Abstract
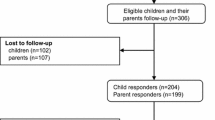
Pediatric acquired disability challenges children and their parents as they adjust to a new reality of physical impairment. This longitudinal study explored the association between severity of children’s acquired disability and children and parents’ adjustment six weeks after diagnosis (T1) and three-four months later (T2), particularly focusing on parental perception of illness and of parent–child interactions. The participants were 140 parents of children with acquired disability who were hospitalized in pediatric or rehabilitation departments at three major medical centers in Israel. Parents completed questionnaires on background information, parental illness perception, perception of parent–child interactions, and child and parents’ adjustment. Physicians and nurses completed a questionnaire on disability severity indexes. The results revealed that severity of child’s disability correlated positively with parental illness perception and adjustment, but not with parental perception of parent–child interactions. At both time points, parents’ adjustment correlated negatively with illness perceptions and positively with perception of parent–child interactions. Parents’ adjustment was partially associated with children’s adjustment. Children and parents’ adjustment improved over time, as the severity of the child’s disability decreased and parental illness perception eased. Parental perception of parent–child interactions did not change significantly. Parents’ initial adjustment at T1 correlated with their children’s subsequent adjustment, but not vice versa. The study showed that parental adjustment affects children’s adjustment to the acquired disability, and demonstrated the role of parental perception. Early identification of parents at risk might facilitate appropriate professional intervention.
Highlights
-
Parental adjustment plays an important role in the child’s adjustment to the acquired disability over time.
-
Early intervention for parents can help prevent the development of maladaptive adjustment in both parents and children over time.
-
Disability severity and parental perception of the child–parent relationship and the illness are associated with the parents’ adjustment to the new, complex reality.


Similar content being viewed by others
References
Abidin, R. R. (1983). Parenting stress index-manual. Charlottesville, VA: Pediatric Psychology Press. https://doi.org/10.1037/t02445-000.
Anderson, V., Godfrey, C., Rosenfeld, J. V., & Catroppa, C. (2012). Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics, 129, 254–262. https://doi.org/10.1542/peds.2011-0311.
Arbuckle, J. L. (2007). Amos 16.0 user’s guide. USA: Amos Development Corporation.
Babikian, T., Merkley, T., Savage, R. C., Giza, C. C., & Levin, H. (2015). Journal of Neurotrauma, 32(23), 1849–1860. https://doi.org/10.1089/neu.2015.3971.
Bakker, A., Martens, K. J. P., Van-Son, M. J. M., & Van-Loey, N. E. E. (2013). Psychological consequences of pediatric burns from a child and family perspective: a review of the empirical literature. Clinical Psychology Review, 33(3), 361–371. https://doi.org/10.1016/j.cpr.2012.12.006.
Barak, S., Elad, D., Silberg, T., & Brezner, A. (2017). Mothers and fathers of children with cerebral palsy: differences in future expectations. Journal of Developmental and Physical Disabilities, 29(2), 223–240. https://doi.org/10.1007/s10882-016-9521-1.
Barbot, B., Crossman, E., Hunter, S. R., Grigorenko, E., & Luthar, S. S. (2014). Reciprocal influences between maternal parenting and child adjustment in a high-risk population: a 5-years cross-lagged analysis of bidirectional effects. American Journal of Orthopsychiatry, 84(5), 567–580. https://doi.org/10.1037/ort0000012.
Barroso, N. E., Hungerford, G. M., Garcia, D., Graziano, P. A., & Bagner, D. (2016). Psychometric properties of the parenting stress index-short form (PSI-SF) in a high-risk sample of mothers and their infants. Psychological Assessment, 28(10), 1331–1335. https://doi.org/10.1037/pas0000257.
Benyamini, Y., Goner-Shiloh, D., & Lazarov, A. (2012). Illness perception and quality of life in patients with contact dermatitis. Contact Dermatitis, 67(4), 193–199. https://doi.org/10.1111/j.1600-0536.2012.02071.x.
