Abstract
Electrospun scaffolds of silk fibroin (SF) and poly(lactide-co-glycolide) (PLGA) were prepared to mimic the morphology and chemistry of the extracellular matrix. The SF/PLGA scaffolds were treated with ethanol to improve their usability. After ethanol treatment the scaffolds exhibited a smooth surface and uniform fibers. SF transformed from random coil conformation to β-sheet structure after ethanol treatment, so that the SF/PLGA scaffolds showed low hydrophilicity and dissolving rate in water. The mechanical properties and the hydrophilicity of the blended fibrous scaffolds were affected by the weight ratio of SF and PLGA. During degradation of ethanol-treated SF/PLGA scaffolds in vitro, the fibers became thin along with the degradation time. Human umbilical vein endothelial cells (HUVECs) were seeded onto the ethanol-treated nanofibrous scaffolds for cell viability, attachment and morphogenesis studies. These SF/PLGA scaffolds could enhance the viability, spreading and attachment of HUVECs. Based on these results, these ethanol-treated scaffolds are proposed to be a good candidate for endothelial cell growth.











Similar content being viewed by others
References
Borcard FO, Staedler D, Comas H, Juillerat FK, Sturzenegger PN, Heuberger R, Gonzenbach UT, Juillerat-Jeanneret L, Gerber-Lemaire S. Chemical functionalization of bioceramics to enhance endothelial cells adhesion for tissue engineering. J Med Chem. 2012;55:7988–97.
Langer R, Tirrell DA. Designing materials for biology and medicine. Nature. 2004;428:487–92.
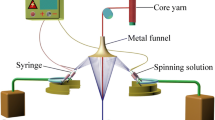
Li L, Li H, Qian Y, Li X, Singh GK, Zhong L, Liu W, Lv Y, Cai K, Yang L. Electrospun poly(ε-caprolactone)/silk fibroin core-sheath nanofibers and their potential applications in tissue engineering and drug release. Int J Biol Macromol. 2011;49:223–32.
Kai D, Jin G, Prabhakaran MP, Ramakrishna S. Electrospun synthetic and natural nanofibers for regenerative medicine and stem cells. J Biotechnol. 2013;8:59–72.
Xu C, Inai R, Kotaki MS, Ramakrishna S. Aligned biodegradable nanofibrous structure: a potential scaffold for blood vessel engineering. Biomaterials. 2004;25:877–86.
Yuan W, Feng Y, Wang H, Yang D, An B, Zhang W, Khan M, Guo J. Hemocompatible surface of electrospun nanofibrous scaffolds by ATRP modification. Mater Sci Eng C Mater Biol Appl. 2013;33:3644–51.
Alsberg E, Feinstein E, Joy MP, Prentiss M, Ingber DE. Magnetically-guided self-assembly of fibrin matrices with ordered nano-scale structure for tissue engineering. Tissue Eng. 2006;12:3247–56.
Wang H, Feng Y, An B, Zhang W, Sun M, Fang Z, Yuan W, Khan M. Fabrication of PU/PEGMA crosslinked hybrid scaffolds by in situ UV photopolymerization favoring human endothelial cells growth for vascular tissue engineering. J Mater Sci Mater Med. 2012;23:1499–510.
Wang H, Feng Y, Behl M, Lendlein A, Zhao H, Xiao R, Lu J, Zhang L, Guo J. Hemocompatible polyurethane/gelatin–heparin nanofibrous scaffolds formed by a bi-layer electrospinning technique as potential artificial blood vessels. Front Chem Sci Eng. 2011;5:392–400.
Wang H, Feng Y, Fang Z, Yuan W, Khan M. Co-electrospun blends of PU and PEG as potential biocompatible scaffolds for small-diameter vascular tissue engineering. Mater Sci Eng C Mater Biol Appl. 2012;32:2306–15.
Wang H, Feng Y, Zhao H, Xiao R, Lu J, Zhang L, Guo J. Electrospun hemocompatible PU/gelatin–heparin nanofibrous bilayer scaffolds as potential artificial blood vessels. Macromol Res. 2012;20:347–50.
Yoshimoto H, Shin Y, Terai H, Vacanti JP. A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials. 2003;24:2077–82.
Meinel L, Hofmann S, Karageorgiou V, Kirker-Head C, McCool J, Gronowicz G, Zichner L, Langer R, Vunjak-Novakovic G, Kaplan DL. The inflammatory responses to silk films in vitro and in vivo. Biomaterials. 2005;26:147–55.
Motta A, Migliaresi C, Faccioni F, Torricelli P, Fini M, Giardino R. Fibroin hydrogels for biomedical applications: preparation, characterization and in vitro cell culture studies. J Biomater Sci Polym Ed. 2004;15:851–64.
