Abstract
Purpose
Pericardial effusion (PE) may occur during the lead extraction procedure (TLE). Little is known about the incidence, causes, and predictors of this complication.
Methods
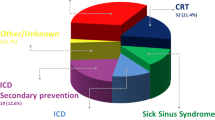
From January 2009 to October 2016, TLE was attempted for 297 leads in 212 patients (age 69.3 ± 12.9 years, 169 male, BMI 27.2 ± 9.9 m²/kg, LVEF 43.4 ± 24.6%) for lead dysfunction (62.7%), upgrade (16.0%), infection (14.2%), or other (7.0%) indications. TLE was performed under general anesthesia with continuous invasive arterial blood pressure and transesophageal echocardiography (TEE) monitoring. For lead removal, the mechanical approach was first attempted, followed by the laser-assisted technique when needed. Severity of PE was defined by the presence of hemodynamically significant PE > 10 mm at TEE.
Results
Clinical success was achieved for 292 leads (98.3%). New-onset PE was observed in 14 patients (6.6%) [mild entity in 7 patients (3.3%) and severe in 7 (3.3%)]. In these latter patients, intra-procedural management included surgery (n = 3), pericardiocentesis (n = 2), or a conservative approach (n = 2). Right ventricular (RV) site lesions were treated with a simple fluid infusion. Laceration of the superior vena cava and other vessels resulted in rescue surgery. Lesions of the right atrial free wall (n = 1) and coronary sinus (n = 1) were treated with pericardiocentesis. NYHA III/IV, LVEF < 35%, renal impairment, right-sided implant, and ≥2 leads targeted for TLE were associated with new-onset PE. More than two factors identified a higher risk group (16.2%, 95% CI 6.2–32.0%, P = 0.02).
Conclusions
New-onset PE is common during TLE and is associated with specific factors. PE severity and subsequent patient management depend on the site of injury.




Similar content being viewed by others
References
Arribas F, Auricchio A, Boriani G, Brugada J, Deharo JC, Hindriks G, et al. Statistics on the use of cardiac electronic devices and electrophysiological procedures in 55 ESC countries: 2013 report from the European heart rhythm association (EHRA). Europace. 2014;16(Suppl 1):i1–i78.
Bongiorni MG, Blomström-Lundqvist C, Kennergren C, Dagres N, Pison L, Svendsen JH, et al. Scientific initiative committee, European heart rhythm association. Current practice in transvenous lead extraction: a European heart rhythm association EP network survey. Europace. 2012;14:783–6.
Bongiorni MG, Kennergren C, Butter C, Deharo JC, Kutarski A, Rinaldi CA, et al. The European lead extraction ConTRolled (ELECTRa) study: a European heart rhythm association (EHRA) registry of Transvenous lead extraction outcomes. Eur Heart J. 2017;38:2995–3005.
Deharo JC, Bongiorni MG, Rozkovec A, Bracke F, Defaye P, Fernandez-Lozano I, et al. Pathways for training and accreditation for transvenous lead extraction: a European heart rhythm association position paper. Europace. 2012;14:124–34.
Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, et al. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management. Heart Rhythm. 2009;6:1085–104.
Kusumoto FM, Schoenfeld MH, Wilkoff BL, Berul CI, Birgersdotter-Green UM, Carrillo R, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–51.
Regoli F, Caputo M, Conte G, Faletra FF, Moccetti T, Pasotti E, et al. Clinical utility of routine use of continuous transesophageal echocardiography monitoring during transvenous lead extraction procedure. Heart Rhythm. 2015;12:313–20.
Swanton BJ, Keane D, Vlahakes GJ, Streckenbach SC. Intraoperative transesophageal echocardiography in the early detection of acute tamponade after laser extraction of a defibrillator lead. Anesth Analg. 2003;97(3):654–6.
Wazni O, Epstein LM, Carrillo RG, Love C, Adler SW, Riggio DW, et al. Lead extraction in the contemporary setting: the LExICon study. J Am Coll Cardiol. 2010;55:579–86.
Love CJ, Wilkoff BL, Byrd CL, et al. Recommendations for extraction of chronically implanted transvenous pacing and defibrillator leads: indications, facilities, training. North American Society of Pacing and Electrophysiology Lead Extraction Conference Faculty. Pacing Clin Electrophysiol. 2000;23:544–51.
Bongiorni MG, Di Cori A, Segreti L, Zucchelli G, Viani S, Paperini L, et al. Transvenous extraction profile of riata leads: procedural outcomes and technical complexity of mechanical removal. Heart Rhythm. 2015;12:580–7.
Sk A, Kamireddy S, Nemec J, Voigt A, Saba S. Predictors of complications of endovascular chronic lead extractions from pacemakers and defibrillators: a single-operator experience. J Cardiovasc Electrophysiol. 2009;20(2):171–5.
Glover BM, Watkins S, Mariani JA¸ Yap S, Asta J, Cusimano RJ, Ralph-Edwards AC et al. Prevalence of tricuspid regurgitation and pericardial effusions following pacemaker and defibrillator lead extraction. Int J Cardiol 2010;145:593–594.
Hauser RG, Katsiyiannis WT, Gornick CC, Almquist AK, Kallinen LM. Deaths and cardiovascular injuries due to device-assisted implantable cardioverter-defibrillator and pacemaker lead extraction. Europace. 2010;12:395–401.
Brunner MP, Cronin EM, Duarte VE, Baranowski B, Saliba WI, Sabik JF, et al. Clinical predictors of adverse patient outcomes in an experience of more than 5000 chronic endovascular pacemaker and defibrillator lead extractions. Heart Rhythm. 2014;11:799–805.
Goyal SK, Ellis CR, Ball SK, Ahmad R, Hoff SJ, Whalen SP, et al. High-risk lead removal by planned sequential transvenous laser extraction and minimally invasive right thoracotomy. J Cardiovasc Electrophysiol. 2014;25:617–21.
Bontempi L, Vassanelli F, Cerini M, Bisleri G, Repossini A, Giroletti L, et al. Hybrid minimally invasive approach for Transvenous lead extraction: a feasible technique in high-risk patients. J Cardiovasc Electrophysiol. 2017;31:1202.
Bongiorni MG, Romano SL, Kennergren C, Butter C, Deharo JC, Kutarsky A, et al. ELECTRa (European lead extraction ConTRolled) registry—shedding light on transvenous lead extraction real-world practice in Europe. Herzschrittmacherther Elektrophysiol. 2013;24:171–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. F. Regoli receives speaker fees from Abbott (former St. Jude Medical), Boston Scientific, Bayer; Dr. A. Auricchio is a consultant for Medtronic, LivaNova, and Boston Scientific.
Rights and permissions
About this article
Cite this article
Regoli, F., D’Ambrosio, G., Caputo, M.L. et al. New-onset pericardial effusion during transvenous lead extraction: incidence, causative mechanisms, and associated factors. J Interv Card Electrophysiol 51, 253–261 (2018). https://doi.org/10.1007/s10840-018-0327-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-018-0327-1