Bornstein, M. H., Cote, L. R., Haynes, O. M., Hahn, C.-S., & Park, Y. (2010). Parenting knowledge: experiential and socio-demographic factors in European American mothers of young children. Developmental Psychology, 46(6), 1677–1693. https://doi.org/10.1037/a0020677.
Broadbent, E., Petrie, K. J., Main, J., & Weinman, J. (2006). The brief illness perception questionnaire. Journal of Psychosomatic Research, 60, 631–637. https://doi.org/10.1016/j.jpsychores.2005.10.020.
Broadbent, E., Wilkes, C., Koschwanez, Weinman, J., Norton, S., & Petrie, K. J. (2015). A systematic review and meta-analysis of the brief illness perception questionnaire. Journal of Psychology and Health, 30(11), 1361–1385. https://doi.org/10.1080/08870446.2015.1070851.
Bugental, D. B., & Johnston, C. (2000). Parental and child cognitions in the context of the family. Annual Review of Psychology, 51, 315–344. https://doi.org/10.1146/annurev.psych.51.1.315.
Byrne, B. M. (2016). Structural equation modeling with EQS: basic concepts, applications, and programming. 3nd ed. Routledge: Taylor & Francis.
Cespedes, A. (2018). An examination of the relationships between family functioning, asthma self-care behaviors, and asthma-related morbidity in young, urban Latino and African American adolescents with uncontrolled asthma. Doctoral dissertation. New York: New York University College of Global Public Health, ProQuest Dissertations, Publishing.
Chevignard, M., Toure, H., Brugel, D. G., Poirier, J., & Laurent‐Vannier, A. (2010). A comprehensive model of care for rehabilitation of children with acquired brain injuries. Child: Care, Health and Development, 36(1), 31–43. https://doi.org/10.1111/j.1365-2214.2009.00949.x.
Colalillo, S., Miller, N. V., & Johnston, C. (2015). Mother and father attributions for child misbehavior: relations to child internalizing and externalizing problems. Journal of Social and Clinical Psychology, 34(9), 788–808. https://doi.org/10.1521/jscp.2015.34.9.788.
Fanti, K. A., Panayiotou, G., & Fanti, S. (2013). Associating parental to child psychological symptoms: investigating a transactional model of development. Journal of Emotional and Behavioral Disorders, 21(3), 193–210. https://doi.org/10.1177/1063426611432171.
Florian, V., & Drori, Y. (1990). Mental health index (MHI): psychometric features and normative data among the Israeli population. Psychologia—Israel. Journal of Psychology, 2, 26–36.
Gewirtz, A., Forgatch, M., & Wieling, E. (2008). Parenting practices as potential mechanisms for child adjustment following mass trauma. Journal of Marital and Family Therapy, 34(2), 177–192. https://doi.org/10.1111/j.1752-0606.2008.00063.x.
Godoy-Izquierdo, D., Lopez-Chicheri, I., Lopez-Torrecillas, F., Velez, M., & Godoy, J. F. (2007). Contents of lay illness models dimensions for physical and mental diseases and implications for health professionals. Patient Education and Counseling, 67(1–2), 196–213. https://doi.org/10.1016/j.pec.2007.03.016.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of American Academy of Child & Adolescent, 40, 1337–1345. https://doi.org/10.1097/00004583-200111000-00015.
Goodman, R., Renfrew, D., & Mullick, M. (2000). Predicting type of psychiatric disorder from strengths and difficulties questionnaire (SDQ) scores in child mental health clinics in London and Dhaka. Journal of Child & Adolescent Psychiatry, 9(2), 129–134. https://doi.org/10.1007/s007870050008.
Grigorian, A., Nahmias, G., Dolich, M., Barrios, C., Schubl, S. D., Sheehan, B., & Lekawa, M. (2019). Increased risk of head injury in pediatric patients with attention deficit hyperactivity disorder. Journal of Child and Adolescent Psychiatric Nursing, 32, 171–176. https://doi.org/10.1111/jcap.12246.
Guerrier, D., & McKeever, P. (1997). Mothering children who survive brain injuries: playing the hand you’re dealt. Journal Society of Pediatric Nurses, 2, 105–115.
Hagger, M. S., & Orbell, S. (2003). A meta-analytic review of common-sense model of illness representations. Psychology and Health, 18, 141–184. https://doi.org/10.1080/088704403100081321.
