Abstract
Purpose
Few clinical options for fertility preservation are available to females with cancer, and data about clinical outcomes is limited. Potential supplementary approaches to fertility preservation include retrieval of immature oocytes followed by in vitro maturation (IVM) and storage. The aim of this study was to evaluate post-thawing outcomes of immature oocytes collected both by transvaginal aspiration and from excised ovarian tissue.
Methods
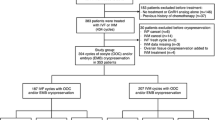
We conducted a retrospective cohort study of patients treated in a single tertiary center. We reviewed the records of 119 cancer patients who underwent ovarian tissue cryopreservation and immature oocyte harvesting for fertility preservation. All embryos and oocytes that were frozen and thawed were included in the study. Post-thawing outcomes were evaluated.
Results
Thirty-five stored embryos from eight patients were thawed. Twenty-nine embryos survived (82% survival rate) and were transferred. Six oocytes were thawed, two oocytes survived, and no oocytes were fertilized. Only one PCOS patient became pregnant, resulting in the normal delivery of a healthy baby.
Conclusions
Although a relatively high number of mature oocytes and embryos can be stored with the combined procedure, the limited rate of pregnancies represents a poor reproductive outcome. Therefore, this approach should be reserved for special groups with limited options.
Similar content being viewed by others
References
Cvancarova M, Samuelsen SO, Magelssen H, Fossa SD. Reproduction rates after cancer treatment: experience from the Norwegian radium hospital. J Clin Oncol. 2009;27(3):334–43. https://doi.org/10.1200/JCO.2007.15.3130.
Green DM, Whitton JA, Stovall M, Mertens AC, Donaldson SS, Ruymann FB, et al. Pregnancy outcome of female survivors of childhood cancer: a report from the childhood cancer survivor study. Am J Obstet Gynecol. 2002;187(4):1070–80.
Magelssen H, Melve KK, Skjaerven R, Fossa SD. Parenthood probability and pregnancy outcome in patients with a cancer diagnosis during adolescence and young adulthood. Hum Reprod. 2008;23(1):178–86. https://doi.org/10.1093/humrep/dem362.
Barton SE, Najita JS, Ginsburg ES, Leisenring WM, Stovall M, Weathers RE, et al. Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: a report from the childhood cancer survivor study cohort. Lancet Oncol. 2013;14(9):873–81. https://doi.org/10.1016/s1470-2045(13)70251-1.
Society for Assisted Reproductive Technology, 2014 Clinic summary report. 2014. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0. Accessed 14/09/2017 2017.
Practice Committees of American Society for Reproductive M, Society for Assisted Reproductive T. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99(1):37–43. https://doi.org/10.1016/j.fertnstert.2012.09.028.
Meirow D. Fertility preservation in cancer patients using stored ovarian tissue: clinical aspects. Curr Opin Endocrinol Diabetes Obes. 2008;15(6):536–47. https://doi.org/10.1097/MED.0b013e32831a44a8.
Rodriguez-Wallberg KA, Oktay K. Options on fertility preservation in female cancer patients. Cancer Treat Rev. 2012;38(5):354–61. https://doi.org/10.1016/j.ctrv.2011.10.002.
Donnez J, Jadoul P, Squifflet J, Van Langendonckt A, Donnez O, Van Eyck AS, et al. Ovarian tissue cryopreservation and transplantation in cancer patients. Best Pract Res Clin Obstet Gynaecol. 2010;24(1):87–100. https://doi.org/10.1016/j.bpobgyn.2009.09.003.
Silber S, Kagawa N, Kuwayama M, Gosden R. Duration of fertility after fresh and frozen ovary transplantation. Fertil Steril. 2010;94(6):2191–6. https://doi.org/10.1016/j.fertnstert.2009.12.073.
Donnez J, Dolmans MM, Pellicer A, Diaz-Garcia C, Sanchez Serrano M, Schmidt KT, et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil Steril. 2013;99(6):1503–13. https://doi.org/10.1016/j.fertnstert.2013.03.030.
Donnez J, Silber S, Andersen CY, Demeestere I, Piver P, Meirow D, et al. Children born after autotransplantation of cryopreserved ovarian tissue. A review of 13 live births. Ann Med. 2011;43(6):437–50. https://doi.org/10.3109/07853890.2010.546807.
Martinez F. Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Fertil Steril. 2017;108(3):407–15.e11. https://doi.org/10.1016/j.fertnstert.2017.05.024.
Meirow D, Hardan I, Dor J, Fridman E, Elizur S, Ra'anani H, et al. Searching for evidence of disease and malignant cell contamination in ovarian tissue stored from hematologic cancer patients. Hum Reprod. 2008;23(5):1007–13. https://doi.org/10.1093/humrep/den055.
Fasano G, Moffa F, Dechene J, Englert Y, Demeestere I. Vitrification of in vitro matured oocytes collected from antral follicles at the time of ovarian tissue cryopreservation. Reprod Biol Endocrinol. 2011;9:150. https://doi.org/10.1186/1477-7827-9-150.
