Abstract
Background
Three-dimensional electroanatomic mapping (EAM) systems reduce radiation exposure when radio frequency catheter ablation (RFCA) procedures are performed by well-trained senior operators. Given the steep learning curve associated with complex RFCA, trainees and their mentors must rely on multiple imaging modalities to maximize safety and success, which might increase procedure and fluoroscopy times. The objective of the present study is to determine if 3-D EAM (CARTO and ESI-NavX) improves procedural outcomes (fluoroscopy time, radio frequency time, procedure duration, complication, and success rates) during CA procedures as compared to fluoroscopically guided conventional mapping alone in an academic teaching hospital.
Methods
We analyzed a total of 1070 consecutive RFCA procedures over an 8-year period for fluoroscopic time stratified by ablation target and mapping system. Multivariate logistic regression and adjusted odds ratios were calculated for each variable.
Results
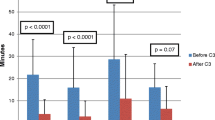
No statistically significant differences in acute success rates were noted between conventional and 3-D mapping cases [CARTO (p = 0.68) or ESI-NavX (p = 0.20)]. Moreover, complication rates were also not significantly different between CARTO (p = 0.23) and ESI-NavX (p = 0.53) when compared to conventional mapping. Procedure, radio frequency, and fluoroscopy times were significantly longer with CARTO and ESI-NavX versus conventional mapping [fluoroscopy time: CARTO, 28.3 min; ESI, 28.5 min; and conventional, 24.3 min; p < 0.001)].
Conclusions
The use of 3-D EAM systems during teaching cases significantly increases radiation exposure when compared with conventional mapping. These findings suggest a need to develop alternative training strategies that enhance confidence and safety during catheter manipulation and allow for reduced fluoroscopy and procedure times during RFCA.




Similar content being viewed by others
Abbreviations
- AF:
-
Atrial fibrillation
- AFL:
-
Atrial flutter
- ANOVA:
-
Analysis of variance
- AOR:
-
Adjusted odds ratios
- AVNRT:
-
Atrial tachycardia atrioventricular nodal reentry tachycardia
- AT:
-
Atrial tachycardia
- RFCA:
-
Radio frequency catheter ablation
- IR:
-
Ionized radiation
- WPW:
-
Wolff-Parkinson-White syndrome
- VT:
-
Ventricular tachycardia
References
Packer, D. L. (2005). Three-dimensional mapping in interventional electrophysiology: techniques and technology. Journal of Cardiovascular Electrophysiology, 16(10), 1110–1116.
Bhakta, D., & Miller, J. M. (2008). Principles of electroanatomic mapping. Indian Pacing and Electrophysiology Journal, 8(1), 32–50.
Wittkampf, F. H., Wever, E. F., Derksen, R., Wilde, A. A., Ramanna, H., Hauer, R. N., et al. (1999). LocaLisa: new technique for real-time 3-dimensional localization of regular intracardiac electrodes. Circulation, 99(10), 1312–1317.
Sporton, S. C., Earley, M. J., Nathan, A. W., & Schilling, R. J. (2004). Electroanatomic versus fluoroscopic mapping for catheter ablation procedures: a prospective randomized study. Journal of Cardiovascular Electrophysiology, 15(3), 310–315.
Della Bella, P., Fassini, G., Cireddu, M., Riva, S., Carbucicchio, C., Giraldi, F., et al. (2009). Image integration-guided catheter ablation of atrial fibrillation: a prospective randomized study. Journal of Cardiovascular Electrophysiology, 20(3), 258–265.
Casella, M., Pelargonio, G., Dello Russo, A., Riva, S., Bartoletti, S., Santangeli, P., et al. (2011). “Near-zero” fluoroscopic exposure in supraventricular arrhythmia ablation using the EnSite NavX mapping system: personal experience and review of the literature. Journal of Interventional Cardiac Electrophysiology, 31(2), 109–118.
Earley, M. J., Showkathali, R., Alzetani, M., Kistler, P. M., Gupta, D., Abrams, D. J., et al. (2006). Radiofrequency ablation of arrhythmias guided by non-fluoroscopic catheter location: a prospective randomized trial. European Heart Journal, 27(10), 1223–1229.
Shurrab, M., Laish-Farkash, A., Lashevsky, I., Morriello, F., Singh, S. M., Schilling, R. J., et al. (2013). Three-dimensional localization versus fluoroscopically only guided ablations: a meta-analysis. Scandinavian Cardiovascular Journal, 47(4), 200–209.
Morady, F. (1999). Radio-frequency ablation as treatment for cardiac arrhythmias. New England Journal of Medicine, 340(7), 534–544.
Scheinman, M. M. (1995). NASPE survey on catheter ablation. Pacing and Clinical Electrophysiology, 18(8), 1474–1478.
Katritsis, D., Efstathopoulos, E., Betsou, S., Korovesis, S., Faulkner, K., Panayiotakis, G., et al. (2000). Radiation exposure of patients and coronary arteries in the stent era: a prospective study. Catheterization and Cardiovascular Interventions, 51(3), 259–264.
Rehani, M. M. (2007). Training of interventional cardiologists in radiation protection—the IAEA’s initiatives. International Journal of Cardiology, 114(2), 256–260.
Bernardi, G., Padovani, R., Trianni, A., Morocutti, G., Spedicato, L., Zanuttini, D., et al. (2008). The effect of fellows’ training in invasive cardiology on radiological exposure of patients. Radiation Protection Dosimetry, 128(1), 72–76.
