Abstract
Purpose
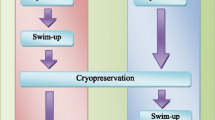
The aim of this study is to evaluate which cryopreservation protocol, freezing before or after swim-up, optimizes cryopreservation outcomes in terms of motile sperm count, motility, morphology, and viability, and also to establish whether sperm viability could be assessed based on sperm motility.
Methods
Fifty-three fresh and 53 swim-up prepared samples were considered for the first experiment. In parallel, total motility evaluation by CASA system (computer-assisted sperm analyzer) and hypoosmotic swelling test (HOS-test) was performed in each sample to compare the viability results of both methods. In the second experiment, 21 normozoospermic semen samples and 20 semen samples from male factor patients were included. After fresh ejaculate evaluation, the semen sample of each patient was divided into two aliquots, one of them was frozen before swim-up and the other was frozen after swim-up. Motility, sperm count, morphology, and viability were evaluated after thawing.
Results
A linear regression model allows prediction of HOS-test viability results based on total motility: HOS = 1.38 + 0.97 · TM (R 2 = 99.10, residual mean squares = 9.51). Freezing before sperm selection leads to higher total and progressive motility, total motile sperm count, and viability rates than when sperm selection is performed before freezing (P < 0.005 in all cases). In fact, sperm selection prior to freezing reaches critical values when subfertile patients are considered.
Conclusions
To conclude, total motility evaluation can predict HOS-test viability results, resulting in a more objective and less time-consuming method to assess viability. In addition, sperm freezing prior to swim-up selection must be considered in order to achieve better outcomes after thawing, especially in patients presenting poor sperm baseline.


Similar content being viewed by others
References
Hammadeh ME, Dehn C, Hippach M, Zeginiadou T, Stieber M, Georg T, et al. Comparison between computerized slow-stage and static liquid nitrogen vapour freezing methods with respect to the deleterious effect on chromatin and morphology of spermatozoa from fertile and subfertile men. Int J Androl. 2001;24:66–72.
Zhu WJ, Liu XG. Cryodamage to plasma membrane integrity in head and tail regions of human sperm. Asian J Androl China. 2000;2:135–8.
Hossain A, Osuamkpe C, Hossain S, Phelps JY. Spontaneously developed tail swellings (SDTS) influence the accuracy of the hypo-osmotic swelling test (HOS-test) in determining membrane integrity and viability of human spermatozoa. J Assist Reprod Genet. 2010;27:83–6.
Lin MH, Morshedi M, Srisombut C, Nassar A, Oehninger S. Plasma membrane integrity of cryopreserved human sperm: an investigation of the results of the hypoosmotic swelling test, the water test, and eosin-Y staining. Fertil Steril. 1998;70:1148–55.
O’Connell M, McClure N, Lewis SEM. The effects of cryopreservation on sperm morphology, motility and mitochondrial function. Hum Reprod. 2002;17:704–9.
Satirapod C, Treetampinich C, Weerakiet S, Wongkularb A, Rattanasiri S, Choktanasiri W. Comparison of cryopreserved human sperm from solid surface vitrification and standard vapor freezing method: on motility, morphology, vitality and DNA integrity. Andrologia. 2012;44(Suppl 1):786–90.
Oberoi B, Kumar S, Talwar P. Study of human sperm motility post cryopreservation. Med J Armed Forces India. 2014;70:349–53.
Agha-Rahimi A, Khalili MA, Nabi A, Ashourzadeh S. Vitrification is not superior to rapid freezing of normozoospermic spermatozoa: effects on sperm parameters, DNA fragmentation and hyaluronan binding. Reprod BioMed Online. 2014;28:352–8.
Ozkavukcu S, Erdemli E, Isik A, Oztuna D, Karahuseyinoglu S. Effects of cryopreservation on sperm parameters and ultrastructural morphology of human spermatozoa. J Assist Reprod Genet. 2008;25:403–11.
Kopeika J, Thornhill A, Khalaf Y. The effect of cryopreservation on the genome of gametes and embryos: principles of cryobiology and critical appraisal of the evidence. Hum Reprod Update. 2015;21:209–27.
Thomson LK, Fleming SD, Aitken RJ, De Iuliis GN, Zieschang JA, Clark AM. Cryopreservation-induced human sperm DNA damage is predominantly mediated by oxidative stress rather than apoptosis. Hum Reprod. 2009;24:2061–70.
Ribas-Maynou J, Fernández-Encinas a., García-Peiró a., Prada E, Abad C, Amengual MJ, et al. Human semen cryopreservation: a sperm DNA fragmentation study with alkaline and neutral comet assay. Andrology 2014;2:83–87.
Michaeli M, Peer S, Anderman S, Ballas S, Ellenbogen A. Post swim-up versus original sperm quality, and strict criteria morphology, it’s influence on fertilization rate in in vitro fertilization program: a pilot study. Int Congr Ser. 2004;1271:181–4.
