Abstract
Purpose
The aim of this study was to identify factors associated with double embryo implantation following double embryo transfer (DET) during assisted reproductive technology (ART) procedures and to evaluate the implications of findings in selecting candidates for elective single embryo transfer (eSET).
Methods
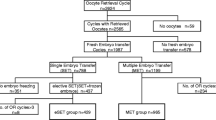
Factors predicting double embryo implantation, defined as embryo transfers with two or more heartbeats on 6-week ultrasound following DET, were assessed using the US National ART Surveillance System data from 2000 to 2012 (n = 1,793,067 fresh, autologous transfers). Adjusted risk ratios (aRRs) were estimated after stratifying by prognosis. Favorable prognosis was defined as first-time ART with supernumerary embryo(s) cryopreserved. Average prognosis was defined as first-time ART without supernumerary embryo(s) cryopreserved, prior unsuccessful ART with supernumerary embryo(s) cryopreserved, or prior ART with previous birth(s) conceived with ART or naturally. Rates and factors associated with double embryo implantation were compared with single embryo implantation following DET among both prognosis groups.
Results
Double embryo implantation was positively associated with blastocyst (versus cleavage) transfer in favorable (aRR = 1.58 (1.51–1.65)) and average (aRR = 1.67 (1.60–1.75)) prognosis groups and negatively associated with age >35 years in both prognosis groups. For average prognosis patients, double embryo implantation was associated with retrieving >10 oocytes (aRR = 1.22 (1.18–1.24)).
Conclusions
Regardless of prognosis, patients aged <35 years with blastocyst-stage embryos and average prognosis patients from whom >10 oocytes were retrieved may be good candidates for eSET. Physicians may consider using these data to counsel patients on eSET, which would reduce multiple gestations and associated complications.


Similar content being viewed by others
Abbreviations
- SET:
-
Single embryo transfer
- DET:
-
Double embryo transfer
- TET:
-
Triple embryo transfer
- QET+:
-
Quadruple or higher embryo transfer
- ET:
-
Embryo transfer
- eSET:
-
Elective single embryo transfer
- ART:
-
Assisted reproductive technology
References
Templeton A, Morris JK. Reducing the risk of multiple births by transfer of two embryos after in vitro fertilization. N Engl J Med. 1998;339(9):573–7. doi:10.1056/NEJM199808273390901.
Kulkarni AD, Jamieson DJ, Jones Jr HW, Kissin DM, Gallo MF, Macaluso M, et al. Fertility treatments and multiple births in the United States. N Engl J Med. 2013;369(23):2218–25. doi:10.1056/NEJMoa1301467.
Sunderam S, Kissin DM, Crawford S, Anderson JE, Folger SG, Jamieson DJ et al. Assisted reproductive technology surveillance—United States, 2010. Morbidity and mortality weekly report surveillance summaries (Washington, DC: 2002). 2013;62(9):1–24.
The ESHRE Capri Workshop Group. Multiple gestation pregnancy. Hum Reprod. 2000;15(8):1856–64.
Centers for Disease Control and Prevention ASfRM, Society for Assisted Reproductive Technology. 2013 assisted reproductive technology national summary report. Atlanta: US Department of Health and Human Services; 2015.
Sazonova A, Kallen K, Thurin-Kjellberg A, Wennerholm UB, Bergh C. Neonatal and maternal outcomes comparing women undergoing two in vitro fertilization (IVF) singleton pregnancies and women undergoing one IVF twin pregnancy. Fertil Steril. 2013;99(3):731–7. doi:10.1016/j.fertnstert.2012.11.023.
Joshi N, Kissin D, Anderson JE, Session D, Macaluso M, Jamieson DJ. Trends and correlates of good perinatal outcomes in assisted reproductive technology. Obstet Gynecol. 2012;120(4):843–51. doi:10.1097/AOG.0b013e318269c0e9.
Practice Committee of Society for Assisted Reproductive Technology, Practice Committee of American Society for Reproductive Medicine. Elective single-embryo transfer. Fertil Steril. 2012;97(4):835–42. doi:10.1016/j.fertnstert.2011.11.050.
Practice Committee of American Society for Reproductive Medicine, Practice Committee of Society for Assisted Reproductive Technology. Criteria for number of embryos to transfer: a committee opinion. Fertil Steril. 2013;99(1):44–6. doi:10.1016/j.fertnstert.2012.09.038.
Steinberg ML, Boulet S, Kissin D, Warner L, Jamieson DJ. Elective single embryo transfer trends and predictors of a good perinatal outcome—United States, 1999 to 2010. Fertil Steril. 2013;99(7):1937–43. doi:10.1016/j.fertnstert.2013.01.134.
