Abstract
Purpose
Intrathoracic impedance monitoring is useful for heart failure (HF) management in patients with cardiac resynchronization therapy (CRT). However, more accurate identification of worsening chronic HF (CHF) is required in the clinical setting. We investigated this issue by estimating changes in impedance.
Methods
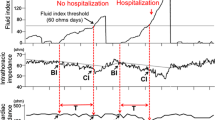
We studied 38 CHF patients (29 males, mean age 67 years) with CRT-defibrillator capable of impedance monitoring. During the follow-up period (20.7 ± 7.8 months), the subjects experienced a total of 129 fluid index threshold (60 ohm·days) crossing events. These events were divided into two groups: HF events (n = 70) and no HF events (n = 59). Based on the impedance at the beginning of increasing fluid index (S) and at the crossing of 60 ohm·days (E), the rate of impedance change (S − E / S) was estimated. In addition, the elapsed time from S to E (T) was evaluated. Then, we calculated the rate of impedance change per day (S − E / S × T) in each group.
Results
The rate of impedance change per day was significantly higher in HF events than in no HF events (0.86 ± 0.48 vs. 0.37 ± 0.22 %/day, P < 0.01). By receiver operating characteristic curve for identification of HF events, the best cutoff value of the rate of impedance change was 0.48 %/day (sensitivity 80 %, specificity 81 %, and area under the curve 0.85).
Conclusions
These results suggest that a faster drop in intrathoracic impedance reflected worsening CHF in patients with CRT-defibrillator. Thus, intrathoracic impedance monitoring based on the rate of impedance change may provide a more accurate identification of worsening CHF.



Similar content being viewed by others
References
Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators, Cleland, J. G., Daubert, J. C., Erdmann, E., Freemantle, N., Gras, D., Kappenberger, L., et al. (2005). The effect of cardiac resynchronization on morbidity and mortality in heart failure. New England Journal of Medicine, 352, 1539–1549.
Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators, Bristow, M. R., Saxon, L. A., Boehmer, J., Krueger, S., Kass, D. A., De Marco, T., et al. (2004). Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. New England Journal of Medicine, 350, 2140–2150.
Multicenter InSync Randomized Clinical Evaluation, Abraham, W. T., Fisher, W. G., Smith, A. L., Delurgio, D. B., Leon, A. R., Loh, E., et al. (2002). Cardiac resynchronization in chronic heart failure. New England Journal of Medicine, 346, 1845–1853.
Yu, C. M., Fung, W. H., Lin, H., Zhang, Q., Sanderson, J. E., & Lau, C. P. (2003). Predictors of left ventricular reverse remodeling after cardiac resynchronization therapy for heart failure secondary to idiopathic dilated or ischemic cardiomyopathy. American Journal of Cardiology, 91, 684–688.
Yu, C. M., Wang, L., Chau, E., Chan, R. H., Kong, S. L., Tang, M. O., et al. (2005). Intrathoracic impedance monitoring in patients with heart failure: correlation with fluid status and feasibility of early warning preceding hospitalization. Circulation, 112, 841–848.
Small, R. S., Wickemeyer, W., Germany, R., Hoppe, B., Andrulli, J., Brady, P. A., et al. (2009). Changes in intrathoracic impedance are associated with subsequent risk of hospitalizations for acute decompensated heart failure: clinical utility of implanted device monitoring without a patient alert. Journal of Cardiac Failure, 15, 475–481.
FAST Study Investigators, Abraham, W. T., Compton, S., Haas, G., Foreman, B., Canby, R. C., Fishel, R., et al. (2011). Intrathoracic impedance vs daily weight monitoring for predicting worsening heart failure events: results of the Fluid Accumulation Status Trial (FAST). Congestive Heart Failure, 17, 51–55.
Wang, L. (2007). Key lessons from cases worldwide. American Journal of Cardiology, 99, 34G–40G.
McKee, P. A., Castelli, W. P., McNamara, P. M., & Kannel, W. B. (1971). The natural history of congestive heart failure: the Framingham Study. New England Journal of Medicine, 285, 1441–1446.
Soga, Y., Ando, K., Arita, T., Hyodo, M., Goya, M., Iwabuchi, M., et al. (2011). Efficacy of fluid assessment based on intrathoracic impedance monitoring in patients with systolic heart failure. Circulation Journal, 75, 129–134.
Ypenburg, C., Bax, J. J., van der Wall, E. E., Schalij, M. J., & van Erven, L. (2007). Intrathoracic impedance monitoring to predict decompensated heart failure. American Journal of Cardiology, 99, 554–557.
Conflict of interest
We received no financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamada, S., Suzuki, H., Kamiyama, Y. et al. Predictive impact of the decreasing rate of intrathoracic impedance in worsening chronic heart failure. J Interv Card Electrophysiol 40, 87–91 (2014). https://doi.org/10.1007/s10840-014-9881-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-014-9881-3