Abstract
Purpose
To evaluate the risk of prematurity and infant mortality by maternal fertility status, and for in vitro fertilization (IVF) pregnancies, by oocyte source and embryo state combinations.
Methods
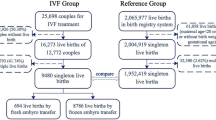
Women in 14 States who had IVF-conceived live births during 2004–13 were linked to their infant’s birth and death certificates; a 10:1 sample of non-IVF births was selected for comparison; those with an indication of infertility treatment on the birth certificate were categorized as subfertile, all others were categorized as fertile. Risks were modeled separately for the fertile/subfertile/IVF (autologous-fresh only) group and for the IVF group by oocyte source-embryo state combinations, using logistic regression, and reported as adjusted odds ratios (AORs) and 95% confidence intervals (CI).
Results
The study population included 2,474,195 pregnancies. Placental complications (placenta previa, abruptio placenta, and other excessive bleeding) and prematurity were both increased with pregestational and gestational diabetes and hypertension, among subfertile and IVF groups, and in IVF pregnancies using donor oocytes. Both subfertile and IVF pregnancies were at risk for prematurity and NICU admission; IVF infants were also at risk for small-for-gestation birthweight, and subfertile infants had greater risks for neonatal and infant death. Within the IVF group, pregnancies with donor oocytes and/or thawed embryos were at greater risk of large-for-gestation birthweight, and pregnancies with thawed embryos were at greater risk of neonatal and infant death.
Conclusions
Prematurity was associated with placental complications, diabetes and hypertension, subfertility and IVF groups, and in IVF pregnancies, donor oocytes and/or thawed embryos.

Similar content being viewed by others
References
Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM. Births: final data for 2000. Natl Vital Stat Rep. 2002;50(5):1–102.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1–70.
Toner J, Coddington CC, Doody K, van Voorhis B, Seifer D, Ball GD, Luke B, Wantman E. SART & ART in the US: a 2016 update. Fertil Steril 2016 Sep 1; 106 (3):541–546.
Center for Disease Control and Prevention, American Society for Reproductive Medicine, and Society for Assisted Reproductive Technology. 2015 Assisted reproductive technology success rates: national summary report. Atlanta (GA): US Dept. of Health and Human Services; 2017.
Basso O, Olsen J. Subfecundity and neonatal mortality: longitudinal study within the Danish National Birth Cohort. BMJ. 2005;330:393–4.
Helmerhorst FM, Perquin DAM, Donker D, Keirse JNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261–6.
Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004;103:551–63.
McDonald SD, Han Z, Mulla S, Murphy KE, Beyene J, Ohlsson A, et al. Preterm birth and low birth weight among in vitro fertilization singletons: a systematic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol. 2009;146:138–48.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren K-G, Olausson PO. Trends in delivery and neonatal outcome after in vitro fertilization in Sweden: data for 25 years. Hum Reprod. 2010;25:1026–34.
Yang X, Li Y, Li C, Zhang W. Current overview of pregnancy complications and live-birth outcome of assisted reproductive technology in mainland China. Fertil Steril. 2014;101:385–91.
Zhu JL, Obel C, Bech BH, Olsen J, Basso O. Infertility, infertility treatment, and fetal growth restriction. Obstet Gynecol. 2007;110:1326–34.
Raatikainen K, Kuivasaari-Pirinen P, Hippeläinen M, Heinonen S. Comparison of the pregnancy outcomes of subfertile women after infertility treatment and in naturally conceived pregnancies. Hum Reprod. 2012;27:1162–9.
Edwards RG, Ludwig M. Are major defects in children conceived in vitro due to innate problems in patients or to induced genetic damage? Reprod BioMed Online. 2003;7:131–8.
Buck Louis GM, Schisterman EF, Dukic VM, Schieve LA. Research hurdles complicating the analysis of infertility treatment and child health. Hum Reprod. 2005;20:12–8.
