Abstract
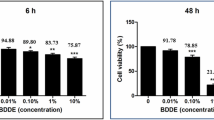
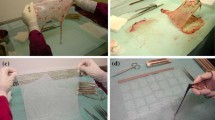
The disadvantages of human amniotic membrane (hAM), used for ocular surface reconstruction, necessitate the development of standardized alternatives. Keratin-derived-films (KF) have been indicated as transferable substrate for cell cultivation and tissue engineering. The impact of different sterilization procedures on KF and surgical feasibility were investigated. Human hair KF were prepared and sterilized; optical, biomechanical properties, in vitro cell seeding efficiency and proliferation of human corneal epithelial cells were studied and compared with hAM. Surgical feasibility was tested on enucleated porcine eye. Sterilized KF showed higher light transmission and significantly higher E-modulus than hAM; cell-seeding-efficiency and proliferation rate were not affected. Although KF could be surgically handled, suture placement was more difficult compared to hAM. Plasma treatment seems the best sterilization method for KF; it does not affect cell biology or optical and biomechanical properties. However material modifications are requested before KF may represent a feasible alternative for ocular surface reconstruction.







Similar content being viewed by others
References
Dua HS, Gomes JA, King AJ, Maharajan VS. The amniotic membrane in ophthalmology. Surv Ophthalmol. 2004;49:51–77.
Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997;123:303–12.
Chen HJ, Pires RT, Tseng SC. Amniotic membrane transplantation for severe neurotrophic corneal ulcers. Br J Ophthalmol. 2000;84:826–33.
Hanada K, Shimazaki J, Shimmura S, Tsubota K. Multilayered amniotic membrane transplantation for severe ulceration of the cornea and sclera. Am J Ophthalmol. 2001;131:324–31.
Rodríguez-Ares MT, Touriño R, López-Valladares MJ, Gude F. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004;23:577–83.
Tsubota K, Satake Y, Ohyama M, et al. Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens–Johnson syndrome. Am J Ophthalmol. 1996;122:38–52.
Tseng SC, Prabhasawat P, Lee SH. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol. 1997;124:765–74.
Nakamura T, Inatomi T, Sekiyama E, Ang LPK, Yokoi N, Kinoshita S. Novel clinical application of sterilized, freeze-dried amniotic membrane to treat patients with pterygium. Acta Ophthalmol Scand. 2006;84:401–5.
Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Eng J Med. 2000;343:86–93.
Rama P, Bonini S, Lambiase A, et al. Autologous fibrin-cultured limbal stem cells permanently restore the corneal surface of patients with total limbal stem cell deficiency. Transplantation. 2001;72:1478–85.
Shimazaki J, Aiba M, Goto E, Kato N, Shimmura S, Tsubota K. Transplantation of human limbal epithelium cultivate on amniotic membrane for the treatment of severe ocular surface disorders. Ophthalmology. 2002;109:1285–90.
Eberle J, Habermann J, Gürtler LG. HIV-1 infection transmitted by serum droplets into the eye: a case report. AIDS. 2000;14(2):206–7.
Gündüz K, Uçakhan OO, Kanpolat A, Günalp I. Nonpreserved human amniotic membrane transplantation for conjunctival reconstruction after excision of extensive ocular surface neoplasia. Eye. 2006;20:351–7.
Gicquel JJ, Dua HS, Brodie A, et al. Epidermal growth factor variations in amniotic membrane used for ex vivo tissue constructs. Tissue Eng Part A. 2009;15:1919–27.
Rahman I, Said DG, Maharajan VS, Dua HS. Amniotic membrane in ophthalmology: indications and limitations. Eye. 2009;23:1954–61.
Kruse FE, Joussen AM, Rohrschneider K, et al. Cryopreserved human amniotic membrane for ocular surface reconstruction. Graefe’s Arch Clin Exp Ophthalmol. 2000;238:68–75.
Rama P, Giannini R, Bruni A, Gatto C, Tiso R, Ponzin D. Further evaluation of amniotic membrane banking for transplantation in ocular surface diseases. Cell Tissue Bank. 2001;2:155–63.
Rodríguez-Ares MT, López-Valladares MJ, Touriño R, et al. Effects of lyophilization on human amniotic membrane. Acta Ophthalmol. 2009;87:396–403.
Dua HS, Rahman I, Miri A, Said DG. Variations in amniotic membrane: relevance for clinical applications. Br J Ophthalmol. 2010;94:963–4.
Hopkinson A, McIntosh RS, Tighe PJ, James DK, Dua HS. Amniotic membrane for ocular surface reconstruction: donor variations and the effect of handling on TGF-beta contents. Investig Ophthalmol Vis Sci. 2006;47:4316–22.
Bourne GL. The microscopic anatomy of the human amnion and chorion. Am J Obstet Gynecol. 1960;79:1070–3.
Koizumi N, Inatomi T, Sotozono C, Fullwood NJ, Quantock AJ, Kinoshita S. Growth factor mRNA and protein in preserved human amniotic membrane. Curr Eye Res. 2000;20:173–7.
López-Valladares MJ, Rodríguez-Ares MT, Touriño R, Gude F, Silva MT, Couceiro J. Donor age and gestational age influence on growth factor levels in human amniotic membrane. Acta Ophthalmol. 2010;88:211–6.
Hill P, Brantley H, Van Dyke M. Some properties of keratin biomaterials: kerateines. Biomaterials. 2010;31:585–93.