Haley, S. M., Coster, W. J., Ludlow, L. H., Haltiwanger, & Andrellos, P. (1992). Pediatric evaluation of disability inventory (PEDI). Developmental, standardization and administration manual. Boston MA: Boston University.
Hassall, R., Rose, J., & McDonald, J. (2005). Parenting stress in mothers of children with an intellectual disability: the effects of parental cognitions in relation to child characteristics and family support. Journal of Intellectual Disability Research, 49(6), 405–418. https://doi.org/10.1111/j.1365-2788.2005.00673.x.
Hawley, C. A., Ward, A. B., Magnay, A. R., & Long, J. (2003). Parental stress and burden following traumatic brain injury amongst children and adolescents. Brain Injury, 17, 1–23. https://doi.org/10.1080/0269905021000010096.
Hayduk, L. A., & Littvay, L. (2012). Should researchers use single indicators, best indicators, or multiple indicators in structural equation models? Medical Research Methodology, 12(159), 1–17. https://doi.org/10.1186/1471-2288-12-159.
Hoh, N. Z., Wagner, A. K., Alexander, S. A., Clark, R. B., & Beers, S. R. (2010). BCL2 genotypes: functional and neurobehavioral outcomes after severe traumatic brain injury. Journal of Neurotrauma, 27(8), 1413–1427. https://doi.org/10.1089/neu.2009.1256.
Izsak, R. (2002). How young people adapt to the army framework: the officer’s functioning as a solid base and his contribution to the mental wellbeing and military functioning of the soldier. Unpublished Doctoral Dissertation. Ramat-Gan. (Hebrew): Bar Ilan University.
Johnston, C., Park, J. L., & Miller, N. V. (2018). Parental cognitions: relations to parenting and child behavior. Handbook of parenting and child development across the lifespan, 395–414. https://doi.org/10.1007/978-3-319-94598-9_17.
Jones, T. L., & Prinz, R. J. (2005). Potential roles of parental self-efficacy in parent and child adjustment: a review. Clinical Psychology, 25(3), 341–363. https://doi.org/10.1016/j.cpr.2004.12.004.
Kaptein, A. A., Bijsterbosch, J., Scharloo, M., Hampson, S. E., Kroon, H. M., & Kloppenburg, M. (2010). Using the common-sense model of illness perceptions to examine osteoarthritis change: a 6-year longitudinal study. Health Psychology, 29(1), 56–64. https://doi.org/10.1037/a0017787.
Kazak, A. E, Rourke, M. T., & Navsaria, N. (2009). Families and other systems in pediatric psychology. In M. Roberts, R. Steele (Eds), Handbook of pediatric psychology (pp. 656–671). New York, NY: Guilford.
Kesler, A., Kliper, E., Goner-Shilo, D., & Benyamini, Y. (2009). Illness perceptions and quality of life amongst women with pseudo tumor cerebri. European Journal of Neurology, 16, 931–36. https://doi.org/10.1111/j.1468-1331.2009.02625.x.
Lalonde, G., Bernier, A., Beaudoin, C., Gravel, G., & Beauchamp, M. H. (2018). Investigating social functioning after early mild TBI: the quality of parent–child interactions. Journal of Neuropsychology, 12(1), 1–22. https://doi.org/10.1111/jnp.12104.
Leventhal, H., Brissette, I., & Leventhal, E. A. (2003). In L. D. Cameron, H. Leventhal (Eds), The common-sense model of self-regulation of health and illness behavior. Ch 3. (pp. 42–65). London: Routledge.
Leventhal, H., Meyer, D., & Nerenz, D. R. (1980). The common-sense representation of illness danger. In S. Rachman (Ed.), Contributions to medical psychology (pp. 17–30). New York, NY: Pergamon.
Maimaran, A. (2007). Stress factors, coping strategies, and adaptation in mothers of chronically ill children. Israel. (Hebrew): Thesis submitted for the degree of Doctor of Philosophy at the Hebrew University.