Eckardt, L., & Breithardt, G. (2009). Catheter ablation of ventricular tachycardia. From indication to three-dimensional mapping technology. Herz, 34(3), 187–196.
Coggins, D. L., Lee, R. J., Sweeney, J., Chein, W. W., Van Hare, G., Epstein, L., et al. (1994). Radiofrequency catheter ablation as a cure for idiopathic tachycardia of both left and right ventricular origin. Journal of the American College of Cardiology, 23(6), 1333–1341.
Waldo, A. L., Henthorn, R. W., Plumb, V. J., & MacLean, W. A. (1984). Demonstration of the mechanism of transient entrainment and interruption of ventricular tachycardia with rapid atrial pacing. Journal of the American College of Cardiology, 3(2 Pt 1), 422–430.
Gepstein, L., Hayam, G., & Ben-Haim, S. A. (1997). A novel method for nonfluoroscopic catheter-based electroanatomical mapping of the heart. In vitro and in vivo accuracy results. Circulation, 95(6), 1611–1622.
Razminia, M., Manankil, M. F., Eryazici, P. L., Arrieta-Garcia, C., Wang, T., D’Silva, O. J., et al. (2012). Nonfluoroscopic catheter ablation of cardiac arrhythmias in adults: feasibility, safety, and efficacy. Journal of Cardiovascular Electrophysiology, 23(10), 1078–1086.
Gellis, L. A., Ceresnak, S. R., Gates, G. J., Nappo, L., & Pass, R. H. (2013). Reducing patient radiation dosage during pediatric SVT ablations using an “ALARA” radiation reduction protocol in the modern fluoroscopic era. Pacing and Clinical Electrophysiology, 36(6), 688–694.
Bulava, A., Hanis, J., & Eisenberger, M. (2015). Catheter ablation of atrial fibrillation using zero-fluoroscopy technique: a randomized trial. Pacing and Clinical Electrophysiology, 38(7), 797–806.
Stellbrink, C., Siebels, J., Hebe, J., Koschyk, D., Haltern, G., Ziegert, K., et al. (1994). Potential of intracardiac ultrasonography as an adjunct for mapping and ablation. American Heart Journal, 127(4 Pt 2), 1095–1101.
Ullah, W., Hunter, R. J., Baker, V., Dhinoja, M. B., Sporton, S., Earley, M. J., et al. (2014). Target indices for clinical ablation in atrial fibrillation: insights from contact force, electrogram, and biophysical parameter analysis. Circulation. Arrhythmia and Electrophysiology, 7(1), 63–68.
Fisher, J. D., & Krumerman, A. K. (2011). Tamponade detection: did you look at the heart borders (redux)? Pacing and Clinical Electrophysiology, 34(1), 8.
Ferguson, J. D., Helms, A., Mangrum, J. M., Mahapatra, S., Mason, P., Bilchick, K., et al. (2009). Catheter ablation of atrial fibrillation without fluoroscopy using intracardiac echocardiography and electroanatomic mapping. Circulation. Arrhythmia and Electrophysiology, 2(6), 611–619.
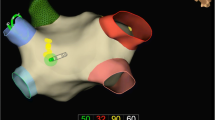
Gallagher, A. G., & Cates, C. U. (2004). Virtual reality training for the operating room and cardiac catheterisation laboratory. Lancet, 364(9444), 1538–1540.
Di Biase, L., Paoletti Perini, A., Mohanty, P., Goldenberg, A. S., Grifoni, G., Santangeli, P., et al. (2014). Visual, tactile, and contact force feedback: which one is more important for catheter ablation? Results from an in vitro experimental study. Heart Rhythm, 11(3), 506–513.
Nestel, D., Groom, J., Eikeland-Husebo, S., & O’Donnell, J. M. (2011). Simulation for learning and teaching procedural skills: the state of the science. Simulation in Healthcare, 6(Suppl), S10–13.
De Ponti, R., Marazzi, R., Doni, L. A., Tamborini, C., Ghiringhelli, S., & Salerno-Uriarte, J. A. (2012). Simulator training reduces radiation exposure and improves trainees’ performance in placing electrophysiologic catheters during patient-based procedures. Heart Rhythm, 9(8), 1280–1285.
De Ponti, R., Marazzi, R., Ghiringhelli, S., Salerno-Uriarte, J. A., Calkins, H., & Cheng, A. (2011). Superiority of simulator-based training compared with conventional training methodologies in the performance of transseptal catheterization. Journal of the American College of Cardiology, 58(4), 359–363.
Stabile, G., Solimene, F., Calo, L., Anselmino, M., Castro, A., Pratola, C., et al. (2014). Catheter-tissue contact force for pulmonary veins isolation: a pilot multicentre study on effect on procedure and fluoroscopy time. Europace, 16(3), 335–340.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Andrew Krumerman is consultant for Biosense Inc., Biotronik Inc., and Speak2mdbyphone.com.
Additional information
Jorge Romero and Florentino Lupercio contributed equally to this work.
Rights and permissions
About this article
Cite this article
Romero, J., Lupercio, F., Goodman-Meza, D. et al. Electroanatomic mapping systems (CARTO/EnSite NavX) vs. conventional mapping for ablation procedures in a training program. J Interv Card Electrophysiol 45, 71–80 (2016). https://doi.org/10.1007/s10840-015-0073-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0073-6