Abstract
Purpose
Extensive follicle loss has been demonstrated in ovarian grafts post transplantation, reducing their productivity and lifespan. Several mechanisms for this loss have been proposed, and this study aims to clarify when and how the massive follicle loss associated with transplantation of ovarian tissue graft occurs. An understanding of the mechanisms of follicle loss will pinpoint potential new targets for optimization and improvement of this important fertility preservation technique.
Methods
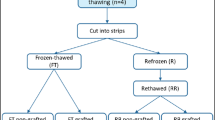
Frozen-thawed marmoset (n = 15), bovine (n = 37), and human (n = 46) ovarian cortical tissue strips were transplanted subcutaneously into immunodeficient castrated male mice for 3 or 7 days. Histological (H&E, Masson’s trichrome) analysis and immunostaining (Ki-67, GDF9, cleaved caspase-3) were conducted to assess transplantation-associated follicle dynamics, with untransplanted frozen-thawed tissue serving as a negative control.
Results
Evidence of extensive primordial follicle (PMF) activation and loss was observed already 3 days post transplantation in marmoset, bovine, and human tissue grafts, compared to frozen-thawed untransplanted controls (p < 0.001). No significant additional PMF loss was observed 7 days post transplantation. Recovered grafts of all species showed markedly higher rates of proliferative activity and progression from dormant to growing follicles (Ki-67 and GDF9 staining) as well as higher growing/primordial (GF/PMF) ratio (p < 0.02) and higher collagen levels compared with untransplanted controls.
Conclusions
This multi-species study demonstrates that follicle activation plays an important role in transplantation-induced follicle loss, and that it occurs within a very short time frame after grafting. These results underline the need to prevent this activation at the time of transplantation in order to retain the maximal possible follicle reserve and extend graft lifespan.





Similar content being viewed by others
References
Donnez J, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364(9443):1405–10.
Meirow D, et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N Engl J Med. 2005;353(3):318–21.
Meirow D, Ra’anani H, Biderman H. Ovarian tissue cryopreservation and transplantation: a realistic, effective technology for fertility preservation. Methods Mol Biol. 2014;1154:455–73.
Stoop D, Cobo A, Silber S. Fertility preservation for age-related fertility decline. Lancet. 2014;384(9950):1311–9.
Donnez J, Dolmans MM. Transplantation of ovarian tissue. Best Pract Res Clin Obstet Gynaecol. 2014;28(8):1188–97.
Andersen CY, et al. Long-term duration of function of ovarian tissue transplants: case reports. Reprod BioMed Online. 2012;25(2):128–32.
Meirow D, et al. Transplantations of frozen-thawed ovarian tissue demonstrate high reproductive performance and the need to revise restrictive criteria. Fertil Steril. 2016;106(2):467–74.
Kawamura K, et al. Ovary transplantation: to activate or not to activate. Hum Reprod. 2015;30(11):2457–60.
Silber S. Ovarian tissue cryopreservation and transplantation: scientific implications. J Assist Reprod Genet. 2016;33(12):1595–603.
McCord JM. Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med. 1985;312(3):159–63.
Van Eyck AS, et al. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in a murine model. Fertil Steril. 2010;93(5):1676–85.
Donnez J, et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil Steril. 2013;99(6):1503–13.
Donnez J, Dolmans MM. Cryopreservation and transplantation of ovarian tissue. Clin Obstet Gynecol. 2010;53(4):787–96.
Lee J, et al. Ovarian injury during cryopreservation and transplantation in mice: a comparative study between cryoinjury and ischemic injury. Hum Reprod. 2016;31(8):1827–37.
Donnez J, et al. Ovarian tissue cryopreservation and transplantation: a review. Hum Reprod Update. 2006;12(5):519–35.
Gavish Z, et al. Follicle activation and ‘burn-out’ contribute to post-transplantation follicle loss in ovarian tissue grafts: the effect of graft thickness. Hum Reprod. 2014;29(5):989–96.
