Abstract
Purpose
The purpose of this study was to investigate the chromosomal constitution and the developmental potential of intracytoplasmic sperm injection (ICSI) deriving embryos displaying a single pronucleus at the zygote stage.
Methods
Eighty-eight embryos from single pronucleus (1PN) two polar bodies (2PB) ICSI zygotes from 64 preimplantational genetic screening (PGS) cycles (October 2012–December 2014), were retrospectively analyzed. Zygotes were cultured in a time-lapse incubator. Embryo biopsy was performed on day 3 and genetic analysis approached by array comparative genomic hybridization.
Results
Chromosomal analysis revealed that 17% (15/88) of embryos derived from 1PN 2PB zygotes were diagnosed as euploid. After blastomere biopsy at day 3, the blastocyst rate at day 5 was 3.4% (3/88). Only 2.3% (2/88) euploid blastocysts were obtained. In two couples and after counseling and patient agreement, the transfer of a euploid blastocyst from a 1PN 2PB ICSI zygote was performed resulting in the birth of a healthy child.
Conclusions
These results open the possibility to consider embryos coming from 1PN 2PB ICSI zygotes for transfer when no other embryos from 2PN 2PB ICSI zygotes are available and if a PGS diagnosis of euploidy is obtained. Confirmation of biparental inheritance is strongly recommended.


Similar content being viewed by others
References
Yang Z, Liu J, Collins GS, Salem SA, Liu X, Lyle SS, Peck AC, Sills ES, Salem RD. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5:24.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, Treff NR, Scott RT. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100:100–7.
Harton GL, Munné S, Surrey M, Grifo J, Kaplan B, McCulloh DH, Griffin D, Wells D. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100:1695–703.
Rubio C, Buendia P, Rodrigo L, Mercader A, Mateu E, Peinado V, Delgado A, Milan M, Mir P, Simon C, et al. Prognostic factors for preimplantation genetic screening in repeated pregnancy loss. Reprod BioMed Online. 2009;18:687–93.
Rodrigo L, Peinado V, Mateu E, Remohí J, Pellicer A, Simón C, Gil-Salom M, Rubio C. Impact of diferent paterns of sperm chromosomal abnormalities on the chromosomal constitution of preimplantation embryos. Fertil Steril. 2010;94:1380–6.
Lemmen JG, Agerholm I, Ziebe S. Kinetic markers of human embryo quality using time-lapse recordings of IVF/ICSI-fertilized oocytes. Reprod BioMed Online. 2008;17:385–91.
Meseguer M, Herrero J, Tejera A, Hilligsøe KM, Ramsing NB, Remoh J. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011;26:2658–71.
Basile N, Vime P, Florensa M, Aparicio Ruiz B, Garcia Velasco JA, Remohi J, Meseguer M. The use of morphokinetics as a predictor of implantation: a multicentric study to define and validate an algorithm for embryo selection. Hum Reprod. 2015;30:276–83.
Castello D, Motato Y, Basile N, Remohi J, Espejo-Catena M, Meseguer M. How much have we learned from time-lapse in clinical IVF? Mol Hum Rep. 2016;22:719–27.
Yang Z, Zhang J, Salem SA, Liu X, Kuang Y, Salem RD, Liu J. Selection of competent blastocysts for transfer by combining time-lapse monitoring and array CGH testing for patients undergoing preimplantation genetic screening: a prospective study with sibling oocytes. BMC Med Genet. 2014;7:38. doi:10.1186/1755-8794-7-38.
Staessen C, Janssenswillen C, Devroey P, Van Steirteghem AC. Cytogenetic and morphological observations of single pronucleated human oocytes after in-vitro fertilization. Hum Reprod. 1993;8:221–3.
Munné S, Tang Y, Grifo J, Cohen J. Origin of single pronucleated human zygotes. J Assist Reprod Genet. 1993;10(4):276–9.
Mateo S, Parriego M, Boada M, Vidal F, Coroleu B, Veiga A. In vitro development and chromosome constitution of embryos derived from monopronucleated zygotes after intracytoplasmic sperm injection. Fertil Steril. 2013;99:897–902.
Azevedo AR, Pinho MJ, Silva J, Sa R, Thorsteinsdottir S, Barros A, Sousa M. Molecular cytogenetics of human single pronucleated zygotes. Reprod Sci. 2014;21:1472–82.
Rosenbusch B. The chromosomal constitution of embryos arising from monopronuclear oocytes in Programmes of assisted reproduction. Int J Reprod Med. 2014:1–8.
Johnson DS, Cinnioglu C, Ross R, Filby A, Gemelos G, Hill M, Ryan A, Smotrich D, Rabinowitz M, Murray MJ. Comprehensive analysis of karyotypic mosaicism between trophectoderm and inner cell mass. Mol Hum Reprod. 2010;16:944–9.