Manor, I., Gutnik, I., Ben-Dor, D. H., Apter, A., Sever, J., Tyano, S., Weizman, A., & Zalsman, G. (2010). Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents: a pilot study. European Psychiatry, 25(3), 146–150. https://doi.org/10.1016/j.eurpsy.2009.06.001.
Marsac, M., Donlon, K. A., Winston, F., & Kassam‐Adams, N. (2013). Child coping, parent coping assistance, and post‐traumatic stress following pediatric physical injury. Child: Care Health. https://doi.org/10.1111/j.1365-2214.2011.01328.x.
McDonald Culp, A. (2010). The transactional model of development: how children and contexts shape each other. Infant Mental Health Journal, 31(1), 115–117. https://doi.org/10.1002/imhj.20246.
McNally, K. A., Bangert, B., Dietrich, A., Nuss, K., Rusin, J., Wright, M., Taylor, H. G., & Yeates, K. O. (2013). Injury versus non-injury factors as predictors of post concussive symptoms following mild traumatic brain injury in children. Neuropsychology, 27(1), 1–12. https://doi.org/10.1037/a0031370.
McSherry, D., Malet, M. F., & Weatherall, K. (2019). The strengths and difficulties questionnaire (SDQ): a proxy measure of parenting stress. The British Journal of Social Work, 49(1), 96–115. https://doi.org/10.1093/bjsw/bcy021.
Molzon, E. S., Mullins, L. L., Cushing, C. C., Chaney, J. M., McNall, R., & Mayes, S. (2018). The relationship between barriers to care, caregiver distress, and child health-related quality of life in caregivers of children with cancer: a structural equation modeling approach. Children’s Health Care, 47(1), 1–15. https://doi.org/10.1080/02739615.2016.1275639.
Moss-Morris, R., Weinman, J., Petrie, K., Horne, R., Cameron, L., & Buick, D. (2008). The revised illness perception questionnaire (IPQ-R). Psychology & Health, 17(1), 1–16. https://doi.org/10.1080/08870440290001494.
Muscara, F., Catroppa, C., Eren, S., & Anderson, V. (2009). The impact of injury severity on long-term social outcome following pediatric traumatic brain injury. Neuropsychological Rehabilitation, 19(4), 541–561. https://doi.org/10.1080/09602010802365223.
Muscara, F., McCarthy, M. C., Hearps, S. J., Nicholson, J. M., Burke, K., Dimovski, A., & Anderson, V. A. (2018). Featured article: trajectories of posttraumatic stress symptoms in parents of children with a serious childhood illness or injury. Journal of Pediatric Psychology, 43(10), 1072–1082. https://doi.org/10.1093/jpepsy/jsy035.
Murphy, L. K., Preacher, K. J., Rights, J. D., Rodriguez, E. M., Bemis, H., Desjardins, L., & Compas, B. E. (2018). Maternal communication in childhood cancer: factor analysis and relation to maternal distress. Journal of Pediatric Psychology, 43(10), 1114–1127. https://doi.org/10.1093/jpepsy/jsy054.
Murphy, L. K., Murray, C. B., & Compas, B. E. (2017). Topical review: integrating findings on direct observation of family communication in studies comparing pediatric chronic illness and typically developing samples. Journal of Pediatric Psychology, 42, 85–94. https://doi.org/10.1093/jpepsy/jsw051.
Myers, R. P., Krajden, M., Bilodeau, M., Kaita, K., Marotta, P., Peltekian, K., & Sherman, M. (2013). Burden of disease and cost of chronic hepatitis c virus infection in Canada. Canadian Journal of Gastroenterology and Hepatology, 28(5), 243–250. https://doi.org/10.1155/2014/317623.
O’Boyle, E. H., & Williams, L. J. (2010). Decomposing model fit: measurement vs. theory in organizational research using latent variables. Journal of Applied Psychology, Aug 16, No Pagination Specified. https://doi.org/10.1037/a0020539.
Olsen, B., Berg, C. A., & Wiebe, D. J. (2008). Dissimilarity in mother and adolescent illness representations of type 1 diabetes and negative emotional adjustment. Psychology and Health, 23(1), 113–129. https://doi.org/10.1080/08870440701437343.
