Abstract
Purpose
To analyse the impact of female characteristics on assisted reproductive technology outcome among male haematological cancer survivors.
Methods
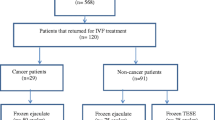
A retrospective analysis of 93 haematological cancer survivors attending our tertiary referral fertility centre between June 1998 and June 2017 for achieving fatherhood with assisted reproductive technology treatments.
Results
A progressive increase in the median female age was observed during the study period (32.2 years until the year 2007 and 36.9 years from the year 2012). Fifty-five out of 93 patients were treated with intracytoplasmic sperm injection (ICSI) (113 ovarian stimulations, 108 ICSI procedures). Cryopreserved ejaculated sperm was used in 28 couples, fresh sperm in 19, and thawed testicular sperm in 8 couples. Mean female age at ovarian stimulation was 37.0 ± 4.7 years. Twenty-six pregnancies resulted in a full-term birth (23% per started ovarian stimulation; 43.6% per couple) and 33 children were born. No significant differences were observed according to source of sperm (fresh, frozen, testicular) and multivariate analysis confirmed that maternal age was the only variable inversely related to the cumulative delivery rate, being five times lower (15.7%) when the female partner was ≥ 40 years (OR = 0.22, 95% CI 0.06–0.77) vs. 58.3% with younger women (p = 0.0037).
Conclusions
Delayed childbearing and female ageing affect ICSI outcome in couples where the male is a survivor of haematological cancer. This topic should be discussed when counselling male cancer patients about fertility preservation.

Similar content being viewed by others
References
Botchan A, Karpol S, Lehavi O, Paz G, Kleiman SE, Yogev L, et al. Preservation of sperm of cancer patients: extent of use and pregnancy outcome in a tertiary infertility center. Asian J Androl. 2013;15(3):382–6.
Hotaling JM, Lopushnyan NA, Davenport M, Christensen H, Pagel ER, Muller CH, et al. Raw and test-thaw semen parameters after cryopreservation among men with newly diagnosed cancer. Fertil Steril. 2013;99(2):464–9.
Ethics ETFo, Law. Taskforce 7: ethical considerations for the cryopreservation of gametes and reproductive tissues for self use. Hum Reprod. 2004;19(2):460–2.
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24(18):2917–31.
Daudin M, Rives N, Walschaerts M, Drouineaud V, Szerman E, Koscinski I, et al. Sperm cryopreservation in adolescents and young adults with cancer: results of the French national sperm banking network (CECOS). Fertil Steril. 2015;103(2):478–86. e1
Chan PT, Palermo GD, Veeck LL, Rosenwaks Z, Schlegel PN. Testicular sperm extraction combined with intracytoplasmic sperm injection in the treatment of men with persistent azoospermia postchemotherapy. Cancer. 2001;92(6):1632–7.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340(8810):17–8.
Babb A, Farah N, Lyons C, Lindsay K, Reddy N, Goldman J, et al. Uptake and outcome of assisted reproductive techniques in long-term survivors of SCT. Bone Marrow Transplant. 2012;47(4):568–73.
van der Kaaij MA, van Echten-Arends J, Heutte N, Meijnders P, Abeilard-Lemoisson E, Spina M, et al. Cryopreservation, semen use and the likelihood of fatherhood in male Hodgkin lymphoma survivors: an EORTC-GELA Lymphoma Group cohort study. Hum Reprod. 2014;29(3):525–33.
Ferrari S, Paffoni A, Filippi F, Busnelli A, Vegetti W, Somigliana E. Sperm cryopreservation and reproductive outcome in male cancer patients: a systematic review. Reprod BioMed Online. 2016;33(1):29–38.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction, vol. viii. 3rd ed. Cambridge: Published on behalf of the World Health Organization by Cambridge University Press; 1992. 107p p
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction, vol. x. 4th ed. Cambridge: Published on behalf of the World Health Organization by Cambridge University Press; 1999. 128p p
World Health Organization DoRHaR. WHO laboratory manual for the examination and processing of human semen. Fifth edition ed; 2010. 287 p
Ziegler WF, Chapitis J. Human motile sperm recovery after cryopreservation: freezing in nitrogen vapor vs the direct plunge technique. Prim Care Update Ob Gyns. 1998;5(4):170.
Negri L, Albani E, DiRocco M, Morreale G, Novara P, Levi-Setti PE. Testicular sperm extraction in azoospermic men submitted to bilateral orchidopexy. Hum Reprod. 2003;18(12):2534–9.