Buckett WM, Tan SL. Congenital abnormalities in children born after assisted reproductive techniques: how much is associated with the presence of infertility and how much with its treatment? Fertil Steril. 2005;84:1318–9.
Sutcliffe AG, Ludwig M. Outcome of assisted reproduction. Lancet. 2007;370:351–9.
Kondapalli LA, Perales-Puchalt A. Low birth weight: is it related to assisted reproductive technology or underlying infertility? Fertil Steril. 2013;99:303–10.
Parrish KM, Holt VL, Connell FA, Williams B, LoGerfo JP. Variations in the accuracy of obstetric procedures and diagnoses on birth records in Washington State, 1989. Am J Epidemiol. 1993;138:119–27.
Buescher PA, Taylor KP, Davis MH, Bowling JM. The quality of the new birth certificate data: a validation study in North Carolina. Am J Public Health. 1993;83:1163–5.
Piper JM, Mitchel EF, Snowden M, Hall C, Adams M, Taylor P. Validation of 1989 Tennessee birth certificate using maternal and newborn hospital records. Am J Epidemiol. 1993;137:758–68.
Woolbright LA, Harshberger DS. The revised standard certificate of live birth: analysis of medical risk factor data from birth certificates in Alabama, 1988-92. Public Health Rep. 1995;110:59–63.
Clark K, Chun-Mei F, Burnett C. Accuracy of birth certificate data regarding the amount, timing, and adequacy of prenatal care using prenatal medical records as referents. Am J Epidemiol. 1997;145:68–71.
Dobie SA, Baldwin L-M, Rosenblatt RA, Fordyce MA, Andrilla CH, Hart LG. How well do birth certificates describe the pregnancies they report? The Washington State experience with low-risk pregnancies. Matern Child Health J. 1998;2:145–54.
Reichman NE, Hade EM. Validation of birth certificate data: a study of women in New Jersey’s healthy start program. Ann Epidemiol. 2001;11:186–93.
Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health. 2003;28:335–46.
Dietz P, Bombard J, Mulready-Ward C, Gauthier J, Sackoff J, Brozicevic P, et al. Validation of selected items on the 2003 US Standard Certificate of Live Birth: New York City and Vermont. Public Health Rep. 2015;130:60–70.
Martin JA, Wilson EC, Osterman MJK, Saadi EW, Sutton SR, Hamilton BE. Assessing the quality of medical and health data from the 2003 birth certificate revision: results from two states. Natl Vital Stat Rep. 2013;62(2):1–20.
Heron M. Deaths: leading causes for 2016. Natl Vital Stat Rep. 2018;67(6):1–77.
Talge NM, Mudd LM, Sikorskii A, Basso O. United States birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133:844–53.
Land JA. How should we report on perinatal outcome? Hum Reprod. 2006;21:2638–9.
Luke B, Gopal D, Cabral H, Stern JE, Diop H. Pregnancy, birth, and infant outcomes by maternal fertility status: the Massachusetts Outcomes Study of Assisted Reproductive Technology. Am J Obstet Gynecol. 2017;217:327.e1–14.
Luke B, Gopal D, Cabral H, Stern JE, Diop H. Adverse pregnancy, birth, and infant outcomes in twins: effects of maternal fertility status and infant gender combinations; the Massachusetts Outcomes Study of Assisted Reproductive Technology. Am J Obstet Gynecol. 2017;217:330.e1–15.
Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP, et al. Diabetes trends among delivery hospitalizations in the US, 1994-2004. Diabetes Care. 2010;33:768–73.
Bateman BT, Shaw KM, Kuklina EV, Callaghan WM, Seely EW. Hypertension in women of reproductive age in the United States: NHANES 1999-2008. PLoS One. 2012;7:e36171. https://doi.org/10.1371/journal.pone.0036171.
Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113:1299–306.
Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and outcomes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206:134.e1–8.
Berg CJ, MacKay AP, Qin C, Callaghan WM. Overview of maternal morbidity during hospitalization for labor and delivery in the United States, 1993–1997 and 2001–2005. Obstet Gynecol 2009; 113:1075–1081.
Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol. 2010;116:1302–9.
Kuklina EV, Callaghan WM. Chronic heart disease and severe maternal morbidity among hospitalizations for pregnancy in the USA: 1995-2006. Br J Obstet Gynecol. 2011;118:345–52.
Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125:5–12.
Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjærven R, Vatten LJ. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum Reprod 2006; 21:2353–2358.
Luke B, Stern JE, Kotelchuck M, Declercq E, Cohen B, Diop H. Birth outcomes by infertility diagnosis: analyses of the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). J Reprod Med. 2015;60:480–90.
Luke B, Stern JE, Hornstein MD, Kotelchuck M, Diop H, Cabral H, et al. Is the wrong question being asked in infertility research? J Assist Reprod Genet. 2016;33(1):3–8.
Schachter M, Tovbin Y, Arieli S, Friedler S, Ron-El R, Sherman D. In vitro fertilization is a risk factor for vasa previa. Fertil Steril. 2002;78:642–3.
Sheiner E, Shoham-Vardi I, Hallak M, Hershkowitz R, Katz M, Mazor M. Placenta previa: obstetric risk factors and pregnancy outcome. J Matern Fetal Med. 2001;10:414–9.
Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: a population-based study of 634,741 pregnancies. PLoS One. 2013;8:e70380. https://doi.org/10.1371/journal.pone.0070380.
Rosenberg T, Pariente G, Serienko R, Wiznitzer A, Sheiner E. Critical analysis of risk factors and outcome of placenta previa. Arch Gynecol Obstet. 2011;284:47–51.
Joy J, Gannon C, McClure N, Cooke I. Is assisted reproduction associated with abnormal placentation? Pediatr Dev Pathol. 2012;15:306–14.
Nelissen ECM, Dumoulin JCM, Daunay A, Evers JLH, Tost J, van Montfort APA. Placentas from pregnancies conceived by IVF/ICSI have a reduced DNA methylation level at the H19 and MEST differentially methylated regions. Hum Reprod. 2013;28:1117–26.
Nakamura Y, Yaguchi C, Itoh H, Sakamoto R, Kimura T, Furuta N, et al. Morphologic characteristics of the placental basal plate in in vitro fertilization pregnancies: a possible association with the amount of bleeding in delivery. Hum Pathol. 2015;46:1171–9.
Sakian S, Louie K, Wong EC, Havelock J, Kashyap S, Rowe T, et al. Altered gene expression of H19 and IGF2 in placentas from ART pregnancies. Placenta. 2015;36:1100–5.
Catov JM, Wu CS, Olsen J, Sutton-Tyrrell K, Li J, Nohr EA. Early or recurrent preterm birth and maternal cardiovascular disease risk. Ann Epidemiol. 2010;20:604–9.
Arias F, Rodriguez L, Raayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am J Obstet Gynecol. 1993;168:585–91.
Germain A, Carvajal J, Sanchez M, Valenzuela G, Tsunekawa H, Chuaqui B. Preterm labor: placental pathology and clinical correlation. Obstet Gynecol. 1999;94:284–9.
Kato O, Kawasaki N, Bodri D, Kuroda T, Kawachiya S, Kato K, et al. Neonatal outcome and birth defects in 6,623 singletons born following minimal ovarian stimulation and vitrified versus fresh single embryo transfer. Eur J Obstet Gyencol Reprod Biol. 2012;161:46–50.
Weinerman R, Mainigi M. Why we should transfer frozen instead of fresh embryos: the translational rationale. Fertil Steril. 2014;102:10–8.
Barnhart KT. Introduction: are we ready to eliminate the transfer of fresh embryos in in vitro fertilization? Fertil Steril. 2014;102:1–2.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil Steril. 2014;102:3–9.
Shapiro BS, Daneshmand ST, De Leon L, Garner FC, Aguirre M, Hudson C. Frozen-thawed embryo transfer is associated with a significantly reduced incidence of ectopic pregnancy. Fertil Steril. 2012;98:1490–4.