Liu J, et al. Early massive follicle loss and apoptosis in heterotopically grafted newborn mouse ovaries. Hum Reprod. 2002;17(3):605–11.
Dolmans MM, et al. Short-term transplantation of isolated human ovarian follicles and cortical tissue into nude mice. Reproduction. 2007;134(2):253–62.
Hancke K, et al. Ovarian transplantation for fertility preservation in a sheep model: can follicle loss be prevented by antiapoptotic sphingosine-1-phosphate administration? Gynecol Endocrinol. 2009;25(12):839–43.
Soleimani R, Heytens E, Oktay K. Enhancement of neoangiogenesis and follicle survival by sphingosine-1-phosphate in human ovarian tissue xenotransplants. PLoS One. 2011;6(4):e19475.
Newton H, et al. Low temperature storage and grafting of human ovarian tissue. Hum Reprod. 1996;11(7):1487–91.
Roness H, et al. Ovarian follicle burnout: a universal phenomenon? Cell Cycle. 2013;12(20):3245–6.
Hearn JP, et al. Use of the common marmoset, Callithrix jacchus, in reproductive research. Primates Med. 1978;10:40–9.
Telfer EE, et al. A two-step serum-free culture system supports development of human oocytes from primordial follicles in the presence of activin. Hum Reprod. 2008;23(5):1151–8.
Meirow D, et al. Monitoring the ovaries after autotransplantation of cryopreserved ovarian tissue: endocrine studies, in vitro fertilization cycles, and live birth. Fertil Steril. 2007;87(2):418 e7–418 e15.
Kalich-Philosoph L, et al. Cyclophosphamide triggers follicle activation and “burnout”; AS101 prevents follicle loss and preserves fertility. Sci Transl Med. 2013;5(185):185ra62.
Vitt UA, et al. In vivo treatment with GDF-9 stimulates primordial and primary follicle progression and theca cell marker CYP17 in ovaries of immature rats. Endocrinology. 2000;141(10):3814–20.
Aubard Y, et al. Orthotopic and heterotopic autografts of frozen-thawed ovarian cortex in sheep. Hum Reprod. 1999;14(8):2149–54.
Nottola SA, et al. Cryopreservation and xenotransplantation of human ovarian tissue: an ultrastructural study. Fertil Steril. 2008;90(1):23–32.
Oktay K, Oktem O. Ovarian cryopreservation and transplantation for fertility preservation for medical indications: report of an ongoing experience. Fertil Steril. 2010;93(3):762–8.
Kawamura K, et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc Natl Acad Sci U S A. 2013;110(43):17474–9.
Suzuki N, et al. Successful fertility preservation following ovarian tissue vitrification in patients with primary ovarian insufficiency. Hum Reprod. 2015;30(3):608–15.
Hsueh AJ, et al. Intraovarian control of early folliculogenesis. Endocr Rev. 2015;36(1):1–24.
Meirow D, et al. Optimizing outcomes from ovarian tissue cryopreservation and transplantation; activation versus preservation. Hum Reprod. 2015;30(11):2453–6.
Visser JA, et al. Anti-Müllerian hormone: a new marker for ovarian function. Reproduction. 2006;131(1):1–9.
Acknowledgements
The authors wish to thank Mrs. Sanaz Dereh-Haim, Mrs. Reinhild Sandhowe-Klawerkamp, and Mr. Martin Heuermann for excellent technical assistance and animal care. The following foundations contributed to the funding of this study: Israel Science Foundation and Kahn Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were conducted according to the German Law on the Care and Use of Laboratory Animals under license 84-02.05.20.12.0.018.
Rights and permissions
About this article
Cite this article
Gavish, Z., Spector, I., Peer, G. et al. Follicle activation is a significant and immediate cause of follicle loss after ovarian tissue transplantation. J Assist Reprod Genet 35, 61–69 (2018). https://doi.org/10.1007/s10815-017-1079-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-1079-z