Abstract
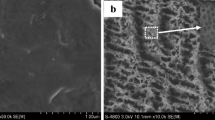
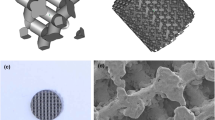
Porous titanium with appropriate surface treatments can be osteoinductive. To investigate the effect of surface treatments of porous titanium on the attachment and differentiation of mesenchymal stem cells (MSCs), two kinds of surface microstructured porous titaniums, H2O2/TaCl5 treated one (HTPT), and H2O2/TaCl5 and subsequent simulated body fluid (SBF) treated one (STPT) were fabricated, and non-treated one (NTPT) was used as control. The morphology, specific surface area (SSA), pore distribution and mechanical strength of these materials were characterized respectively, and the results showed that H2O2/TaCl5 treatment led to a significant increase in both SSA and micropores of HTPT, and the further SBF immersion resulted in the formation of a layer of bone-like apatite on the surface of STPT. Although the surface treatments had a little negative impact on the compressive strength and elasticity modulus of porous titanium, the mechanical strength of HTPT or STPT was enough for the bone defect repair of the load-bearing sites. The protein adsorption and cell adhesion experiments confirmed that the microstructured surface notably enhanced porous titanium’s protein binding capacity and promoted MSCs adhesion on the surface. More importantly, cell differentiation experiments proved that the microstructured surface evidently elevated the osteoblastic gene expressions of MSCs compared to NTPT. The enhanced biological effect by the surface treatments was more robust on STPT. Therefore, our results suggest that the microstructured surface has great potential for promoting MSCs differentiation towards osteoblasts, giving excellent support for the osteoinduction of porous titanium with appropriate surface treatments.






Similar content being viewed by others
References
Geetha M, Singh AK, Asokamani R, Gogia AK. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog Mater Sci. 2009;54:397–425.
Liu X, Chu PK, Ding C. Surface modification of titanium, titanium alloys, and related materials for biomedical applications. Mater Sci Eng R Rep. 2004;47:49–121.
Froimson MI, Garino J, Machenaud A, Vidalain JP. Minimum 10-year results of a tapered, titanium, hydroxyapatite-coated hip stem: an independent review. J Arthroplast. 2007;22:1–7.
Weinans H, Huiskes R, Grootenboer HJ. Effects of material properties of femoral hip components on bone remodeling. J Orthop Res. 1992;10:845–53.
Krishna BV, Bose S, Bandyopadhyay A. Low stiffness porous Ti structures for load-bearing implants. Acta Biomater. 2007;3:997–1006.
Imwinkelried T. Mechanical properties of open-pore titanium foam. J Biomed Mater Res Part A. 2007;81A:964–70.
Chen YJ, Feng B, Zhu YP, Weng J, Wang JX, Lu X. Fabrication of porous titanium implants with biomechanical compatibility. Mater Lett. 2009;63:2659–61.
Li H, Fan HS, Zhang XD. Fabrication of porous titanium with biomechanical compatibility. Key Eng Mater. 2005;288:611–4.
Li JP, Habibovic P, van den Doel M, Wilson CE, de Wijn JR, van Blitterswijk CA, et al. Bone ingrowth in porous titanium implants produced by 3D fiber deposition. Biomaterials. 2007;28:2810–20.
Otsuki B, Takemoto M, Fujibayashi S, Neo M, Kokubo T, Nakamura T. Pore throat size and connectivity determine bone and tissue ingrowth into porous implants: three-dimensional micro-CT based structural analyses of porous bioactive titanium implants. Biomaterials. 2006;27:5892–900.
Bobyn J, Pilliar R, Cameron H, Weatherly G. The optimum pore size for the fixation of porous-surfaced metal implants by the ingrowth of bone. Clin Orthop. 1980;150:263–70.
Ryan G, Pandit A, Apatsidis DP. Fabrication methods of porous metals for use in orthopaedic applications. Biomaterials. 2006;27:2651–70.
Xue W, Krishna BV, Bandyopadhyay A, Bose S. Processing and biocompatibility evaluation of laser processed porous titanium. Acta Biomater. 2007;3:1007–18.
Traini T, Mangano C, Sammons RL, Mangano F, Macchi A, Piattelli A. Direct laser metal sintering as a new approach to fabrication of an isoelastic functionally graded material for manufacture of porous titanium dental implants. Dent Mater. 2008;24:1525–33.