Schrooyen PM, Dijkstra PJ, Oberthür RC, Bantjes A, Feijen J. Partially carboxymethylated feather keratins. 2. Thermal and mechanical properties of films. J Agric Food Chem. 2001;49:221–30.
Verma P, Ray P, Ray AR. Preparation of scaffolds from human hair proteins for tissue-engineering applications. Biomed Mater. 2008;3:25007.
Tachibana A, Kaneko S, Tanabe T, Yamauchi K. Rapid fabrication of keratin-hydroxyapatite hybrid sponges toward osteoblast cultivation and differentiation. Biomaterials. 2005;26:297–302.
Sierpinski P, Garrett J, Ma J, et al. The use of keratin biomaterials derived from human hair for the promotion of rapid regeneration of peripheral nerves. Biomaterials. 2008;29:118–28.
Chen Y, Dong WR, Xiao YQ, Zhao BL, Hu GD, An LB. Preparation and bioactivity of human hair keratin-collagen sponge, a new type of dermal analogue. Nan Fang Yi Ke Da Xue Xue Bao. 2006;26:131–8.
Dias G, Peplow P, McLaughlin A, Teixeira F, Kelly R. Biocompatibility and osseointegration of reconstituted keratin in an ovine model. J Biomed Mater Res Part A. 2010;92:513–20.
de Guzman RC, Merrill MR, Richter JR, Hamzi RI, Greengauz-Roberts OK, Van Dyke ME. Mechanical and biological properties of keratose biomaterials. Biomaterials. 2011;32:8205–17.
Reichl S, Borrelli M, Geerling G. Keratin films for ocular surface reconstruction. Biomaterials. 2011;32:3375–86.
Riau AK, Beuerman RW, Lim LS, Mehta JS. Preservation, sterilization and de-epithelialization of human amniotic membrane for use in ocular surface reconstruction. Biomaterials. 2010;31:216–25.
Thomasen H, Pauklin M, Noelle B, Geerling G, Vetter J, Steven P, Steuhl KP, Meller D. The effect of long-term storage on the biological and histological properties of cryopreserved amniotic membrane. Curr Eye Res. 2011;36:247–55.
Nakamura A, Arimoto M, Takeuchi K, Fujii T. A rapid extraction procedure of human hair proteins and identification of phosphorylated species. Biol Pharm Bull. 2002;25:569–72.
Araki-Sasaki K, Ohashi Y, Sasabe T, et al. An SV40-immortalized human corneal epithelial cell line and its characterization. Invest Ophthalmol Vis Sci. 1995;36:614–21.
Yamauchi K, Maniwa M, Mori T. Cultivation of fibroblast cells on keratin-coated substrata. J Biomater Sci Polym Ed. 1998;9:259–70.
Tachibana A, Furuta Y, Takeshima H, Tanabe T, Yamauchi K. Fabrication of wool keratin sponge scaffolds for long-term cell cultivation. J Biotechnol. 2002;93:165–70.
Reichl S. Films based on human hair keratin as substrates for cell culture and tissue engineering. Biomaterials. 2009;30:6854–66.
Yamauchi K, Hojo H, Yamamoto Y, Tanabe T. Enhanced cell adhesion on RGDS-carrying keratin film. Mater Sci Eng C. 2003;23:467–72.
Srinivasan B, Kumar R, Shanmugam K, Sivagnam U, Reddy N, Sehgal P. Porous keratin scaffold-promising biomaterial for tissue engineering and drug delivery. J Biomed Mater Res Part B Appl Biomater. 2010;92:5–12.
Rouse JG, Van Dyke ME. A review of keratin-based biomaterials for biomedical applications. Materials. 2010;3:999–1014.
Connon CJ, Doutch J, Chen B, et al. The variation in transparency of amniotic membrane used in ocular surface regeneration. Br J Ophthalmol. 2010;94:1057–61.
Mandal B, Kundu S. Non-bioengineered silk gland fibroin protein: characterization and evaluation of matrices for potential tissue engineering applications. Biotechnol Bioeng. 2008;100:1237–50.
Rafat M, Griffith M, Hakim M, et al. Plasma surface modification and characterization of collagen-based artificial cornea for enhanced epithelialization. J Appl Polym Sci. 2007;106:2056–64.
Acknowledgments
The authors would like to thank Dr. K. Araki-Sasaki (Kagoshima, Japan) for his generous gift of the HCE-T cell line, and Dr. Meyer (Department of Ophthalmology, University of Würzburg, Germany) for help with the statistical analysis. Furthermore, special thanks are given to Drs. T. Klink, R. Guthoff and H. Sold (Department of Ophthalmology, University of Würzburg, Germany) for their time spent in the laboratory participating in the surgical feasibility tests, as well as Lucia Albrecht and Gesa Grobe (Technische Universität Braunschweig, Germany) for their technical assistance in the cell culture studies and tensile strength testing. This work was supported by the Deutsche Forschungsgemeinschaft, DFG grants Re 2596/3-1 and Ge 895/7-1.
Author information
Authors and Affiliations
Corresponding author
Additional information
Maria Borrelli and Stephan Reichl contributed equally to this study.
Rights and permissions
About this article
Cite this article
Borrelli, M., Reichl, S., Feng, Y. et al. In vitro characterization and ex vivo surgical evaluation of human hair keratin films in ocular surface reconstruction after sterilization processing. J Mater Sci: Mater Med 24, 221–230 (2013). https://doi.org/10.1007/s10856-012-4774-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4774-4