18.
Christian, L. M. (2012). Psychoneuroimmunology in pregnancy: Immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neuroscience and Biobehavioral Reviews,36, 350–361.
**Christian, L. M., Iams, J. D., Porter, K., & Glaser, R. (2012). Epstein-barr virus reactivation during pregnancy and postpartum: Effects of race and racial discrimination. Brain, Behavior, and Immunity,26, 1280–1287.
**Christian, L. M., Iams, J., Porter, K., & Leblebicioglu, B. (2013). Self-rated health among pregnant women: Associations with objective health indicators, psychological functioning, and serum inflammatory markers. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine,46, 295–309.
**Cole-Lewis, H. J., Kershaw, T. S., Earnshaw, V. A., Yonkers, K. A., Lin, H., & Ickovics, J. R. (2014). Pregnancy-specific stress, preterm birth, and gestational age among high-risk young women. Health Psychology,33, 1033–1045.
Coussons-Read, M. E. (2012). The psychoneuroimmunology of stress in pregnancy. Current Directions in Psychological Science,21, 323–328.
Coussons-Read, M. E. (2013). Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstetric Medicine,6, 52–57.
**Coussons-Read, M. E., Lobel, M., Carey, J. C., Kreither, M. O., D’Anna, K., Argys, L., et al. (2012). The occurrence of preterm delivery is linked to pregnancy-specific distress and elevated inflammatory markers across gestation. Brain, Behavior, and Immunity,26, 650–659.
*Dias, L., & Lobel, M. (1997). Social comparison in medically high-risk pregnant women. Journal of Applied Social Psychology,27, 1629–1649.
DiPietro, J. A., Ghera, M. M., Costigan, K., & Hawkins, M. (2004). Measuring the ups and downs of pregnancy stress. Journal of Psychosomatic Obstetrics & Gynecology,25, 189–201.
DiPietro, J. A., Hilton, S. C., Hawkins, M., Costigan, K. A., & Pressman, E. K. (2002). Maternal stress and affect influence fetal neurobehavioral development. Developmental Psychology,38, 659–668.
Dominguez, T. P., Dunkel-Schetter, C., Glynn, L. M., Hobel, C., & Sandman, C. A. (2008). Racial differences in birth outcomes: The role of general, pregnancy, and racism stress. Health Psychology,27, 194–203.
*Draffin, C. R., Alderdice, F. A., McCance, D. R., Maresh, M., Harper, R., Patterson, C. C., et al. (2017). Impact of an educational DVD on anxiety and glycaemic control in women diagnosed with gestational diabetes mellitus (GDM): A randomised controlled trial. Diabetes Research and Clinical Practice,126, 164–171.
*Dukal, H., Frank, J., Lang, M., Treutlein, J., Gilles, M., Wolf, I. A., et al. (2015). New-born females show higher stress- and genotype-independent methylation of SLC6A4 than males. Borderline Personality Disorder and Emotion Dysregulation,2, 1–8.
Dunkel Schetter, C. (2011). Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology,62, 531–558.
Dunkel Schetter, C., & Glynn, L. M. (2010). Stress in pregnancy: Empirical evidence and theoretical issues to guide interdisciplinary research. In R. Contrada & A. Baum (Eds.), Handbook of stress (pp. 321–344). New York, NY: Springer.
**Earnshaw, V. A., Rosenthal, L., Lewis, J. B., Stasko, E. C., Tobin, J. N., Lewis, T. T., et al. (2013). Maternal experiences with everyday discrimination and infant birth weight: A test of mediators and moderators among young, urban women of color. Annals of Behavioral Medicine,45, 13–23.
*Faramarzi, M., & Pasha, H. (2018). Psychometric properties of the Persian version of the Prenatal Distress Questionnaire. Social Behavior and Personality: An International Journal,46, 815–822.
*Faramarzi, M., Yazdani, S., & Barat, S. (2015). A RCT of psychotherapy in women with nausea and vomiting of pregnancy. Human Reproduction,30, 2764–2773.
*Gennaro, S., Shults, J., & Garry, D. J. (2008). Stress and preterm labor and birth in Black women. Journal of Obstetric, Gynecologic, and Neonatal Nursing,37, 538–545.