Yook S-W, Kim H-E, Koh Y-H. Fabrication of porous titanium scaffolds with high compressive strength using camphene-based freeze casting. Mater Lett. 2009;63:1502–4.
Ryan GE, Pandit AS, Apatsidis DP. Porous titanium scaffolds fabricated using a rapid prototyping and powder metallurgy technique. Biomaterials. 2008;29:3625–35.
Zhao CY, Li H, Yuan T, Fan HS, Zhang XD, Gu ZW. A comparative study of porous titanium with different surface modification implanted in dogs. Key Eng Mater. 2007;342:561–4.
Zhao CY, Zhu XD, Yuan T, Fan HS, Zhang XD. Fabrication of biomimetic apatite coating on porous titanium and their osteointegration in femurs of dogs. Mater Sci Eng C. 2010;30:98–104.
Fukuda A, Takemoto M, Saito T, Fujibayashi S, Neo M, Pattanayak DK, et al. Osteoinduction of porous Ti implants with a channel structure fabricated by selective laser melting. Acta Biomater. 2011;7:2327–36.
Habibovic P, Li J, van der Valk CM, Meijer G, Layrolle P, van Blitterswijk CA, et al. Biological performance of uncoated and octacalcium phosphate-coated Ti6Al4V. Biomaterials. 2005;26:23–36.
Fujibayashi S, Neo M, Kim H-M, Kokubo T, Nakamura T. Osteoinduction of porous bioactive titanium metal. Biomaterials. 2004;25:443–50.
Zhao C, Zhu X, Liang K, Ding J, Xiang Z, Fan H, et al. Osteoinduction of porous titanium: a comparative study between acid–alkali and chemical–thermal treatments. J Biomed Mater Res B Appl Biomater. 2010;95B:387–96.
Takemoto M, Fujibayashi S, Neo M, Suzuki J, Matsushita T, Kokubo T, et al. Osteoinductive porous titanium implants: effect of sodium removal by dilute HCl treatment. Biomaterials. 2006;27:2682–91.
Yu S, Yu Z-t, Wang G, Han J-y, Ma X-q, Dargusch MS. Preparation and osteoinduction of active micro-arc oxidation films on Ti-3Zr-2Sn-3Mo-25Nb alloy. Trans Nonferrous Met Soc China. 2011;21:573–80.
Habibovic P, Sees TM, van den Doel MA, van Blitterswijk CA, de Groot K. Osteoinduction by biomaterials—Physicochemical and structural influences. J Biomed Mater Res Part A. 2006;77A:747–62.
Nakamura T. Biomaterial osteoinduction. J Orthop Sci. 2007;12:111–2.
Habibovic P, Yuan H, van der Valk CM, Meijer G, van Blitterswijk CA, de Groot K. 3D microenvironment as essential element for osteoinduction by biomaterials. Biomaterials. 2005;26:3565–75.
Habibovic P, de Groot K. Osteoinductive biomaterials—properties and relevance in bone repair. J Tissue Eng Regen Med. 2007;1:25–32.
Miron RJ, Zhang YF. Osteoinduction: a review of old concepts with new standards. J Dent Res. 2012;91:736–44.
Zhang XD, Yuan HP, De Groot K. Calcium phosphate biomaterials with intrinsic osteoinductivity. The 6th world biomaterials congress Hawaii, USA, May15–20, 2000.
Olivares-Navarrete R, Hyzy SL, Hutton DL, Erdman CP, Wieland M, Boyan BD, et al. Direct and indirect effects of microstructured titanium substrates on the induction of mesenchymal stem cell differentiation towards the osteoblast lineage. Biomaterials. 2010;31:2728–35.
Hu Y, Cai K, Luo Z, Zhang R, Yang L, Deng L, et al. Surface mediated in situ differentiation of mesenchymal stem cells on gene-functionalized titanium films fabricated by layer-by-layer technique. Biomaterials. 2009;30:3626–35.
Cai K, Lai M, Yang W, Hu R, Xin R, Liu Q, et al. Surface engineering of titanium with potassium hydroxide and its effects on the growth behavior of mesenchymal stem cells. Acta Biomater. 2010;6:2314–21.
