Abstract
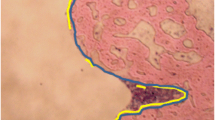
The aim of this study was to assess tissue reactions to bioabsorbable self-reinforced ciprofloxacin-releasing polylactide/polyglycolide (SR-PLGA) 80/20 screws in rabbits’ cranial bone. Two screws were implanted in each rabbit, one screw on either side of the sagittal suture (n = 28 rabbits). Animals were sacrificed after 2, 4, 8, 16, 24, 54 and 72 weeks, four animals per group. On histological examination the number of macrophages, giant cells, active osteoblasts and fibrous tissue layers were assessed and degradation of the screws was evaluated. At 2 weeks, the highest number of macrophages and giant cells were seen near the heads of the screws. After 4 and 8 weeks, the number of giant cells decreased but that of macrophages decreased from 16 weeks and on. Screws were surrounded by fibrous tissue capsule that progressively was growing in thickness by time. Active osteoblasts were seen around the shaft of the screws with the highest number seen at 4 weeks postoperatively. At 16 weeks, compact fragmentation of the screw heads was seen with macrophages seen inside the screw matrices. After 24 weeks, no polarization of the screws was seen. After one year, PLGA screws had been replaced by adipose tissue, fibrous tissue and “foamy macrophages” which had PLGA particles inside them. After 1½ years, the amount of biomaterial remaining had decreased remarkably. The particles of biomaterial were inside “foamy macrophages.” Ciprofloxacin-releasing SR-PLGA 80/20 screws elicited a mild inflammatory reaction but did not interfere with osteoblast activity. No complications were seen when implanted in cranial bone of rabbit.
Similar content being viewed by others
References
L. NIE, D. NICOLAU, P. TESSIER, H. KOUREA, B. BROWNER and C. NIGHTINGALE, Use of a bioabsorbable polymer for the delivery of ofloxacin during experimental osteomyelitis treatment. J. Orthop. Res. 16 (1998) 76–79.
P. BECKER, R. SMITH, R. WILLIAMS and J. DUTKOWSKY, Comparison of antibiotic release from polymethylmethacrylate beads and sponge collagen. J. Orthop. Res. 12 (1994) 737–741.
J. CALHOUN and J. MADER, Treatment of osteomyelitis with a biodegradable antibiotic implant. Clin. Orthop. 341 (1997) 206–214.
Y. SHINTO, A. UCHIDA, F. KORKUSUZ, N. ARAKI and K. ONO, Calcium hydroxyapatite ceramic used as a delivery system for antibiotics. J. Bone. Joint. Surg. Br. 74-B (1992) 600–604.
J. OVERBECK, S. WINCKLER, R. MEFFERT, P. TÖRMÄLÄ, H. SPIEGEL and E. BRUG, Penetration of ciprofloxacin into bone: A new bioabsorbable implant. J. Invest. Surg. 8 (1995) 155–162.
E. JACOB, J. SETTERSTRÖM, D. BACH, J. R. HEATH, L. MCNIESH and G. CIERNY, Evaluation of biodegradable ampicillin anhydrate microcapsules for local treatment of experimental staphylococcal osteomyelitis. Clin. Orthop. 267 (1991) 237–244.
P. OSTERMANN, S. HENRY and D. SELIGSON, The role of local antibiotic therapy in the management of compound fractures. Clin. Orthop. 295 (1993) 102–111.
M. GÜMÜ SDERELIOGLU and G. DENIZ, Sustained release of mitomycin-C from poly (DL-lactide) /poly (DL-lactide-co-glycolide) films. J. Biomater. Sci. 11 (2000) 1039–1050.
C. TEUPE, R. MEFFERT, S. WINCKLER, W. RITZERFELD, P. TÖRMÄLÄ and E. BRUG, Ciprofloxacin-impregnated poly-L-lactic acid drug carrier. New aspects of a resorbable drug delivery system in local antimicrobial treatment of bone infections. Arch. Orthop. Trauma Surg. 112 (1992) 33–35.
J. TIAINEN, M. VEIRANTO, E. SUOKAS, P. TÖRMÄLÄ and T. WARIS, M. Ninkovic and N. Ashammakhi, Bioabsorbable ciprofloxacin-containing and plain self-reinforced polylactide-polyglycolide 80/20 screws: pull-out strength properties in human cadaver parietal bones. J. Craniofac. Surg. 13 (2002) 427–433.
S. LEINONEN, E. SUOKAS, M. VEIRANTO, P. TÖRMÄLÄ, T. WARIS and N. ASHAMMAKHI, Holding power of bioabsorbable ciprofloxacin-containing self-reinforced poly-L/DL-lactide 70/30 bioactive glass 13 miniscrews in human cadaver bone. J. Craniofac. Surg. 13 (2002) 212–218.
N. ASHAMMAKHI, Neomembranes: A concept review with special reference to self-reinforced polyglycolide membranes. J. Biomed. Mater. Res. [Appl. Biomater.] 33 (1996) 297–303.
B. EPPLEY and M. SADOVE, A comparison of resorbable and metallic fixation in healing of calvarial bone grafts. Plast. Reconstr. Surg. 96 (1995) 316–322.