**Giarratano, G., Harville, E. W., Barcelona de Mendoza, V., Savage, J., & Parent, C. M. (2015). Healthy Start: Description of a safety net for perinatal support during disaster recovery. Maternal and Child Health Journal,19, 819–827.
**Gillespie, S. L., Mitchell, A. M., Kowalsky, J. M., & Christian, L. M. (2018). Maternal parity and perinatal cortisol adaptation: The role of pregnancy-specific distress and implications for postpartum mood. Psychoneuroendocrinology,97, 86–93.
Giscombé, C. W., & Lobel, M. (2005). Explaining disproportionately high rates of adverse birth outcomes among African Americans: The impact of stress, racism, and related factors in pregnancy. Psychological Bulletin,131, 662–683.
Giurgescu, C., Penckofer, S., Maurer, M. C., & Bryant, F. B. (2006). Impact of uncertainty, social support, and prenatal coping on the psychological well-being of high-risk pregnant women. Nursing Research,55, 356–365.
Glynn, L. M., Wadhwa, P. D., Dunkel-Schetter, C., Chicz-DeMet, A., & Sandman, C. A. (2001). When stress happens matters: Effects of earthquake timing on stress responsivity in pregnancy. American Journal of Obstetrics and Gynecology,184, 637–642.
Greenberg, J., Solomon, S., Pyszczynski, T., Rosenblatt, A., Burling, J., Lyon, D., et al. (1992). Why do people need self-esteem? Converging evidence that self-esteem serves an anxiety-buffering function. Journal of Personality and Social Psychology,63, 913–922.
Guardino, C. M., & Dunkel Schetter, C. (2014). Coping during pregnancy: A systematic review and recommendations. Health Psychology Review,8, 70–94.
Guardino, C. M., Dunkel Schetter, C., Bower, J. E., Lu, M. C., & Smalley, S. L. (2014). Randomised controlled pilot trial of mindfulness training for stress reduction during pregnancy. Psychology & Health,29, 334–349.
*Haghparast, E., Faramarzi, M., & Hassanzadeh, R. (2016). Psychiatric symptoms and pregnancy distress in subsequent pregnancy after spontaneous abortion history. Pakistan Journal of Medical Sciences,32, 1097–1101.
**Hamilton, J. G., & Lobel, M. (2008). Types, patterns, and predictors of coping with stress during pregnancy: Examination of the revised Prenatal Coping Inventory in a diverse sample. Journal of Psychosomatic Obstetrics & Gynecology,29, 97–104.
**Harville, E. W., Giarratano, G., Savage, J., Barcelona de Mendoza, V., & Zotkiewicz, T. (2015). Birth outcomes in a disaster recovery environment: New Orleans women after Katrina. Maternal and Child Health Journal,19, 2512–2522.
*Hasanjanzadeh, P., & Faramarzi, M. (2017). Relationship between maternal general and specific-pregnancy stress, anxiety, and depression symptoms and pregnancy outcome. Journal of Clinical and Diagnostic Research,11, VC04–VC07.
*Haselbeck, C., Niederberger, U., Kulle, A., Wache, K., Brauner, E., Gutermuth, M., et al. (2017). Prenatal maternal distress seems to be associated with the infant’s temperament and motor development: An explorative study. Journal of Neural Transmission,124, 881–890.
Heaman, M., Kingston, D., Chalmers, B., Sauve, R., Lee, L., & Young, D. (2013). Risk factors for preterm birth and small-for-gestational-age births among Canadian women. Paediatric and Perinatal Epidemiology,27, 54–61.
**Heberlein, E. C., Picklesimer, A. H., Billings, D. L., Covington-Kolb, S., Farber, N., & Frongillo, E. A. (2015). The comparative effects of group prenatal care on psychosocial outcomes. Archives of Women’s Mental Health,19, 259–269.
Hedegaard, M., Henriksen, T. B., Sabroe, S., & Secher, N. J. (1993). Psychological distress in pregnancy and preterm delivery. British Medical Journal,307, 234–239.
*Heery, E., Kelleher, C. C., Wall, P. G., & McAuliffe, F. M. (2014). Prediction of gestational weight gain—A biopsychosocial model. Public Health Nutrition,18, 1488–1498.
*Heery, E., Wall, P. G., Kelleher, C. C., & McAuliffe, F. M. (2016). Effects of dietary restraint and weight gain attitudes on gestational weight gain. Appetite,107, 501–510.