Zhang YQ, Zhou WL, Shen WD, Chen YH, Zha XM, Shirai K, Kiguchi K. Synthesis, characterization and immunogenicity of silk fibroin-l-asparaginase bioconjugates. J Biotechnol. 2005;120:315–26.
Guziewicz N, Best A, Perez-Ramirez B, Kaplan DL. Lyophilized silk fibroin hydrogels for the sustained local delivery of therapeutic monoclonal antibodies. Biomaterials. 2011;32:2642–50.
Shahverdi S, Hajimiri M, Esfandiari MA, Larijani B, Atyabi F, Rajabiani A, Dehpour AR, Gharehaghaji AA, Dinarvand R. Fabrication and structure analysis of poly(lactide-co-glycolic acid)/silk fibroin hybrid scaffold for wound dressing applications. Int J Pharm. 2014;473:345–55.
Marelli B, Alessandrino A, Farè S. Compliant electrospun silk fibroin tubes for small vessel bypass grafting. Acta Biomater. 2010;6:4019–26.
Liu S, Dong C, Lu G. Bilayered vascular grafts based on silk proteins. Acta Biomater. 2013;9:8991–9003.
Nakazawa Y, Sato M, Takahashi R, Aytemiz D, Takabayashi C, Tamura T, Enomoto S, Sata M, Asakura T. Development of small-diameter vascular grafts based on silk fibroin fibers from Bombyx mori for vascular regeneration. J Biomater Sci Polym Ed. 2011;22:195–206.
Lovett M, Cannizzaro C, Daheron L, Messmer B, Vunjak-Novakovic G, Kaplan DL. Silk fibroin microtubes for blood vessel engineering. Biomaterials. 2007;28:5271–9.
Soffer L, Wang X, Zhang X, Kluge J, Dorfmann L, Kaplan DL, Leisk G. Silk-based electrospun tubular scaffolds for tissue engineered vascular grafts. J Biomater Sci Ploym Ed. 2008;19:653–64.
Zhang XH, Baughman CB, Kaplan DL. In vitro evaluation of electrospun silk fibroin scaffolds for vascular cell growth. Biomaterials. 2008;29:2217–27.
Zhang X, Wang X, Keshav V, Wang X, Johanas JT, Leisk GG, Kaplan DL. Dynamic culture conditions to generate silk-based tissue-engineered vascular grafts. Biomaterials. 2009;30:3213–23.
Wang S, Zhang Y, Wang H, Yin G, Dong Z. Fabrication and properties of the electrospun polylactide/silk fibroin–gelatin composite tubular scaffold. Biomacromolecules. 2009;10:2240–4.
Liu X, Zhang C, Xu W, Liu H, Ouyang C. Blend films of silk fibroin and water-insoluble polyurethane prepared from an ionic liquid. Mater Lett. 2011;65:2489–91.
Stoppato M, Stevens HY, Carletti E, Migliaresi C, Motta A, Guldberg RE. Effects of silk fibroin fiber incorporation on mechanical properties, endothelial cell colonization and vascularization of PDLLA scaffolds. Biomaterials. 2013;34:4573–81.
Wenk E, Meinel AJ, Wildy S, Merkle HP, Meinel L. Microporous silk fibroin scaffolds embedding PLGA microparticles for controlled growth factor delivery in tissue engineering. Biomaterials. 2009;30:2571–81.
Zhou S, Peng H, Yu X, Zheng X, Cui W, Zhang Z, Li X, Wang J, Weng J, Jia W, Li F. Preparation and characterization of a novel electrospun spider silk fibroin/poly(d,l-lactide) composite fiber. J Phys Chem B. 2008;112:11209–16.
Li S, Wu H, Hu XD, Tu CQ, Pei FX, Wang GL, Lin W, Fan HS. Preparation of electrospun PLGA–silk fibroin nanofibers-based nerve conduits and evaluation in vivo. Artif Cell Blood Substit Immobil Biotechnol. 2012;40:171–8.
McClure M, Sell S, Ayres C, Simpson DG, Bowlin GL. Electrospinning-aligned and random polydioxanone–polycaprolactone–silk fibroin-blended scaffolds: geometry for a vascular matrix. Biomed Mater. 2009;4:055010.
Zhang K, Wang H, Huang C, Su Y, Mo X, Ikada Y. Fabrication of silk fibroin blended P(LLA-CL) nanofibrous scaffolds for tissue engineering. J Biomed Mater Res A. 2010;93:984–93.
Liu H, Xu W, Zou H, Ke G, Li W, Ouyang C. Feasibility of wet spinning of silk-inspired polyurethane elastic biofiber. Mater Lett. 2008;62:1949–52.
