Abstract
Objective
Intracytoplasmic sperm injection (ICSI) is commonly used during pre-implantation genetic diagnosis (PGD) in vitro fertilization (IVF), aiming to eliminate the risk of contamination from extraneous sperm DNA. Recently, ICSI “overuse” in non-male infertility has been doubted, since it does not offer an advantage over IVF. Prompted by the aforementioned observations, we sought to assess the accuracy of IVF vs ICSI in PGD cases, as might be reflected by a difference in the prevalence of discarded embryos as a consequent of parental contamination.
Methods
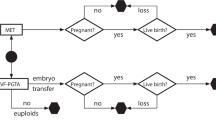
Cohort-historical study of all consecutive patients admitted to the IVF-PGD program in a large tertiary center. The percentages of complete, incomplete diagnosis, PCR failure, abnormal embryos, and the contamination rate with paternal DNA in the IVF-only and the ICSI-only groups. We reviewed the computerized files of all consecutive women admitted to our IVF for a PGD-PCR cycle. Patients were divided accordingly into three groups: an IVF group—where all the oocytes underwent IVF only, an ICSI group—where all oocytes underwent ICSI, and a mixed group—where sibling oocytes underwent both IVF and ICSI. The laboratory data and the genetic diagnostic results were collected and compared between the different insemination groups.
Results
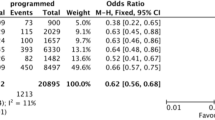
Nine-hundred and twenty-seven patients underwent IVF-PGD cycles in our program, 315 in the IVF group, 565 in the ICSI group, and 47 in the mixed group. No differences were observed in fertilization rates, the percentage of embryos available for biopsy, and the percentages of complete, incomplete diagnosis, PCR failure, or abnormal embryos, between the IVF-only and the ICSI-only groups and between the IVF and the ICSI of sibling oocytes in the mixed group. Moreover, contamination with paternal DNA, through contamination with sperm cells, was negligible. Not one single case of misdiagnosis was encountered during the study period.
Conclusion
It might be therefore concluded that IVF should be the preferred insemination methods in PGD cycles, and ICSI should be indicated only in cases of male-factor infertility.
Similar content being viewed by others
References
Harton GL, Magli MC, Lundin K, Montag M, Lemmen J, ESHRE PGD, et al. Consortium/embryology special interest group-best practice guidelines for polar body and embryo biopsy for preimplantation genetic diagnosis/screening (PGD/PGS). Hum Reprod. 2011;26:41–6.
Berger VK, Baker VL. Preimplantation diagnosis for single gene disorders. Semin Reprod Med. 2014;32:107–13.
De Rycke M, Belva F, Goossens V, Moutou C, SenGupta SB, ESHRE PGD, et al. Consortium data collection XIII: cycles from January to December 2010 with pregnancy follow-up to October 2011. Hum Reprod. 2015;30:1763–89.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic sperm injection of single spermatozoon into the oocyte. Lancet. 1992;340:17–8.
Evers JLH. Santa Claus in the fertility clinic. Hum Reprod. 2016;31:1381–2.
Bhattacharya S, Hamilton MP, Shaaban M, Kalaf Y, Seddler M, Ghobara T, et al. Conventional in-vitro fertilization versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet. 2001;357:2075–9.
Tannus S, Son WY, Gilman A, Younes G, Shavit T, Dahan MH. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod. 2017;32:119–24.
ASRM, the practice committees of the American Society for Reproductive Medicine and Society for Assisted Reproductive Technology. Intracytoplasmic sperm injection (ICSI) for non-male factor infertility: a committee opinion. Fertil Steril. 2012;98:1395–9.
Orvieto R, Brengauz M, Feldman BA. Novel approach to normal responder patient with repeated implantation failures—a case report. Gynecol Endocrinol. 2015;31:435–7.
World Health Organization. WHO Laboratory manual for the examination and processing of human semen. 5th ed. Geneva: WHO Press; 2010.
Dotan K, Feldman B, Goldman B, Peri Y, Peleg L. The single cell as a tool for genetic testing: credibility, precision, implication. J Assist Reprod Genet. 2010;27(6):335–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Feldman, B., Aizer, A., Brengauz, M. et al. Pre-implantation genetic diagnosis—should we use ICSI for all?. J Assist Reprod Genet 34, 1179–1183 (2017). https://doi.org/10.1007/s10815-017-0966-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-0966-7