Hogue, C. J. R., Hoffman, S., & Hatch, M. C. (2001). Stress and preterm delivery: A conceptual framework. Paediatric and Perinatal Epidemiology,15, 30–40.
Huizink, A. C., Mulder, E. J., Robles de Medina, P. G., Visser, G. H., & Buitelaar, J. K. (2004). Is pregnancy anxiety a distinctive syndrome? Early Human Development,79, 81–91.
**Hux, V. J., Roberts, J. M., & Okun, M. L. (2017). Allostatic load in early pregnancy is associated with poor sleep quality. Sleep Medicine,33, 85–90.
**Ibrahim, S. M., Nicoloro-SantaBarbara, J., Auerbach, M. V., Rosenthal, L., Kocis, C., Busso, C. E., & Lobel, M. (2019). Pregnancy-specific coping and changes in emotional distress from mid-to late pregnancy. Journal of Reproductive and Infant Psychology. https://doi.org/10.1080/02646838.2019.1578871.
**Ickovics, J. R., Kershaw, T. S., Westdahl, C., Magriples, U., Massey, Z., Reynolds, H., et al. (2007). Group prenatal care and perinatal outcomes: A randomized controlled trial. Obstetrics and Gynecology,110, 330–339.
Jesse, D. E., Seaver, W., & Wallace, D. C. (2003). Maternal psychosocial risks predict preterm birth in a group of women from Appalachia. Midwifery,19, 191–202.
**Kennedy, H. P., Farrell, T., Paden, R., Hill, S., Jolivet, R. R., Cooper, B. A., et al. (2011). A randomized clinical trial of group prenatal care in two military settings. Military Medicine,176, 1169–1177.
Khashan, A. S., McNamee, R., Abel, K. M., Mortensen, P. B., Kenny, L. C., Pedersen, M. G., et al. (2009). Rates of preterm birth following antenatal maternal exposure to severe life events: A population-based cohort study. Human Reproduction,24, 429–437.
**Kim, Y., & Chung, C. W. (2017). Development of the Korean pregnancy stress scale. Japan Journal of Nursing Science,15, 113–124.
*Koletzko, S. H., La Marca-Ghaemmaghami, P., & Brandstätter, V. (2015). Mixed expectations: Effects of goal ambivalence during pregnancy on maternal well-being, stress, and coping. Applied Psychology: Health and Well-Being,7, 249–274.
Lederman, S. A., Rauh, V., Weiss, L., Stein, J. L., Hoepner, L. A., Becker, M., et al. (2004). The effects of the World Trade Center event on birth outcomes among term deliveries at three lower Manhattan hospitals. Environmental Health Perspectives,112, 1772–1778.
*Levine, T. A., Grunau, R. E., Segurado, R., Daly, S., Geary, M. P., Kennelly, M. M., et al. (2017). Pregnancy-specific stress, fetoplacental haemodynamics, and neonatal outcomes in women with small for gestational age pregnancies: A secondary analysis of the multicentre prospective observational trial to optimise paediatric health in intrauterine growth restriction. British Medical Journal Open,7, 1–12.
Littleton, H. L., Breitkopf, C. R., & Berenson, A. B. (2007). Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: A meta-analysis. American Journal of Obstetrics and Gynecology,196, 424–432.
Lobel, M. (1994). Conceptualizations, measurement, and effects of prenatal maternal stress on birth outcomes. Journal of Behavioral Medicine,17, 225–272.
Lobel, M. (1998). Pregnancy and mental health. In H. Friedman (Ed.), Encyclopedia of mental health (pp. 229–238). San Diego, CA: Academic Press.
**Lobel, M., Cannella, D. L., Graham, J. E., DeVincent, C., Schneider, J., & Meyer, B. A. (2008). Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology,27, 604–615.
Lobel, M., & DeLuca, R. S. (2007). Psychosocial sequelae of cesarean delivery: Review and analysis of their causes and implications. Social Science and Medicine,64, 2272–2284.
*Lobel, M., DeVincent, C. J., Kaminer, A., & Meyer, B. A. (2000). The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychology,19, 544–553.
Lobel, M., & Dunkel Schetter, C. (2016). Pregnancy and prenatal stress. In H. S. Friedman (Ed.), Encyclopedia of mental health (2nd ed., pp. 318–329). Waltham, MA: Academic Press.