Hauser R, Botchan A, Amit A, Ben Yosef D, Gamzu R, Paz G, et al. Multiple testicular sampling in non-obstructive azoospermia--is it necessary? Hum Reprod. 1998;13(11):3081–5.
Hendriks DJ, Mol BW, Bancsi LF, Te Velde ER, Broekmans FJ. Antral follicle count in the prediction of poor ovarian response and pregnancy after in vitro fertilization: a meta-analysis and comparison with basal follicle-stimulating hormone level. Fertil Steril. 2005;83(2):291–301.
La Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Artenisio AC, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. 2010;16(2):113–30.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24.
Levi Setti PE, Albani E, Matteo M, Morenghi E, Zannoni E, Baggiani AM, et al. Five years (2004-2009) of a restrictive law-regulating ART in Italy significantly reduced delivery rate: analysis of 10,706 cycles. Hum Reprod. 2013;28(2):343–9.
Anserini P, Chiodi S, Spinelli S, Costa M, Conte N, Copello F, et al. Semen analysis following allogeneic bone marrow transplantation. Additional data for evidence-based counselling. Bone Marrow Transplant. 2002;30(7):447–51.
Magelssen H, Melve KK, Skjaerven R, Fossa SD. Parenthood probability and pregnancy outcome in patients with a cancer diagnosis during adolescence and young adulthood. Hum Reprod. 2008;23(1):178–86.
Leader A, Lishner M, Michaeli J, Revel A. Fertility considerations and preservation in haemato-oncology patients undergoing treatment. Br J Haematol. 2011;153(3):291–308.
Muller I, Oude Ophuis RJ, Broekmans FJ, Lock TM. Semen cryopreservation and usage rate for assisted reproductive technology in 898 men with cancer. Reprod BioMed Online. 2016;32(2):147–53.
Dar S, Orvieto R, Levron J, Haas J, Gat I, Raviv G. IVF outcome in azoospermic cancer survivors. Eur J Obstet Gynecol Reprod Biol. 2018;220:84–7.
Pivetta E, Maule MM, Pisani P, Zugna D, Haupt R, Jankovic M, et al. Marriage and parenthood among childhood cancer survivors: a report from the Italian AIEOP Off-Therapy Registry. Haematologica. 2011;96(5):744–51.
Gunnes MW, Lie RT, Bjorge T, Ghaderi S, Ruud E, Syse A, et al. Reproduction and marriage among male survivors of cancer in childhood, adolescence and young adulthood: a national cohort study. Br J Cancer. 2016;114(3):348–56.
ISTAT. Births and fertility among the resident population 2015 [Available from: http://www.istat.it/en/files/2016/11/EN_Births_Fertility_2015.pdf?title=Birth+and+fertility+-+28+Nov+2016+-+Full+text.pdf.
Newsrelease E. Birth and fertility, over 5 million babies born in the EU in 2015. Women first became mothers at almost 29 on average 2017 [Available from: http://ec.europa.eu/eurostat/documents/2995521/7898237/3-08032017-AP-EN.pdf/b17c1516-faad-4e65-b291-187826a7ac88.
Garcia A, Herrero MB, Holzer H, Tulandi T, Chan P. Assisted reproductive outcomes of male cancer survivors. J Cancer Surviv. 2015;9(2):208–14.
Hourvitz A, Goldschlag DE, Davis OK, Gosden LV, Palermo GD, Rosenwaks Z. Intracytoplasmic sperm injection (ICSI) using cryopreserved sperm from men with malignant neoplasm yields high pregnancy rates. Fertil Steril. 2008;90(3):557–63.
van Casteren NJ, van Santbrink EJ, van Inzen W, Romijn JC, Dohle GR. Use rate and assisted reproduction technologies outcome of cryopreserved semen from 629 cancer patients. Fertil Steril. 2008;90(6):2245–50.
Bhattacharya S, Maheshwari A, Mollison J. Factors associated with failed treatment: an analysis of 121,744 women embarking on their first IVF cycles. PLoS One. 2013;8(12):e82249.
Ragni G, Somigliana E, Restelli L, Salvi R, Arnoldi M, Paffoni A. Sperm banking and rate of assisted reproduction treatment: insights from a 15-year cryopreservation program for male cancer patients. Cancer. 2003;97(7):1624–9.
Acknowledgments
The authors thank Pasquale Patrizio, M.D., M.B.E., Yale University, Fertility Center, for helping in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Levi-Setti, P.E., Negri, L., Baggiani, A. et al. Delayed childbearing and female ageing impair assisted reproductive technology outcome in survivors of male haematological cancers. J Assist Reprod Genet 35, 2049–2056 (2018). https://doi.org/10.1007/s10815-018-1283-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1283-5