Ricci G, Perticarari S, Boscolo R, Montico M, Guaschino S, Presani G. Semen preparation methods and sperm apoptosis: swim-up versus gradient-density centrifugation technique. Fertil Steril. 2009;91:632–8.
Fácio CL, Previato LF, Machado-Paula LA, Matheus PCS, Araújo FE. Comparison of two sperm processing techniques for low complexity assisted fertilization: sperm washing followed by swim-up and discontinuous density gradient centrifugation. J Bras Reprod Assist. 2016;20:206–11.
Martínez-Soto JC, Landeras J, Gadea J. Spermatozoa and seminal plasma fatty acids as predictors of cryopreservation success. Andrology. 2013;1:365–75.
Patel M, Gandotra VK, Cheema RS, Bansal AK, Kumar A. Seminal plasma heparin binding proteins improve semen quality by reducing oxidative stress during cryopreservation of cattle bull semen. Asian-Australasian J Anim Sci. 2016;29:1247–55.
Barrios B, Pérez-Pé R, Muiño-Blanco T, Cebrián-Pérez JA. Seminal plasma proteins revert the cold-shock damage on ram sperm membrane. Int J Androl. 2001;24:352–9.
Hotaling J, Patel D, Vendryes C. Predictors of sperm recovery after cryopreservation in testicular cancer. Asian J. 2016:35–8.
Hamilton JAM, Cissen M, Brandes M, JMJ S, De Bruin JP, Kremer JAM, et al. Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Hum Reprod. 2014;30:1110–21.
Borges E, Setti AS, Braga DPAF, RCS F, Iaconelli A. Total motile sperm count has a superior predictive value over the WHO 2010 cut-off values for the outcomes of intracytoplasmic sperm injection cycles. Andrology. 2016;4:880–6.
Montagut M, Gatimel N, Bourdet-Loub??re S, Daudin M, Bujan L, Mieusset R, et al. Sperm freezing to address the risk of azoospermia on the day of ICSI. Hum Reprod 2015;30:2486–2492.
Caponecchia L, Cimino G, Sacchetto R, Fiori C, Sebastianelli A, Salacone P, et al. Do malignant diseases affect semen quality? Sperm parameters of men with cancers. Andrologia Wiley Online Library. 2016;48:333–40.
Auger J, Sermondade N, Eustache F. Semen quality of 4480 young cancer and systemic disease patients: baseline data and clinical considerations. Basic Clin Androl. 2016;26:3.
Daudin M, Rives N, Walschaerts M, Drouineaud V, Szerman E, Koscinski I, et al. Sperm cryopreservation in adolescents and young adults with cancer: results of the French national sperm banking network (CECOS). Fertil Steril. 2015;103:478–486.e1.
Agarwal A, Allamaneni SSR. Disruption of spermatogenesis by the cancer disease process. J Natl Cancer Inst Monogr. 2005;44195:9–12.
Martini AC, Molina RI, Estofán D, Tissera A, Ruiz RD, de Cuneo MF. Improving the predictive value of the hypoosmotic swelling test in humans. Fertil Steril. 2016;85:1840–2.
Nallella KP, Sharma RK, Allamaneni SSR, Aziz N, Agarwal A. Cryopreservation of human spermatozoa: comparison of two cryopreservation methods and three cryoprotectants. Fertil Steril. 2004;82:913–8.
Donnelly ET, McClure N, Lewis SEM. Cryopreservation of human semen and prepared sperm: effects on motility parameters and DNA integrity. Fertil Steril. 2001;76:892–900.
Petyim S, Neungton C, Thanaboonyawat I, Laokirkkiat P, Choavaratana R. Sperm preparation before freezing improves sperm motility and reduces apoptosis in post-freezing-thawing sperm compared with post-thawing sperm preparation. J Assist Reprod Genet. 2014;31:1673–80.
Esteves SC, Sharma RK, Thomas AJ, Agarwal A. Improvement in motion characteristics and acrosome status in cryopreserved human spermatozoa by swim-up processing before freezing. Hum Reprod. 2000;15:2173–9.
Brugnon F, Ouchchane L, Pons-Rejraji H, Artonne C, Farigoule M, Janny L. Density gradient centrifugation prior to cryopreservation and hypotaurine supplementation improve post-thaw quality of sperm from infertile men with oligoasthenoteratozoospermia. Hum Reprod. 2013;28:2045–57.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Hospital La Fe Research Foundation (Instituto de Investigación Sanitaria La Fe) research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Palomar Rios, A., Gascón, A., Martínez, J.V. et al. Sperm preparation after freezing improves motile sperm count, motility, and viability in frozen-thawed sperm compared with sperm preparation before freezing-thawing process. J Assist Reprod Genet 35, 237–245 (2018). https://doi.org/10.1007/s10815-017-1050-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-1050-z