Lobel, M., Hamilton, J. G., & Cannella, D. T. (2008). Psychosocial perspectives on pregnancy: Prenatal maternal stress and coping. Social and Personality Psychology Compass,2, 1600–1623.
*Lynn, F. A., Alderdice, F. A., Crealey, G. E., & McElnay, J. C. (2011). Associations between maternal characteristics and pregnancy-related stress among low-risk mothers: An observational cross-sectional study. International Journal of Nursing Studies,48, 620–627.
*Lynn, F. A., Crealey, G. E., Alderdice, F. A., & McElnay, J. C. (2013). Preferences for a third-trimester ultrasound scan in a low-risk obstetric population: A discrete choice experiment. Health Expectations: An International Journal of Public Participation in Health Care & Health Policy,18, 892–903.
**Magriples, U., Boynton, M. H., Kershaw, T. S., Lewis, J., Rising, S. S., Tobin, J. N., et al. (2015). The impact of group prenatal care on pregnancy and postpartum weight trajectories. American Journal of Obstetrics and Gynecology,213, 688.e1–688.e9.
**Magriples, U., Boynton, M. H., Kershaw, T. S., Rising, S. S., & Ickovics, J. R. (2013). Blood pressure changes during pregnancy: Impact of race, body mass index, and weight gain. American Journal of Perinatology,30, 415–424.
**Magriples, U., Kershaw, T. S., Rising, S. S., Massey, Z., & Ickovics, J. R. (2008). Prenatal health care beyond the obstetrics service: Utilization and predictors of unscheduled care. American Journal of Obstetrics and Gynecology,198, 75.e1–75.e7.
Mahaffey, B., & Lobel, M. (2019). Mental health and emotional distress during pregnancy. In T. A. Revenson & R. A. R. Gurung (Eds.), Handbook of health psychology. New York, NY: Taylor & Francis.
*Matvienko-Sikar, K., & Dockray, S. (2017). Effects of a novel positive psychological intervention on prenatal stress and well-being: A pilot randomised controlled trial. Women and Birth,30, e111–e118.
*McCormack, D., Scott-Heyes, G., & McCusker, C. G. (2011). The impact of hyperemesis gravidarum on maternal mental health and maternal–fetal attachment. Journal of Psychosomatic Obstetrics & Gynecology,32, 79–87.
Misra, D. P., O’campo, P., & Strobino, D. (2001). Testing a sociomedical model for preterm delivery. Paediatric and Perinatal Epidemiology,15, 110–122.
**Mitchell, A. M., & Christian, L. M. (2017). Financial strain and birth weight: The mediating role of psychological distress. Archives of Women’s Mental Health,20, 201–208.
**Mitchell, A. M., Kowalsky, J. M., Epel, E. S., Lin, J., & Christian, L. M. (2017). Childhood adversity, social support, and telomere length among perinatal women. Psychoneuroendocrinology,87, 43–52.
Mokkink, L. B., Terwee, C. B., Patrick, D. L., Alonso, J., Stratford, P. W., Knol, D. L., et al. (2010). The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Quality of Life Research,19, 539–549.
*Monk, C., Feng, T., Lee, S., Krupska, I., Champagne, F. A., & Tycko, B. (2016). Distress during pregnancy: Epigenetic regulation of placenta glucocorticoid-related genes and fetal neurobehavior. The American Journal of Psychiatry,173, 705–713.
*Moog, N. K., Entringer, S., Rasmussen, J. M., Styner, M., Gilmore, J. H., Kathmann, N., et al. (2017). Intergenerational effect of maternal exposure to childhood maltreatment on newborn brain anatomy. Biological Psychiatry,3, 120–127.
Mürner-Lavanchy, I. M., & Anderson, P. J. (2018). Developmental disorders among very preterm children. Current Developmental Disorders Reports,5, 1–9.
**Okun, M. L., Kline, C. E., Roberts, J. M., Wettlaufer, B., Glover, K., & Hall, M. (2013). Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. Journal of Women’s Health,22, 1028–1037.
*Omidvar, S., Faramarzi, M., Hajian-Tilak, K., & Amiri, F. N. (2018). Associations of psychosocial factors with pregnancy healthy life styles. PLoS ONE,13, 1–13.