Martin JY, Schwartz Z, Hummert TW, Schraub DM, Simpson J, Lankford J, et al. Effect of titanium surface roughness on proliferation, differentiation, and protein synthesis of human osteoblast-like cells (MG63). J Biomed Mater Res. 1995;29:389–401.
Zhu X, Chen J, Scheideler L, Reichl R, Geis-Gerstorfer J. Effects of topography and composition of titanium surface oxides on osteoblast responses. Biomaterials. 2004;25:4087–103.
Gomes ME, Holtorf HL, Reis RL, Mikos AG. Influence of the porosity of starch-based fiber mesh scaffolds on the proliferation and osteogenic differentiation of bone marrow stromal cells cultured in a flow perfusion bioreactor. Tissue Eng. 2006;12:801–9.
Holtorf HL, Datta N, Jansen JA, Mikos AG. Scaffold mesh size affects the osteoblastic differentiation of seeded marrow stromal cells cultured in a flow perfusion bioreactor. J Biomed Mater Res Part A. 2005;74A:171–80.
Takahashi Y, Tabata Y. Effect of the fiber diameter and porosity of non-woven PET fabrics on the osteogenic differentiation of mesenchymal stem cells. J Biomater Sci Polym Ed. 2004;15:41–57.
St-Pierre J-P, Gauthier M, Lefebvre L-P, Tabrizian M. Three-dimensional growth of differentiating MC3T3-E1 pre-osteoblasts on porous titanium scaffolds. Biomaterials. 2005;26:7319–28.
Tengvall P, Elwing H, Sjöqvist L, Lundström I, Bjursten LM. Interaction between hydrogen peroxide and titanium: a possible role in the biocompatibility of titanium. Biomaterials. 1989;10:118–20.
Tengvall P, Lundström I, Sjöqvist L, Elwing H, Bjursten LM. Titanium-hydrogen peroxide interaction: model studies of the influence of the inflammatory response on titanium implants. Biomaterials. 1989;10:166–75.
Zhao CY, Liang KL, Tan J, Xiang Z, Fan HS, Zhang XD. Bioactivity of porous titanium with hydrogen peroxide solution with or without tantalum chloride treatment at a low temperature. Biomed Mater. 2013;8(2):025006.
Kokubo T, Takadama H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials. 2006;27:2907–15.
Hennessy KM, Pollot BE, Clem WC, Phipps MC, Sawyer AA, Culpepper BK, et al. The effect of collagen I mimetic peptides on mesenchymal stem cell adhesion and differentiation, and on bone formation at hydroxyapatite surfaces. Biomaterials. 2009;30:1898–909.
Caplan AI. Why are MSCs therapeutic? New data: new insight. J Pathol. 2009;217:318–24.
Dee KC, Puleo DA, Bizios R. Protein-surface interactions. In: Dee KC, Puleo DA, Bizios R, editors. An introduction to tissue-biomaterial interactions. New York: Wiley; 2002. p. 37–52.
Puleo DA, Nanci A. Understanding and controlling the bone-implant interface. Biomaterials. 1999;20:2311–21.
Wassell DTH, Embery G. Adsorption of bovine serum albumin on to titanium powder. Biomaterials. 1996;17(9):859–64.
Wu J-M, Hayakawa S, Tsuru K, Osaka A. Low-temperature preparation of anatase and rutile layers on titanium substrates and their ability to induce in vitro apatite deposition. J Am Ceram Soc. 2004;87(9):1635–42.
Zeng H, Chittur KK, Lacefield WR. Analysis of bovine serum albumin adsorption on calcium phosphate and titanium surfaces. Biomaterials. 1999;20:377–84.
Kilpadi KL, Chang P-L, Bellis SL. Hydroxylapatite binds more serum proteins, purified integrins, and osteoblast precursor cells than titanium or steel. J Biomed Mater Res. 2001;57:258–67.
Sawyer AA, Hennessy KM, Bellis SL. Regulation of mesenchymal stem cell attachment and spreading on hydroxyapatite by RGD peptides and adsorbed serum proteins. Biomaterials. 2005;26:1467–75.
Yang YZ, Glover R, Ong JL. Fibronectin adsorption on titanium surfaces and its effect on osteoblast precursor cell attachment. Colloids Surf B Biointerfaces. 2003;30:291–7.
Cairns ML, Burke GA, Meenan BJ. Regulation of osteoblast attachment and morphology on calcium phosphate coatings by surface chemistry and pre-adsorption of fibronectin. Bone. 2005;36:S285–6.
