Abstract
Purpose
The aim of our study was to evaluate the influence of different ejaculatory abstinence time frames (several days versus 1 h) on semen parameters, blastocysts ploidy rate, and clinical results in assisted reproduction cycles on sibling oocytes.
Methods
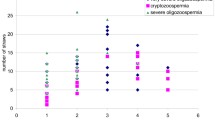
This is a prospective study including 22 preimplantation genetic testing for aneuploidy (PGT-A) cycles performed between November 2015 and December 2018. Male partners with oligoastenoteratozoospermia produced two semen samples on the day of oocyte retrieval: the first one after several days of abstinence and the second, 1 h after the first one. Oocytes from each patient were divided into two groups: those in group 1 were injected with spermatozoa from the first ejaculate (N = 121) and oocytes in group 2 with spermatozoa from the second one (N = 144). Outcomes of aniline blue test, fertilization, blastocyst formation, ploidy rates, and clinical results were compared between the two groups.
Results
Semen volume resulted lower in the second sperm retrieval. Sperm concentration, motility, and morphology were similar in the two groups. A total of 106 blasotcysts were biospied. Higher blastocyst euploidy rates resulted in group 2 (43.6%) than in group 1 (27.5%). A higher percentage of mature chromatine was observed in group 2.
Conclusion
Using spermatozoa from samples with a shorter abstinence could be a simple method to select higher quality spermatozoa, reducing aneuploidy rate in blastocysts. Prospective randomized controlled trials should be performed to confirm the potential advantage of using semen samples with short abstinence period to improve the outcome of assisted reproduction cycles.
Similar content being viewed by others
References
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Munne S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64:382–91.
Munne S, Sandalinas M, Magli C, Gianaroli L, Cohen J, Warburton D. Increased rate of aneuploid embryos in young women with previous aneuploid conceptions. Prenat Diagn. 2004;24:638–43.
Wilding M, Forman R, Hogewind G, Di Matteo L, Zullo F, Cappiello F, et al. Preimplantation genetic diagnosis for the treatment of failed in vitro fertilization-embryo transfer and habitual abortion. Fertil Steril. 2004;81:1302–7.
Silber S, Escudero T, Lenahan K, Abdelhadi I, Kilani Z, Munne S. Chromosomal abnormalities in embryos derived from testicular sperm extraction. Fertil Steril. 2003;79:30–8.
World Health Organization. Department of Reproductive Health and Research. WHO laboratory manual for the examination and processing of human semen. 5th ed. Switzerland: WHO Press; 2010. p. 10–1.
Mortimer D, Templeton AA, Lenton EA, Coleman RA. Influence of abstinence and ejaculation-to-analysis delay on semen analysis parameters of suspected infertile men. Arch Androl. 1982;8:251–6.
Jørgensen N, Andersen AG, Eustache F, Irvine DS, Suominen J, Petersen JH, et al. Regional differences in semen quality in Europe. Hum Reprod. 2001;16:1012–9.
Jørgensen N, Joensen UN, Jensen TK, Jensen MB, Almstrup K, Olesen IA, et al. Human semen quality in the new millennium: a prospective cross-sectional population based study of 4867 men. BMJ Open. 2012;2:e000990.
Makkar G, Ng EH, Yeung WS, Ho PC. A comparative study of raw and prepared semen samples from two consecutive days. J Reprod Med. 2001;46:565–72.
Levitas E, Lunenfeld E, Weiss N, Friger M, Har-Vardi I, Koifman A, et al. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83:1680–6.
Francavilla F, Barbonetti A, Necozione S, Santucci R, Cordeschi G, Macerola B, et al. Within-subject variation of seminal parameters in men with infertile marriages. Int J Androl. 2007;30:174–81.
Frank J, Confino E, Friberg J, Dudkiewicz AB, Gleicher N. Effect of ejaculation frequency on sperm quality. Arch Androl. 1986;16:203–7.
Levin RM, Latimore J, Wein AJ, Van Arsdalen KN. Correlation of sperm count with frequency of ejaculation. Fertil Steril. 1986;45:732–4.
Tonguc E, Var T, Onalan G, Altinbas S, Tokmak A, Karakas N, et al. Comparison of the effectiveness of single versus double intrauterine insemination with three different timing regimens. Fertil Steril. 2010;94:1267–70.
Lehavi O, Botchan A, Paz G, Yogev L, Kleiman SE, Yavetz H, et al. Twenty-four hours abstinence and the quality of sperm parameters. Andrologia. 2014;46:692–7.
Mayorga-Torres BJ, Camargo M, Agarwal A, du Plessis SS, Cadavid ÁP, Cardona Maya WD. Influence of ejaculation frequency on seminal parameters. Reprod Biol Endocrinol. 2015;13:47.
Olderid NB, Gordeladze JO, Kirkhus B, Purvis K. Human sperm characteristics during frequent ejaculation. J Reprod Fertil. 1984;71:135–40.
Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. 2015;13:37.
Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat. 2005;23:1–160.
Carrell DT. Epigenetics of the male gamete. Fertil Steril. 2012;97(2):267–74.
Yan W, McCarrey JR. Sex chromosome inactivation in the male. Epigenetics. 2009;4(7):452–6.
Loutradi KE, Tarlatzis BC, Goulis DG, Zepiridis L, Pagou T, Chatziioannou E, et al. The effects of sperm quality on embryo development after intracytoplasmic sperm injection. J Assist Reprod Genet. 2006;23:69–74.
Chapuis A, Gala A, Ferrières-Hoa A, Mullet T, Bringer-Deutsch S, Vintejoux E, et al. Sperm quality and paternal age: effect on blastocyst formation and pregnancy rates. Basic Clin Androl. 2017;27:2.
Ramasamy R, Chiba K, Butler P, Dolores J. Lamb Male biological clock: a critical analysis of advanced paternal age. Fertil Steril. Author manuscript; available in PMC 2016 Jul 21. Published in final edited form as: Fertil Steril. 2015;103(6):1402–6.
Puscheck EE, Jeyendran RS. The impact of male factor on recurrent pregnancy loss. Curr Opin Obstet Gynecol. 2007;19:222–8.
Depa-Martynow M, Kempisty B, Jagodziński PP, Pawelczyk L, Jedrzejczak P. Impact of protamine transcripts and their proteins on the quality and fertilization ability of sperm and the development of preimplantation embryos. Reprod Biol. 2012;12(1):57–72.
Rogenhofer N, Dansranjavin T, Schorsch M, Spiess A, Wang H, von Schönfeldt V, et al. The sperm protamine mRNA ratio as a clinical parameter to estimate the fertilizing potential of men taking part in an ART programme. Hum Reprod. 2013;28(4):969–78.
Carrell DT, Emery BR, Hammoud S. Altered protamine expression and diminished spermatogenesis: what is the link? Hum Reprod Update. 2007;13:313–27.
Rodenhiser D, Mann M. Epigenetics and human disease: translating basic biology into clinical applications. CMAJ. 2006;174(3):341–8.
Denomme MM, White CR, Gillio-Meina C, MacDonald WA, Deroo BJ, Kidder GM, et al. Compromised fertility disrupts Peg1 but not Snrpn and Peg3 imprinted methylation acquisition in mouse oocytes. Front Genet. 2012;3:129 Published online 2012 Jul 11.
Francis S, Yelumalai S, Jones C, Coward K. Aberrant protamine content in sperm and consequential implications for infertility treatment. Hum Fertil (Camb). 2014;17(2):80–9.
Greco E, Bono S, Ruberti A, Lobascio AM, Greco P, Biricik A, et al. Comparative genomic hybridization selection of blastocysts for repente implantation failure tretament: a pilot study. Biomed Res Int. 2014;2014:457913.
Minasi MG, Fiorentino F, Ruberti A, Biricik A, Cursio E, Cotroneo E, et al. Genetic diseases and aneuploidies can be detected with a single blastocyst biopsy: a successfull clinical approach. Hum Reprod. 2017;32(8):1770–7.
Alkhayal A, San Gabriel M, Zeidan K, Alrabeeah K, Noel D, McGraw R, et al. Sperm DNA and chromatin integrity in semen samples used for intrauterine insemination. J Assist Reprod Genet. 2013;30(11):1519–24.
Agarwal A, Majzoub A, Esteves SC, Ko E, Ramasamy R, Zini A. Clinical utility of sperm DNA fragmentation testing: practice recommendations based on clinical scenarios. Transl Androl Urol. 2016;5:935–50.
Alipour H, Van Der Horst G, Christiansen OB, Dardmeh F, Jørgensen N, Nielsen HI, et al. Improved sperm kinematics in semen samples collected after 2 h versus 4-7 days of ejaculation abstinence. Hum Reprod. 2017;32(7):1364–72.
Bahadur G, Almossawi O, IIlahibuccus A, Al-Habib A, Okolo S. Factors leading to pregnancies in stimulated intrauterine insemination cycles and the use of consecutive ejaculations within a small clinic environment. J Obstet Gynaecol India. 2016;66(Suppl 1):513–20.
Sugiyam R, Nakagawa K, Nishi Y, Sugiyama R, Shirai A, Inoue M. Improvement of sperm motility by short-interval sequential ejaculation in oligoasthenozoospermic patients. Arch Med Sci. 2008;4:438–42.
Bar-Hava I, Perri T, Ashkenazi J, Shelef M, Ben-Rafael Z, Orvieto R. The rationale for requesting a second consecutive sperm ejaculate for assisted reproductive technology. Gynecol Endocrinol. 2000;14(6):433–6.
De Jonge C, LaFromboise M, Bosmans E, Ombelet W, Cox A, Nijs M. Influence of the abstinence period on human sperm quality. Fertil Steril. 2004;82(1):57–65.