Jin HJ, Fridrikh SV, Rutledge GC, Kaplan DL. Electrospinning Bombyx mori silk with poly(ethylene oxide). Biomacromolecules. 2002;3:1233–9.
Horst M, Milleret V, Nötzli S, Madduri S, Sulser T, Gobet R, Eberli D. Increased porosity of electrospun hybrid scaffolds improved bladder tissue regeneration. J Biomed Mater Res A. 2014;102:2116–24.
Zhang JG, Mo XM. Current research on electrospinning of silk fibroin and its blends with natural and synthetic biodegradable polymers. Front Mater Sci. 2013;7:1–14.
Ju HW, Sheikh FA, Moon BM, Park HJ, Lee OJ, Kim JH, Eun JJ, Khang G, Park CH. Fabrication of poly(lactic-co-glycolic acid) scaffolds containing silk fibroin scaffolds for tissue engineering applications. J Biomed Mater Res A. 2014;102:2713–24.
Hasan A, Memic A, Annabi N, Hossain M, Paul A, Dokmeci MR, Dehghani F, Khademhosseini A. Electrospun scaffolds for tissue engineering of vascular grafts. Acta Biomater. 2014;10:11–25.
Farokhi M, Mottaghitalab F, Shokrgozar MA, Ai J, Hadjati J, Azami M. Bio-hybrid silk fibroin/calcium phosphate/PLGA nanocomposite scaffold to control the delivery of vascular endothelial growth factor. Mater Sci Eng C Mater Biol Appl. 2014;35:401–10.
Gandhimathi C, Venugopal J, Ramakrishna S, Tay S, Kumar S. Biomimetic porous tetracycline loaded PLGA/Silk Fibroin/Ascorbic acid/n-HA hybrid scaffolds for adipose derived stem cells differentiation into osteogenic lineage (LB32). FASEB J. 2014;28(1), Supplement LB32.
Wang SD, Zhang YZ. Preparation, structure and in vitro degradation behavior of the electrospun poly(lactide-co-glycolide) ultrafine fibrous vascular scaffold. Fiber Polym. 2012;13(6):754–61.
Vaz CM, van Tuijl S, Bouten CVC. Design of scaffolds for blood vessel tissue engineering using a multi-layering electrospinning technique. Acta Biomater. 2005;1:575–82.
Wang CY, Zhang KH, Fan CY, Mo XM, Ruan HJ, Li FF. Aligned natural-synthetic polyblend nanofibers for peripheral nerve regeneration. Acta Biomater. 2011;7:634–43.
Um IC, Kweon H, Park YH, Hudson S. Structural characteristics and properties of the regenerated silk fibroin prepared from formic acid. Int J Biol Macromol. 2001;29:91–7.
Jin HJ, Kaplan DL. Mechanism of silk processing in insects and spiders. Nature. 2003;424:1057–61.
Lu Q, Hu X, Wang X, Kluge JA, Lu S, Cebe P, Kaplan DL. Water-insoluble silk films with silk I structure. Acta Biomater. 2010;6:1380–7.
Sell SA, McClure MJ, Barnes CP. Electrospun polydioxanone–elastin blends: potential for bioresorbable vascular grafts. Biomed Mater. 2006;1:72–80.
Ertel SI, Ratner BD, Horbett TA. Radiofrequency plasma deposition of oxygen-containing films on polystyrene and poly(ethylene terephthalate) substrates improves endothelial cell growth. J Biomed Mater Res. 1990;24:1637–59.
Wang YQ, Cai JY. Enhanced cell affinity of poly(l-lactic acid) modified by base hydrolysis: wettability and surface roughness at nanometer scale. Curr Appl Phys. 2007;7:e108–11.
Lee JH, Lee SJ, Khang G, Lee HB. The effect of fluid shear stress on endothelial cell adhesiveness to polymer surfaces with wettability gradient. J Colloid Interface Sci. 2000;230:84–90.
Wachem PV, Beugeling T, Feijen J, Bantjes A, Detmers JP, van Aken WG. Interaction of cultured human endothelial cells with polymeric surfaces of different wettabilities. Biomaterials. 1985;6:403–8.
Acknowledgments
This project was supported by the National Natural Science Foundation of China (Grant No. 31370969), the International Cooperation from Ministry of Science and Technology of China (Grant No. 2013DFG52040, 2008DFA51170), Ph.D. Programs Foundation of Ministry of Education of China (No. 20120032110073) and the Program of Introducing Talents of Discipline to Universities of China (No. B06006).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhou, W., Feng, Y., Yang, J. et al. Electrospun scaffolds of silk fibroin and poly(lactide-co-glycolide) for endothelial cell growth. J Mater Sci: Mater Med 26, 56 (2015). https://doi.org/10.1007/s10856-015-5386-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-015-5386-6