Staessen C, Van Steirteghem AC. The chromosomal constitution of embryos developing from abnormally fertilized oocytes after intracytoplasmic sperm injection and conventional in-vitro fertilization. Hum Reprod. 1997;12:321–7.
Barak Y, Kogosowski A, Goldman S, Soffer Y, Gonen Y, Tesarik J. Pregnancy and birth after transfer of embryos that developed from single-nucleated zygotes obtained by injection of round spermatids into oocytes. Fertil Steril. 1998;70:67–70.
Boada M, Gil Y, Mateo S, Joda L, Barri PN, Veiga A. Morphokinetic differences on embryo development after normal or abnormal fertilization. Fert and Ster. 2012;98(3):S159–60.
Van der Heijen GW, Van der Berg IM, Baart EB, Derijck AAHA, Martini E, De Boer P. Parental origin of chromatin in human monopronuclear zygotes revealed by asymmetric histone methylation patterns, differs between IVF and ICSI. Mol Reprod Dev. 2009;76:101–8.
Gras L, Trounson AO. Pregnancy and birth resulting from transfer of a blastocyst observed to have one pronucleus at the time of examination for fertilization. Hum Reprod. 1999;14:1869–71.
Liao H, Zhang S, Cheng D, Ouyang Q, Lin G, Gu Y, Lu C, Gong F, Lu G. Cytogenetic analysis of human embryos and embryonic stem cells derived from monopronuclear zygotes. J Assist Reprod Genet. 2009;26:583–9.
Lim AST, Goh VHH, Su CL, Yu SL. Microscopic assessment of pronuclear embryos is not definitive. Hum Genet. 2000;107:62–8.
Munné S. Chromosome abnormalities and their relationship to morphology and development of human embryos. Reprod BioMed Online. 2006;12:234–53.
Magli MC, Gianaroli L, Ferraretti AP, Lappi M, Ruberti A, Farfalli V. Embryo morphology and development are dependent on the chromosomal complement. Fertil Steril. 2007;87:534–41.
Fragouli E, Alfarawati S, Daphnis DD, Goodall NN, Mania A, Griffiths T, Gordon A, Wells D. Cytogenetic analysis of human blastocysts with the use of FISH, CGH and aCGH: scientific data and technical evaluation. Hum Reprod. 2011;26:480–90.
Mertzanidou A, Wilton L, Cheng J, Spits C, Vanneste E, Moreau Y, Vermeesch JR, Sermon K. Microarray analysis reveals abnormal chromosomal complements in over 70% of 14 normally developing human embryos. Hum Reprod. 2013;28:256–64.
Gutiérrez-Mateo C, Colls P, Sánchez-García J, Escudero T, Prates R, Ketterson K, Wells D, Munné S. Validation of microarray comparative genomic hybridization for comprehensive chromosome analysis of embryos. Fertil Steril. 2011;95:953–8.
Itoi F, Asano Y, Shimizu M, Honnma H, Murata Y. Birth of nine normal healthy babies following transfer of blastocysts derived from human single-pronucleate zygotes. J Assist Reprod Genet. 2015;32:1401–7.
Otsu E, Sato A, Nagaki M, Araki Y, Utsunomiya T. Developmental potential and chromosomal constitution of embryos derived from larger single pronuclei of human zygotes used in in vitro fertilization. Fertil Steril. 2004;81:723–4.
Dasig D, Lyon J, Behr B, Milki A. Monozygotic twin birth after the transfer of a cleavage stage embryo resulting from a single pronucleated oocyte. J Assist Reprod Genet. 2004;21:427–9.
Yin BL, Hao HY, Zhang YN, Wei D, Zhang CL. Good quality blastocyst from non-/mono-pronuclear zygote may be used for transfer during IVF. Syst Biol Reprod Med. 2016;62:139–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The project was approved by the institutional review board of the center.
Funding
This work was performed under the auspices of “Càtedra d’Investigació en Obstetrícia i Ginecologia” of the Department of Obstetrics, Gynecology and Reproduction, Dexeus Women’s Health (Barcelona).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Video 1
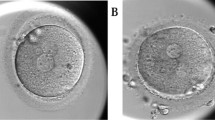
In vitro development until day 3 of 1PN 2PB ICSI zygote that produced an ongoing pregnancy and the delivery of a healthy child (AVI 313780 kb)
Rights and permissions
About this article
Cite this article
Mateo, S., Vidal, F., Parriego, M. et al. Could monopronucleated ICSI zygotes be considered for transfer? Analysis through time-lapse monitoring and PGS. J Assist Reprod Genet 34, 905–911 (2017). https://doi.org/10.1007/s10815-017-0937-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-0937-z