Rappaport, M., Hall, K. M., Hopkins, K., Belleza, T., & Cope, D. N. (1982). Disability rating scale for severe head trauma: coma to community. Archives of Physical and Medical Rehabilitation, 63, 118–123.
Rodrigue, J. R., Geffken, G. R., Clark, J. E., Hunt, F., & Fishel, P. (2010). Parenting satisfaction and efficacy among caregivers of children with diabetes. Journal of Children’s Health Care, 23(3), 181–191. https://doi.org/10.1207/s15326888chc2303-3.
Rodriguez, E. M., Dunn, M. J., Zuckerman, T., Vannatta, K., Gerhardt, C. A., & Compas, B. E. (2012). Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology, 37, 185–197. https://doi.org/10.1093/jpepsy/jsr054.
Rubin, S. S. (1992). Adult child loss and the two-track model of bereavement. Omega: Journal of Death and Dying, 24(3), 183–202. https://doi.org/10.2190/2V09-H301-YMGG-M065.
Rubin, S. S., & Bar-Nadav, O. (2016). The two-track bereavement questionnaire for complicated grief (TTBQ-CG31). In R. Neimeyer (Ed), Techniques of grief therapy (pp. 87–98). New York, NY: Routledge. vol. 2. https://doi.org/10.4324/9781315692401.
Rubin, S. S., Malkinson, R., & Witztum, E. (2016). The multiple faces of loss and bereavement: theory and therapy. Haifa: Pardes publishers. (Hebrew).
Salewski, C. (2003). Illness representations in families with a chronically ill adolescent: differences between family members and impact on patients’ outcome variables. Journal of Health Psychology, 8(5), 587–598. https://doi.org/10.1177/13591053030085009.
Salvador, Á., Crespo, C., Martins, A. R., Santos, S., & Canavarro, M. C. (2015). Parents’ perceptions about their child’s illness in pediatric cancer: links with caregiving burden and quality of life. Journal of Child and Family Studies, 24(4), 1129–1140. https://doi.org/10.1007/s10826-014-9921-8.
Schlomer, G. L., Bauman, S., & Card, N. A. (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. https://doi.org/10.1037/a0018082.
Sharry, J. M., Moss-Morris, R., & Kendrick, T. (2011). Illness perceptions and glycaemic control in diabetes: a systematic review with meta-analysis. Diabetic Medicine, 28(11), 1300–1310. https://doi.org/10.1111/j.1464-5491.2011.03298.x.
Silva, N., Crespo, C., & Canavarro, M. C. (2014). Transactional paths between children and parents in pediatric asthma: associations between family relationships and adaptation. Journal of Child and Family Studies, 23(2), 360–372. https://doi.org/10.1007/s10826-013-9734-1.
Stafford, L., Jackson, H. J., & Berg, M. (2008). Illness beliefs about heart disease and adherence to secondary prevention regimens. Psychosomatic Medicine, 70(8), 942–948. https://doi.org/10.1097/PSY.0b013e318187e22e.
Stancin, T., Wade, S. L., Walz, N. C., Yeates, K. O., & Taylor, H. G. (2008). Traumatic brain injuries in early childhood: initial impact on the family. Journal of Developmental and Behavioral Pediatrics, 29(4), 253–261. https://doi.org/10.1097/DBP.0b013e31816b6b0f.
Stanton, A. L., Revenson, T. A., & Tennen, H. (2007). Health psychology: psychological adjustment to chronic disease. Annual Review of Psychology, 58, 565–592.
Steenbeek, D., Gorter, J. W., Ketelaar, M., Galama, K., & Lindeman, E. (2011). Responsiveness of goal attainment scaling in comparison to two standardized measures in outcome evaluation of children with cerebral palsy. Clinical Rehabilitation, 25(12), 1128–1139.
Tasmoc, A., Hogas, S., & Covic, A. (2013). A longitudinal study on illness perceptions in hemodialysis patients: changes over time. Archives of Medical Science, 9(5), 831–836. https://doi.org/10.5114/aoms.2013.38678.
Teti, D. M., & Cole, P. M. (2011). Parenting at risk: new perspectives, new approaches. Journal of Family Psychology, 25(5), 625–634. https://doi.org/10.1037/a0025287.
