Abstract
Introduction
Patent foramen ovale (PFO) has been recently implicated as a strong predictor of stroke or transient ischemic attack (TIA) in patients with implanted pacemaker or defibrillation leads. Leads in the right heart can form thrombi that embolize to the pulmonary circulation and raise pulmonary pressure. This increases right-to-left shunting through PFO or intrapulmonary shunts and can result in paradoxical embolism. We sought to determine whether certain lead characteristics confer a higher thrombogenic risk resulting in stroke/TIAs in patients either with or without a PFO.
Methods
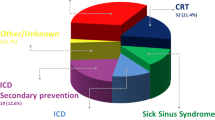
We retrospectively analyzed 5,646 patients (mean age 67.3 ± 16.3 years, 64 % male) who had endocardial device leads implanted in 2000–2010. We performed univariate and multivariate-adjusted proportional hazards models to determine association of lead characteristics with stroke/TIA during follow-up.
Results
On univariate analysis, passively fixated tined leads were associated with more stroke/TIAs (HR 1.77, 95 % CI 1.27, 2.47; p < 0.001), whereas presence of defibrillation coil was associated with fewer stroke/TIAs (HR 0.59, 95 % CI 0.42–0.84; p = 0.003). Number of leads per patient, presence of atrial lead, maximum lead size, tip shape, and type of insulating material were not associated with stoke/TIA. On multivariate analyses adjusting for age, sex, diagnosis of PFO, and prior history of stroke/TIA, the presence of tined leads was associated with stroke/TIA (HR 1.41, 95 % CI 1.00–1.97; p = 0.049). Defibrillation coils were no longer associated with lower stroke/TIA on multivariate analysis.
Conclusions
Most physical characteristics of contemporary leads do not impact rate of stroke/TIA among patients receiving implantable devices. The presence of a PFO is a major risk factor for stroke/TIA in patients with endovascular leads.




Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- CIED:
-
Cardiovascular implantable electronic device
- HR:
-
Hazard ratio
- PFO:
-
Patent foramen ovale
- RVSP:
-
Right ventricular systolic pressure
- TIA:
-
Transient ischemic attack
References
Epstein, A. E., DiMarco, J. P., Ellenbogen, K. A., et al. (2013). 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 61, e6–e75.
van Rees, J. B., de Bie, M. K., Thijssen, J., et al. (2011). Implantation-related complications of implantable cardioverter-defibrillators and cardiac resynchronization therapy devices: a systematic review of randomized clinical trials. Journal of the American College of Cardiology, 58, 995–1000.
Greenspon, A. J., Patel, J. D., Lau, E., et al. (2012). Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. Journal of the American College of Cardiology, 60, 1540–1545.
Korkeila, P. J., Saraste, M. K., Nyman, K. M., et al. (2006). Transesophageal echocardiography in the diagnosis of thrombosis associated with permanent transvenous pacemaker electrodes. Pacing and Clinical Electrophysiology, 29, 1245–1250.
Fehske, W., Jung, W., Omran, H., et al. (1995). Multiplane transesophageal echocardiographic evaluation of transvenous defibrillation leads. Journal of Clinical Ultrasound, 23, 153–162.
Alizadeh, A., Maleki, M., Bassiri, H., et al. (2006). Evaluation of atrial thrombus formation and atrial appendage function in patients with pacemaker by transesophageal echocardiography. Pacing and Clinical Electrophysiology, 29, 1251–1254.
Supple, G. E., Ren, J. F., Zado, E. S., et al. (2011). Mobile thrombus on device leads in patients undergoing ablation: identification, incidence, location, and association with increased pulmonary artery systolic pressure. Circulation, 124, 772–778.
Chow, B., & Tang, A. (2005). Pulmonary embolism in a man with an implantable cardioverter defibrillator. CMAJ, 173, 487.
van Rooden, C. J., Molhoek, S. G., Rosendaal, F. R., et al. (2004). Incidence and risk factors of early venous thrombosis associated with permanent pacemaker leads. Journal of Cardiovascular Electrophysiology, 15, 1258–1262.
Korkeila, P., Mustonen, P., Koistinen, J., et al. (2010). Clinical and laboratory risk factors of thrombotic complications after pacemaker implantation: a prospective study. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology : Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 12, 817–824.
Novak, M., Dvorak, P., Kamaryt, P., et al. (2009). Autopsy and clinical context in deceased patients with implanted pacemakers and defibrillators: intracardiac findings near their leads and electrodes. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology : Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 11, 1510–1516.
Desimone, C. V., Desimone, D. C., Hagler, D. J., et al. (2013). Cardioembolic stroke in patients with patent foramen ovale and implanted cardiac leads. Pacing and Clinical Electrophysiology, 36, 50–54.