*Pluess, M., Bolten, M., Pirke, K.-M., & Hellhammer, D. (2010). Maternal trait anxiety, emotional distress, and salivary cortisol in pregnancy. Biological Psychology,83, 169–175.
*Richter, J., Bittner, A., Petrowski, K., Junge-Hoffmeister, J., Bergmann, S., Joraschky, P., et al. (2012). Effects of an early intervention on perceived stress and diurnal cortisol in pregnant women with elevated stress, anxiety, and depressive symptomatology. Journal of Psychosomatic Obstetrics & Gynecology,33, 162–170.
*Rieger, M., Pirke, K.-M., Buske-Kirschbaum, A., Wurmser, H., Papoušek, M., & Hellhammer, D. H. (2004). Influence of stress during pregnancy on HPA activity and neonatal behavior. Annals of the New York Academy of Sciences,1032, 228–230.
Rini, C. K., Dunkel-Schetter, C., Sandman, C. A., & Wadhwa, P. D. (1999). Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychology,18, 333–345.
Roesch, S. C., Schetter, C. D., Woo, G., & Hobel, C. J. (2004). Modeling the types and timing of stress in pregnancy. Anxiety, Stress & Coping: An International Journal,17, 87–102.
*Romero-Gonzalez, B., Caparros-Gonzalez, R. A., Gonzalez-Perez, R., Delgado-Puertas, P., & Peralta-Ramirez, M. I. (2018). Newborn infants’ hair cortisol levels reflect chronic maternal stress during pregnancy. PLoS ONE,13, 1–13.
**Rosenthal, L., Earnshaw, V. A., Moore, J. M., Ferguson, D. N., Lewis, T. T., Reid, A. E., et al. (2018). Intergenerational consequences: Women’s experiences of discrimination in pregnancy predict infant social-emotional development at 6 months and 1 year. Journal of Developmental and Behavioral Pediatrics,39, 228–237.
Rosenthal, L., & Lobel, M. (2011). Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social Science and Medicine,72, 977–983.
**Rosenthal, L., & Lobel, M. (2018). Gendered racism and the sexual and reproductive health of Black and Latina women. Ethnicity and Health. https://doi.org/10.1080/13557858.2018.1439896.
*Ross, K. M., Miller, G., Qadir, S., Keenan-Devlin, L., Leigh, A. K. K., & Borders, A. (2017). Close relationship qualities and maternal peripheral inflammation during pregnancy. Psychoneuroendocrinology,77, 252–260.
*Ruhstaller, K. E., Elovitz, M. A., Stringer, M., Epperson, C. N., & Durnwald, C. P. (2017). Obesity and the association with maternal mental health symptoms. The Journal of Maternal-Fetal & Neonatal Medicine,30, 1897–1901.
Saigal, S., & Doyle, L. W. (2008). An overview of mortality and sequelae of preterm birth from infancy to adulthood. The Lancet,371, 261–269.
**Saunders, T. A., Lobel, M., Veloso, C., & Meyer, B. A. (2006). Prenatal maternal stress is associated with delivery analgesia and unplanned cesareans. Journal of Psychosomatic Obstetrics & Gynecology,27, 141–146.
*Schoch-Ruppen, J., Ehlert, U., Uggowitzer, F., Weymerskirch, N., & La Marca-Ghaemmaghami, P. (2018). Women’s word use in pregnancy: Associations with maternal characteristics, prenatal stress, and neonatal birth outcome. Frontiers in Psychology,9, 1–14.
*Schredl, M., Gilles, M., Wolf, I., Peus, V., Scharnholz, B., Sütterlin, M., et al. (2016). Nightmare frequency in last trimester of pregnancy. BMC Pregnancy and Childbirth,16, 346–352.
*Send, T. S., Gilles, M., Codd, V., Wolf, I., Bardtke, S., Streit, F., et al. (2017). Telomere length in newborns is related to maternal stress during pregnancy. Neuropsychopharmacology,42, 2407–2413.
*Simon, C. D., Adam, E. K., Holl, J. L., Wolfe, K. A., Grobman, W. A., & Borders, A. E. B. (2016). Prenatal stress and the cortisol awakening response in African–American and Caucasian women in the third trimester of pregnancy. Maternal and Child Health Journal,20, 2142–2149.