Asmarinah, Syauqy A, Umar LA, Lestari SW, Mansyur E, Hestiantoro A, et al. Sperm chromatin maturity and integrity correlated to zygote development in ICSI program. Syst Biol Reprod Med. 2016;62(5):309–16.
Hammadeh ME, al-Hasani S, Stieber M, Rosenbaum P, Küpker D, Diedrich K, et al. The effect of chromatin condensation (aniline blue staining) and morphology (strict criteria) of human spermatozoa on fertilization, cleavage and pregnancy rates in an intracytoplasmic sperm injection programme. Hum Reprod. 1996;11(11):2468–71.
Seli E, Gardner DK, Schoolcraft WB, Moffatt O, Sakkas D. Extent of nuclear DNA damage in ejaculated spermatozoa impacts on blastocyst development after in vitro fertilization. Fertil Steril. 2004;82:378–83.
Shubhashree U, Sherine EM, Sujith RS, Dayanidhi K, Vikram JS, D’Souza F, et al. Sperm chromatin immaturity observed in short abstinence ejaculates affects DNA integrity and longevity in vitro. Plos One. 2016.
Gill K, Rosiak A, Gaczarzewicz D, Jakubik J, Kurzawa R, Kazienko A, et al. The effect of human sperm chromatin maturity on ICSI outcomes. Hum Cell. 2018;31(3):220–31.
Björndahl L, Kvist U. Human sperm chromatin stabilization: a proposed model including zinc bridges. Mol Hum Reprod. 2010;16(1):23–9.
Falcone T, Hurd WT, editors. Clinical reproductive medicine and surgery: a practical guide. New York: Springer Sciences; 2013. p. 31–42.
Rivera-Montes AM, Rivera-Gallegos A, Rodríguez-Villasana E, Juárez-Bengoa A, Díaz-Pérez Mde L, Hernández-Valencia M. Estimate of the variability in the evaluation of semen analysis. Ginecol Obstet Mex. 2013;81(11):639–44.
Turner TT. On the epididymis and its role in the development of the fertile ejaculate. J Androl. 1995;16(4):292–8 Review.
Sullivan R, Mieusset R. The human epididymis: its function in sperm maturation. Hum Reprod Update. 2016;22(5):574–87.
Tur-Kaspa I, Maor Y, Levran D, Yonish M, Mashiach S, Dor J. How often should infertile men have intercourse to achieve conception? Fertil Steril. 1994;62(2):370–5.
du Plessis SS, McAllister DA, Luu A, Savia J, Agarwal A, Lampiao F. Effects of H(2)O(2) exposure on human sperm motility parameters, reactive oxygen species levels and nitric oxide levels. Andrologia. 2010;42(3):206–10.
Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, Aitken RJ. DNA integrity in human spermatozoa: relationships with semen quality. J Androl. 2000;21(1):33–44.
Rousseaux S, Caron C, Govin J, Lestrat C, Faure AK, Khochbin S. Establishment of male-specific epigenetic information. Gene. 2005;345(2):139–53.
Rodenhiser D, Mann M. Epigenetics and human disease: translating basic biology into clinical applications. CMAJ. 2006;174(3):341–8.
Jenkins TG, Carrell DT. The sperm epigenome and potential implications for the developing embryo. Reproduction. 2012;143(6):727–34.
Marchetti F, Lowe X, Bishop J, Wyrobek AJ. Absence of selection against aneuploid mouse sperm at fertilization. Biol Reprod. 1999;61(4):948–54.
Curley JP, Mashoodh R, Champagne FA. Epigenetics and the origins of paternal effects. Horm Behav. 2011;59(3):306–14.
Denomme MM, McCallie BR, Parks JC, Booher K, Schoolcraft WB, Katz-Jaffe MG. Inheritance of epigenetic dysregulation from male factor infertility has a direct impact on reproductive potential. Fertil Steril. 2018;110(3):419–428.e1.
Hammoud SS, Nix DA, Hammoud AO, Gibson M, Cairns BR, Carrell DT. Genome-wide analysis identifies changes in histone retention and epigenetic modifications at developmental and imprinted gene loci in the sperm of infertile men. Hum Reprod. 2011;26(9):2558–69.
Tüttelmann F, Ruckert C, Röpke A. Disorders of spermatogenesis: perspectives for novel genetic diagnostics after 20 years of unchanged routine. Med Genet. 2018;30(1):12–20.
Kosova G, Scott NM, Niederberger C, Prins GS, Ober C. Genome-wide association study identifies candidate genes for male fertility traits in humans. Am J Hum Genet. 2012;90(6):950–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scarselli, F., Cursio, E., Muzzì, S. et al. How 1 h of abstinence improves sperm quality and increases embryo euploidy rate after PGT-A: a study on 106 sibling biopsied blastocysts. J Assist Reprod Genet 36, 1591–1597 (2019). https://doi.org/10.1007/s10815-019-01533-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01533-7