DeSimone, C. V., DeSimone, D. C., Patel, N. A., et al. (2012). Implantable cardiac devices with patent foramen ovale–a risk factor for cardioembolic stroke? Journal of Interventional Cardiac Electrophysiology, 35, 159–162.
Velthuis, S., Buscarini, E., van Gent, M. W., et al. (2013). Grade of pulmonary right-to-left shunt on contrast echocardiography and cerebral complications: a striking association. Chest, 144(2):542–8.
Abushora, M. Y., Bhatia, N., Alnabki, Z., et al. (2013). Intrapulmonary shunt is a potentially unrecognized cause of ischemic stroke and transient ischemic attack. Journal of the American Society of Echocardiography, 26, 683–690.
DeSimone, C. V., Friedman, P. A., Noheria, A., et al. (2013). Stroke or transient ischemic attack in patients with transvenous pacemaker or defibrillator and echocardiographically detected patent foramen ovale. Circulation, 128, 1433–1441.
Tobis, J., & Shenoda, M. (2012). Percutaneous treatment of patent foramen ovale and atrial septal defects. Journal of the American College of Cardiology, 60, 1722–1732.
Marriott, K., Manins, V., Forshaw, A., et al. (2013). Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. Journal of the American Society of Echocardiography, 26, 96–102.
Woods, T. D., & Patel, A. (2006). A critical review of patent foramen ovale detection using saline contrast echocardiography: when bubbles lie. Journal of the American Society of Echocardiography, 19, 215–222.
Lovering, A. T., Elliott, J. E., Beasley, K. M., et al. (2010). Pulmonary pathways and mechanisms regulating transpulmonary shunting into the general circulation: an update. Injury, 41(Suppl 2), S16–S23.
Ozcan, C., Jahangir, A., Friedman, P. A., et al. (2001). Long-term survival after ablation of the atrioventricular node and implantation of a permanent pacemaker in patients with atrial fibrillation. New England Journal of Medicine, 344, 1043–1051.
DeSimone, C. V., DeSimone, D. C., Patel, N. A., et al. (2012). Implantable cardiac devices with patent foramen ovale—a risk factor for cardioembolic stroke? Journal of Interventional Cardiac Electrophysiology, 35, 159–162.
Laurie, S. S., Yang, X., Elliott, J. E., et al. (2010). Hypoxia-induced intrapulmonary arteriovenous shunting at rest in healthy humans. Journal of Applied Physiology, 109, 1072–1079.
Lovering, A. T., Romer, L. M., Haverkamp, H. C., et al. (2008). Intrapulmonary shunting and pulmonary gas exchange during normoxic and hypoxic exercise in healthy humans. Journal of Applied Physiology, 104, 1418–1425.
Haghjoo, M., Nikoo, M. H., Fazelifar, A. F., et al. (2007). Predictors of venous obstruction following pacemaker or implantable cardioverter-defibrillator implantation: a contrast venographic study on 100 patients admitted for generator change, lead revision, or device upgrade. Europace, 9, 328–332.
Korkeila, P., Nyman, K., Ylitalo, A., et al. (2007). Venous obstruction after pacemaker implantation. Pacing and Clinical Electrophysiology, 30, 199–206.
Rozmus, G., Daubert, J. P., Huang, D. T., et al. (2005). Venous thrombosis and stenosis after implantation of pacemakers and defibrillators. Journal of Interventional Cardiac Electrophysiology, 13, 9–19.
Bulur, S., Vural, A., Yazici, M., et al. (2010). Incidence and predictors of subclavian vein obstruction following biventricular device implantation. Journal of Interventional Cardiac Electrophysiology, 29, 199–202.
Bracke, F., Meijer, A., & Van Gelder, B. (2003). Venous occlusion of the access vein in patients referred for lead extraction: influence of patient and lead characteristics. Pacing and Clinical Electrophysiology, 26, 1649–1652.
de Cock, C. C., Vinkers, M., Van Campe, L. C., et al. (2000). Long-term outcome of patients with multiple (> or = 3) noninfected transvenous leads: a clinical and echocardiographic study. Pacing and Clinical Electrophysiology, 23, 423–426.
Reinig, M., White, M., Levine, M., et al. (2007). Left ventricular endocardial pacing: a transarterial approach. Pacing and Clinical Electrophysiology, 30, 1464–1468.
Chow, B. J., Hassan, A. H., Chan, K. L., et al. (2003). Prevalence and significance of lead-related thrombi in patients with implantable cardioverter defibrillators. American Journal of Cardiology, 91, 88–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vaidya, V.R., DeSimone, C.V., Asirvatham, S.J. et al. Implanted endocardial lead characteristics and risk of stroke or transient ischemic attack. J Interv Card Electrophysiol 41, 31–38 (2014). https://doi.org/10.1007/s10840-014-9900-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-014-9900-4