M. VEIRANTO, E. SUOKAS, N. ASHAMMAKHI and P. TÖRMÄLÄ, Novel bioabsorbable antibiotic releasing bone fracture fixation implants. Adv. Exp. Med. Biol. 553 (2004) 197–208.
S.-M. NIEMELÄ, I. IKÄ HEIMO, M. KOSKELA, M. VEIRANTO, E. SUOKAS, P. TÖRMÄLÄ, T. WARIS, N. ASHAMMAKHI and H. SYRJÄ LÄ, Ciprofloxacin-releasing bioabsorbable polymer is superior to titanium in preventing Staphylococcus epidermis attachment and biofilm formation in vitro. J. Biomed. Mater. Res. [Appl. Biomater.] (Accepted) .
J. KITCHELL and D. WISE, Poly(lactic/glycolic acid) biodegradable drug-polymer matrix systems. Methods Enzymol. 112 (1985) 436–448.
S. HUMPHREY, S. MEHTA, A. SEABER and T. VAIL, Pharmacokinetics of a degradable drug delivery system in bone. Clin. Orthop. 349 (1998) 218–224.
M. VERT, M. LI, G. SPENLEHAUER and P. GUERIN, Bioresorbability and biocompatibility of aliphatic polyesters. J. Mater. Sci. Mater. Med. 3 (1992) 432–446.
P. TÖRMÄLÄ, Biodegradable self-reinforced composite materials; manufacturing structure and mechanical properties. Clin. Mater. 10 (1992) 29–34.
W. PIETRZAK, D. SARVER and M VERSTYNEN, Bioabsorbable polymer science for the practicing surgeon. J. Craniofac. Surg. 8 (1997) 87–91.
K. KNUUTILA, J. TIAINEN, M. VEIRANTO, E. SUOKAS, T. WARIS, P. TÖRMÄLÄ, O. KAARELA and N. ASHAMMAKHI, Pull-Out Strength Properties of Antibiotic Releasing Tacks in Human Cadaver Bone. Society for Biomaterials Symposium on Biomaterials in Regenerative Medicine: The Advent of Combination Products, Philadelphia, Pennsylvania, USA, 10 (2004) 16–18.
P. D. HOLTOM, S. A. PAVKOVIC, P. D. BRAVOS, M. J. PATZAKIS, L. E. SHEPHERD and B. FRENKEL, Inhibitory effects of the quinolone antibiotics trovafloxacin, ciprofloxacin, and levofloxacin on osteoblastic cells in vitro. J. Orthop. Res. 18 (2000) 721–727.
T. MICLAU, M. L. EDIN, G. E. LESTER, R. W. LINDSEY and L. E. DAHNERS, Effect of ciprofloxacin on the proliferation of osteoblast-like MG-63 human osteosarcoma cells in vitro. J. Orthop. Res. 16 (1998) 509–512.
A. C. PERRY, B. PRPA, M. S. ROUSE, K. E. PIPER, A. D. HANSSEN, J. M. STECKELBERG and R. PATEL, Levofloxacin and trovafloxacin inhibition of experimental fracture-healing. Clin. Orthop. 414 (2003) 95–100.
N. ASHAMMAKHI, H. PELTONIEMI, E. WARIS, R. SUURONEN, W. SERLO, M. KELLOMäKI, P. TÖRMÄLÄ and T. WARIS, Developments in craniomaxillofacial surgery: Use of self-reinforced polyglycolide and polylactide osteofixation devices. Review. Plast. Reconstr. Surg. 108 (2001) 167–180.
J. HUNT and D. WILLIAMS, Quantifying the soft tissue response to implanted materials. Biomaterials. 16 (1995) 167–170.
J. TIAINEN, Y. SOINI, P. TÖRMÄLÄ, T. WARIS and N. ASHAMMAKHI, Self-reinforced polylactide-polyglycolide 80/20 screws take more than 1 1/2 years to resorb in rabbit cranial bone. J. Biomed. Mater. Res. [Appl. Biomater.] 70B (2004) 49–55.
M. HABAL and W. PIETRZAK, Key points in the fixation of the craniofacial skeleton with absorbable biomaterial. J. Craniofac. Surg. 10 (1999) 491–499.
N. ASHAMMAKHI, Editorial. Reactions to Biomaterials: the Good, the Bad and Ideas for Developing New Therapeutic Approaches. J. Craniofac. Surg. 16 (2005) 195.
G. VINCE, J. HUNT and D. WILLIAMS, Quantitative assessment of the tissue response to implanted biomaterials. Biomaterials. 12 (1991) 731–736.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sources of support: Technology Development Center in Finland (TEKES, 90220), the European Commission (Biomedicine and Health Programme, European Union Demonstration Project BMH4-98-3892 and R&D Project QLRT-2000-00487), the Academy of Finland (Group of Excellence, Project 37726), and the Ministry of Education (Graduate School of Biomaterials and Tissue Engineering).
Rights and permissions
About this article
Cite this article
Tiainen, J., Soini, Y., Suokas, E. et al. Tissue reactions to bioabsorbable ciprofloxacin-releasing polylactide-polyglycolide 80/20 screws in rabbits’ cranial bone. J Mater Sci: Mater Med 17, 1315–1322 (2006). https://doi.org/10.1007/s10856-006-0606-8
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10856-006-0606-8