Hourvitz A, Yerushalmi GM, Maman E, Raanani H, Elizur S, Brengauz M, et al. Combination of ovarian tissue harvesting and immature oocyte collection for fertility preservation increases preservation yield. Reprod BioMed Online. 2015;31(4):497–505. https://doi.org/10.1016/j.rbmo.2015.06.025.
Revel A, Revel-Vilk S, Aizenman E, Porat-Katz A, Safran A, Ben-Meir A, et al. At what age can human oocytes be obtained? Fertil Steril. 2009;92(2):458–63. https://doi.org/10.1016/j.fertnstert.2008.07.013.
Prasath EB, Chan ML, Wong WH, Lim CJ, Tharmalingam MD, Hendricks M, et al. First pregnancy and live birth resulting from cryopreserved embryos obtained from in vitro matured oocytes after oophorectomy in an ovarian cancer patient. Hum Reprod. 2014;29(2):276–8. https://doi.org/10.1093/humrep/det420.
Segers I, Mateizel I, Van Moer E, Smitz J, Tournaye H, Verheyen G, et al. In vitro maturation (IVM) of oocytes recovered from ovariectomy specimens in the laboratory: a promising “ex vivo” method of oocyte cryopreservation resulting in the first report of an ongoing pregnancy in Europe. J Assist Reprod Genet. 2015;32(8):1221–31. https://doi.org/10.1007/s10815-015-0528-9.
Uzelac PS, Delaney AA, Christensen GL, Bohler HC, Nakajima ST. Live birth following in vitro maturation of oocytes retrieved from extracorporeal ovarian tissue aspiration and embryo cryopreservation for 5 years. Fertil Steril. 2015;104(5):1258–60. https://doi.org/10.1016/j.fertnstert.2015.07.1148.
Meirow D, Epstein M, Lewis H, Nugent D, Gosden RG. Administration of cyclophosphamide at different stages of follicular maturation in mice: effects on reproductive performance and fetal malformations. Hum Reprod. 2001;16(4):632–7.
Meirow D, Nugent D. The effects of radiotherapy and chemotherapy on female reproduction. Hum Reprod Update. 2001;7(6):535–43.
Fadini R, Dal Canto MB, Mignini Renzini M, Brambillasca F, Comi R, Fumagalli D, et al. Effect of different gonadotrophin priming on IVM of oocytes from women with normal ovaries: a prospective randomized study. Reprod BioMed Online. 2009;19(3):343–51.
Meirow D, Levron J, Eldar-Geva T, Hardan I, Fridman E, Zalel Y, et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N Engl J Med. 2005;353(3):318–21. https://doi.org/10.1056/NEJMc055237.
Meirow D, Ra’anani H, Biderman H. Ovarian tissue cryopreservation and transplantation: a realistic, effective technology for fertility preservation. Methods Mol Biol. 2014;1154:455–73. https://doi.org/10.1007/978-1-4939-0659-8_21.
Revel A, Safran A, Benshushan A, Shushan A, Laufer N, Simon A. In vitro maturation and fertilization of oocytes from an intact ovary of a surgically treated patient with endometrial carcinoma: case report. Hum Reprod. 2004;19(7):1608–11.
Shalom-Paz E, Almog B, Shehata F, Huang J, Holzer H, Chian RC, et al. Fertility preservation for breast-cancer patients using IVM followed by oocyte or embryo vitrification. Reprod BioMed Online. 2010;21(4):566–71. https://doi.org/10.1016/j.rbmo.2010.05.003.
Yin H, Jiang H, Kristensen SG, Andersen CY. Vitrification of in vitro matured oocytes collected from surplus ovarian medulla tissue resulting from fertility preservation of ovarian cortex tissue. J Assist Reprod Genet. 2016;33(6):741–6. https://doi.org/10.1007/s10815-016-0691-7.
Walls ML, Douglas K, Ryan JP, Tan J, Hart R. In-vitro maturation and cryopreservation of oocytes at the time of oophorectomy. Gynecol Oncol Rep. 2015;13:79–81. https://doi.org/10.1016/j.gore.2015.07.007.
Sonigo C, Simon C, Boubaya M, Benoit A, Sifer C, Sermondade N, et al. What threshold values of antral follicle count and serum AMH levels should be considered for oocyte cryopreservation after in vitro maturation? Hum Reprod. 2016;31(7):1493–500. https://doi.org/10.1093/humrep/dew102.
Chung K, Donnez J, Ginsburg E, Meirow D. Emergency IVF versus ovarian tissue cryopreservation: decision making in fertility preservation for female cancer patients. Fertil Steril. 2013;99(6):1534–42. https://doi.org/10.1016/j.fertnstert.2012.11.057.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no competing interests.
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kedem, A., Yerushalmi, G., Brengauz, M. et al. Outcome of immature oocytes collection of 119 cancer patients during ovarian tissue harvesting for fertility preservation. J Assist Reprod Genet 35, 851–856 (2018). https://doi.org/10.1007/s10815-018-1153-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1153-1