Theadom, A., Barker-Collo, S., Feigin, V. L., Starkey, N. J., Jones, K., & Barber, P. A. (2012). The spectrum captured: a methodological approach to studying incidence and outcomes of traumatic brain injury on a population level. Neuroepidemiology, 38(1), 18–29. https://doi.org/10.1159/000334746.
Tracy, E. T., Englum, B. R., Barbas, A. S., Foley, C., Rice, H. E., & Shapiro, M. L. (2013). Pediatric injury patterns by year of age. Journal of Pediatric Surgery, 48(6), 1384–1388. https://doi.org/10.1016/j.jpedsurg.2013.03.041.
Trenchard, S. O., Rust, S., & Bunton, P. (2013). A systematic review of psychosocial outcomes within 2 years of pediatric traumatic brain injury in a school-aged population. Brain Injury, 27(11), 1217–1237. https://doi.org/10.3109/02699052.2013.812240.
Wade, S. L., Walz, N. C., Cassedy, A., Taylor, H. G., Stancin, T., & Yeats, K. O. (2010). Caregiver functioning following early childhood TBI: do moms and dads respond differently? Neuro Rehabilitation, 27, 63–72. https://doi.org/10.3233/NRE-2010-0581.
Watson, S. L., Hayes, S. A., & Radford-Paz, E. (2011). Diagnose me please!: a review of research about the journey and initial impact of parents seeking a diagnosis of developmental disability for their child. International Review of Research in Developmental Disabilities, 41, 31–71. https://doi.org/10.1016/B978-0-12-386495-6.00002-3.
Weiss, J. A., MacMullin, J. A., & Lunsky, Y. (2015). Empowerment and parent gain as mediators and moderators of distress in mothers of children with autism spectrum disorders. Journal of Child and Family Studies, 24(7), 2038–2045. https://doi.org/10.1007/s10826-014-0004-7.
Yeates, K. O., Beauchamp, M, Craig, W. on behalf of Pediatric Emergency Research Canada (PERC), et al. (2017). Advancing concussion assessment in pediatrics (A-CAP): a prospective, concurrent cohort, longitudinal study of mild traumatic brain injury in children: study protocol. BMJ Open, 7:e017012. https://doi.org/10.1136/bmjopen-2017-017012.
Yehene, E., Brezner, A., Ben-Valid, S., Golan, S., Bar-Nadav, O., & Landa, J. (2019). Factors associated with parental grief reaction following pediatric acquired brain injury. Neuropsychological Rehabilitation, 26, 1–24. https://doi.org/10.1080/09602011.2019.1668280.
Youngblut, J. M., & Brooten, D. (2008). Mother’s mental health, mother-child relationship, and family functioning 3 months after a preschooler’s head injury. Journal of Head Trauma Rehabilitation, 23(2), 92–102. https://doi.org/10.1097/01.HTR.0000314528.85758.30.
Zautra, A. J., Potter, P. T., & Reich, J. W. (1997). The independence of affects is context-dependent: an integrative model of the relationship between positive and negative affect. In M. P. Lawton (Series Ed.) & K. W. Schaie & M. P. Lawton (Eds), Annual review of gerontology and geriatrics, 17. Focus on adult development (pp. 75–103). New York: Springer.
Zung, W. W., Brodhead, W. E., & Roth, M. E. (1993). Prevalence of depression symptom in primary care. Journal of Family Practice, 3, 337–334.
Acknowledgements
We would like to thank Professor Benyamini, Y., and Professor Ginsburg, K. for their professional guidance; Ms. Alkalay, Y. for her statistical work; and the pediatric and rehabilitation department heads at the medical centers (Dr. Brezner, A., Dr. Kornitzer, E., and Professor Kerem, E.). In addition, we want to thank the parents who openly shared their experiences, despite going through such a difficult time in their lives.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Palmor Haspel, S., Hamama, L. Pediatric Acquired Disability: Child and Parental Adjustment. J Child Fam Stud 30, 403–415 (2021). https://doi.org/10.1007/s10826-020-01894-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-020-01894-z