Maegawa N, Kawamura K, Hirose M, Yajima H, Takakura Y, Ohgushi H. Enhancement of osteoblastic differentiation of mesenchymal stromal cells cultured by selective combination of bone morphogenetic protein-2 (BMP-2) and fibroblast growth factor-2 (FGF-2). J Tissue Eng Regen Med. 2007;1:306–13.
Jaiswal N, Haynesworth SE, Caplan AI, Bruder SP. Osteogenic differentiation of purified, culture-expanded human mesenchymal stem cells in vitro. J Cell Biochem. 1997;64:295–312.
Schwartz Z, Simon BJ, Duran MA, Barabino G, Chaudhri R, Boyan BD. Pulsed electromagnetic fields enhance BMP-2 dependent osteoblastic differentiation of human mesenchymal stem cells. J Orthop Res. 2008;26:1250–5.
Shimaoka H, Dohi Y, Ohgushi H, Ikeuchi M, Okamoto M, Kudo A, et al. Recombinant growth/differentiation factor-5 (GDF-5) stimulates osteogenic differentiation of marrow mesenchymal stem cells in porous hydroxyapatite ceramic. J Biomed Mater Res Part A. 2004;68A:168–76.
Na K, Kim Sw, Sun BK, Woo DG, Yang HN, Chung HM, et al. Osteogenic differentiation of rabbit mesenchymal stem cells in thermo-reversible hydrogel constructs containing hydroxyapatite and bone morphogenic protein-2 (BMP-2). Biomaterials. 2007;28:2631–7.
Lissenberg-Thunnissen S, Gorter DJ, Sier CM, Schipper I. Use and efficacy of bone morphogenetic proteins in fracture healing. Int Orthop (SICOT). 2011;35:1271–80.
Gautschi OP, Frey SP, Zellweger R. Bone morphogenetic proteins in clinical applications. ANZ J Surg. 2007;77:626–31.
Sykaras N, Opperman LA. Bone morphogenetic proteins (BMPs): how do they function and what can they offer the clinician? J Oral Sci. 2003;45:57–74.
Frank O, Heim M, Jakob M, Barbero A, Schäfer D, Bendik I, et al. Real-time quantitative RT-PCR analysis of human bone marrow stromal cells during osteogenic differentiation in vitro. J Cell Biochem. 2002;85:737–46.
Sumanasinghe RD, Bernacki SH, Loboa EG. Osteogenic differentiation of human mesenchymal stem cells in collagen matrices: effect of uniaxial cyclic tensile strain on bone morphogenetic protein (BMP-2) mRNA expression. Tissue Eng. 2006;12:3459–65.
Phimphilai M, Zhao Z, Boules H, Roca H, Franceschi RT. BMP signaling is required for RUNX2-dependent induction of the osteoblast phenotype. J Bone Miner Res. 2006;21:637–46.
Jonášová L, Müller FA, Helebrant A, Strnad J, Greil P. Biomimetic apatite formation on chemically treated titanium. Biomaterials. 2004;25:1187–94.
Kim HM, Miyaji F, Kokubo T, Nakamura T. Effect of heat treatment on apatite-forming ability of Ti metal induced by alkali treatment. J Mater Sci: Mater Med. 1997;8:341–7.
Liang F, Zhou L, Wang K. Apatite formation on porous titanium by alkali and heat-treatment. Surf Coat Technol. 2003;165:133–9.
Vanzillotta PS, Sader MS, Bastos IN, Soares GdA. Improvement of in vitro titanium bioactivity by three different surface treatments. Dent Mater. 2006;22:275–82.
Ohtsuki C, Iida H, Hayakawa S, Osaka A. Bioactivity of titanium treated with hydrogen peroxide solutions containing metal chlorides. J Biomed Mater Res. 1997;35:39–47.
Acknowledgments
This work was financially supported by National Natural Science Foundation of China (Contract Grant No. 81190131) and National Key Technology Support Program of China (Contract Grant No. 2012BAI18B04 and 2012BAI17B01).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yang, J., Wang, J., Yuan, T. et al. The enhanced effect of surface microstructured porous titanium on adhesion and osteoblastic differentiation of mesenchymal stem cells. J Mater Sci: Mater Med 24, 2235–2246 (2013). https://doi.org/10.1007/s10856-013-4976-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-4976-4