*Singh, A., Trumpff, C., Genkinger, J., Davis, A., Spann, M., Werner, E., et al. (2017). Micronutrient dietary intake in Latina pregnant adolescents and its association with level of depression, stress, and social support. Nutrients,9, 1–16.
Souza, A. C. D., Alexandre, N. M. C., & Guirardello, E. D. B. (2017). Psychometric properties in instruments evaluation of reliability and validity. Epidemiologia e Serviços de Saúde,26, 649–659.
**Staneva, A., Morawska, A., Bogossian, F., & Wittkowski, A. (2016). Pregnancy-specific distress: The role of maternal sense of coherence and antenatal mothering orientations. Journal of Mental Health,25, 387–394.
**Staneva, A. A., Morawska, A., Bogossian, F., & Wittkowski, A. (2017). Maternal psychological distress during pregnancy does not increase the risk for adverse birth outcomes. Women and Health,58, 92–111.
Stein, A., Pearson, R. M., Goodman, S. H., Rapa, E., Rahman, A., McCallum, M., et al. (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet,384, 1800–1819.
*Talley, P., Heitkemper, M., Chicz-Demet, A., & Sandman, C. A. (2006). Male violence, stress, and neuroendocrine parameters in pregnancy: A pilot study. Biological Research for Nursing,7, 222–233.
Terwee, C. B., Bot, S. D., de Boer, M. R., van der Windt, D. A., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology,60, 34–42.
Torche, F., & Kleinhaus, K. (2012). Prenatal stress, gestational age and secondary sex ratio: The sex-specific effects of exposure to a natural disaster in early pregnancy. Human Reproduction,27, 558–567.
Vieten, C., & Astin, J. (2008). Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Archives of Women’s Mental Health,11, 67–74.
**Walsh, K., Basu, A., Werner, E., Lee, S., Feng, T., Osborne, L. M., et al. (2016). Associations among child abuse, depression, and interleukin-6 in pregnant adolescents: Paradoxical findings. Psychosomatic Medicine,78, 920–930.
*White, O., McCorry, N. K., Scott-Heyes, G., Dempster, M., & Manderson, J. (2008). Maternal appraisals of risk, coping and prenatal attachment among women hospitalised with pregnancy complications. Journal of Reproductive and Infant Psychology,26, 74–85.
*Williams, P. H., & Oravecz, L. M. (2016). University-community collaboration to promote healthy mothers and infants: The Relationships and Parenting Support (RAPS) program. Journal of Higher Education Outreach and Engagement,20, 164–183.
**Woods-Giscombé, C. L., Lobel, M., & Crandell, J. L. (2010). The impact of miscarriage and parity on patterns of maternal distress in pregnancy. Research in Nursing & Health,33, 316–328.
World Health Organization. (2016). Standards for improving quality of maternal and newborn care in health facilities. Geneva. Retrieved May 25, 2018 from http://www.who.int/maternal_child_adolescent/documents/improving-maternal-newborn-care-quality/en/.
*Yali, A. M., & Lobel, M. (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics & Gynecology,20, 39–52.
**Yali, A. M., & Lobel, M. (2002). Stress-resistance resources and coping in pregnancy. Anxiety, Stress & Coping: An International Journal,15, 289–309.
Ye, J., Zhang, J., Mikolajczyk, R., Torlino, M. R., Gulmezoglu, A. M., & Betran, A. P. (2016). Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG,123, 745–753.
**Yuksel, F., Akin, S., & Durna, Z. (2013). Prenatal distress in Turkish pregnant women and factors associated with maternal prenatal distress. Journal of Clinical Nursing,23, 54–64.
Zimmer-Gembeck, M. J., & Skinner, E. A. (2016). The development of coping: Implications for psychopathology and resilience. In D. Cicchetti (Ed.), Developmental psychopathology: Risk, resilience, and intervention (3rd ed., Vol. 4, pp. 485–545). New York, NY: Wiley.
Funding
The first author (SI) received support from the Dr. W. Burghardt Turner Fellowship program during work on this project. No other funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and Informed consent
This article does not contain any studies with human participants or animals performed by either of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ibrahim, S.M., Lobel, M. Conceptualization, measurement, and effects of pregnancy-specific stress: review of research using the original and revised Prenatal Distress Questionnaire. J Behav Med 43, 16–33 (2020). https://doi.org/10.1007/s10865-019-00068-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-019-00068-7