Santos MA, Kuijk EW, Macklon NS. The impact of ovarian stimulation for IVF on the developing embryo. Reproduction. 2010;139:23–34.
Pinborg A, Loft A, Henningsen A-KA, Rasmussen S, Andersen AN. Infant outcome of 957 singletons born after frozen embryo replacement: the Danish National Cohort Study 1995-2006. Fertil Steril. 2010;94:1320–7.
Ishihara O, Araki R, Kuwahara A, Itakura A, Saito H, Adamson GD. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. 2014;101:128–33.
Sutcliffe AG, D’Souza SW, Cadman J, Richards B, McKinlay IA, Lieberman B. Minor congenital anomalies, major congenital malformations and development in children conceived from cryopreserved embryos. Hum Reprod. 1995;10:3332–7.
Belva F, Henriet S, Van den Abbeel E, Camus M, Devroey P, Van der Elst J, et al. Neonatal outcome of 937 children born after transfer of cryopreserved embryos obtained by ICSI and IVF and comparison with outcome data of fresh ICSI and IVF cycles. Hum Reprod. 2008;23:2227–38.
Shih W, Rushford DD, Bourne H, Garrett C, McBain JC, Healy DL, et al. Factors affecting low birthweight after assisted reproduction technology: difference between transfer of fresh and cryopreserved embryos suggests an adverse effect of oocyte collection. Hum Reprod. 2008;23:1644–53.
Murakami M, Egashira A, Murakami K, Araki Y, Kuramoto T. Perinatal outcome of twice-frozen-thawed embryo transfers: a clinical follow-up study. Fertil Steril. 2011;95:2648–50.
Wennerholm U-B, Henningsen A-KA, Romundstad LB, Bergh C, Pinborg A, Skjaerven R, et al. Perinatal outcomes of children born after frozen-thawed embryo transfer: a Nordic cohort study from the CoNARTaS group. Hum Reprod. 2013;28:2545–53.
Luke B, Brown MB, Wantman E, Stern JE, Toner J, Coddington CC. Increased risk of large-for-gestational age birthweight in singleton siblings conceived with in vitro fertilization in frozen versus fresh cycles. J Assist Reprod Genet. 2017;34:191–200.
Luke B, Brown MB, Spector LG. Validation of infertility treatment and assisted reproductive technology use on the birth certificate in eight States. (Research Letter) Am J Obstet Gynecol 2016; 215:126–7. PMID:26945609, 127.
Acknowledgements
The authors wish to thank SART and all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of their members, this research would not have been possible.
The authors also gratefully acknowledge the following State agencies for their assistance in conducting this study:
California Department of Public Health, Office of Health Information and Research
Colorado Department of Public Health and Environment
Connecticut Department of Public Health
Florida Department of Health
Illinois Department of Public Health
Massachusetts Department of Public Health
Michigan Department of Health and Human Services, Division for Vital Records and Health Statistics
New Jersey Department of Health
New York City Department of Health and Mental Hygiene, Bureau of Vital Statistics
New York State Department of Health, Bureau of Health Informatics, Vital Statistics Unit
North Carolina Department of Health
Ohio Department of Health, Bureau of Vital Statistics
Pennsylvania Department of Health, Bureau of Health Statistics and Research
Texas Department of State Health Services, Center for Health Statistics
Virginia Department of Health.
Source of funding
The project described was supported by grant R01CA151973 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health, nor any of the State Departments of Health which contributed data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Barbara Luke is a research consultant to the Society for Assisted Reproductive Technology; all other authors report no conflict of interest.
Rights and permissions
About this article
Cite this article
Luke, B., Brown, M.B., Wantman, E. et al. Risk of prematurity and infant morbidity and mortality by maternal fertility status and plurality. J Assist Reprod Genet 36, 121–138 (2019). https://doi.org/10.1007/s10815-018-1333-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1333-z