Kissin DM, Kulkarni AD, Kushnir VA, Jamieson DJ, National ARTSSG. Number of embryos transferred after in vitro fertilization and good perinatal outcome. Obstet Gynecol. 2014;123(2 Pt 1):239–47. doi:10.1097/AOG.0000000000000106.
Hunault CC, Eijkemans MJC, Pieters MHEC, te Velde ER, Habbema JDF, Fauser BCJM, et al. A prediction model for selecting patients undergoing in vitro fertilization for elective single embryo transfer. Fertil Steril. 2002;77(4):725–32. doi:10.1016/S0015-0282(01)03243-5.
Groeneveld E, Lambers MJ, Stakelbeek ME, Mooij TM, van den Belt-Dusebout AW, Heymans MW, et al. Factors associated with dizygotic twinning after IVF treatment with double embryo transfer. Hum Reprod. 2012;27(10):2966–70. doi:10.1093/humrep/des258.
Gianaroli L, Magli MC, Gambardella L, Giusti A, Grugnetti C, Corani G. Objective way to support embryo transfer: a probabilistic decision. Hum Reprod. 2013;28(5):1210–20. doi:10.1093/humrep/det030.
Strandell A, Bergh C, Lundin K. Selection of patients suitable for one-embryo transfer may reduce the rate of multiple births by half without impairment of overall birth rates. Hum Reprod. 2000;15(12):2520–5.
Hellberg D, Blennborn M, Nilsson S. Defining women who are prone to have twins in in vitro fertilization—a necessary step towards single embryo transfer. J Assist Reprod Genet. 2005;22(5):199–206.
Vilska S, Tiitinen A, Hyden-Granskog C, Hovatta O. Elective transfer of one embryo results in an acceptable pregnancy rate and eliminates the risk of multiple birth. Hum Reprod. 1999;14(9):2392–5.
Gerris J, De Neubourg D, Mangelschots K, Van Royen E, Van de Meerssche M, Valkenburg M. Prevention of twin pregnancy after in-vitro fertilization or intracytoplasmic sperm injection based on strict embryo criteria: a prospective randomized clinical trial. Hum Reprod. 1999;14(10):2581–7. doi:10.1093/humrep/14.10.2581.
Fertility Clinic Success Rate and Certification Act of 1992 (FCSRCA), Public Law 102–493 (1992).
Practice Committee of the Society for Assisted Reproductive Technology, The American Society for Reproductive Medicine. Guidelines on the number of embryos transferred. Fertil Steril. 2004;82 Suppl 1:S1–2. doi:10.1016/j.fertnstert.2004.07.937.
Practice Committees of the American Society for Reproductive Medicine, The Society for Assisted Reproductive Technology. Blastocyst culture and transfer in clinical-assisted reproduction: a committee opinion. Fertil Steril. 2013;99(3):667–72. doi:10.1016/j.fertnstert.2013.01.087.
Kresowik JDK, Sparks AET, Van Voorhis BJ. Clinical factors associated with live birth after single embryo transfer. Fertil Steril. 2012;98(5):1152–6. doi:10.1016/j.fertnstert.2012.07.1141.
Sifer C, Sermondade N, Poncelet C, Hafhouf E, Porcher R, Cedrin-Durnerin I, et al. Biological predictive criteria for clinical pregnancy after elective single embryo transfer. Fertil Steril. 2011;95(1):427–30. doi:10.1016/j.fertnstert.2010.07.1055.
Kissin DM, Kulkarni AD, Mneimneh A, Warner L, Boulet SL, Crawford S, et al. Embryo transfer practices and multiple births resulting from assisted reproductive technology: an opportunity for prevention. Fertil Steril. 2015;103(4):954–61. doi:10.1016/j.fertnstert.2014.12.127.
Luke B, Brown MB, Wantman E, Stern JE, Baker VL, Widra E, et al. A prediction model for live birth and multiple births within the first three cycles of assisted reproductive technology. Fertil Steril. 2014;102(3):744–52. doi:10.1016/j.fertnstert.2014.05.020.
Papanikolaou EGMDP, Camus MMD, Kolibianakis EMMDP, Van Landuyt LB, Van Steirteghem AMDP, Devroey PMDP. In vitro fertilization with single blastocyst-stage versus single cleavage-stage embryos. N Engl J Med. 2006;354(11):1139–46.
Stillman RJ, Richter KS, Banks NK, Graham JR. Elective single embryo transfer: a 6-year progressive implementation of 784 single blastocyst transfers and the influence of payment method on patient choice. Fertil Steril. 2009;92(6):1895–906. doi:10.1016/j.fertnstert.2008.09.023.
Baker VL, Brown MB, Luke B, Conrad KP. Association of number of retrieved oocytes with live birth rate and birth weight: an analysis of 231,815 cycles of in vitro fertilization. Fertil Steril. 2015;103(4):931–8.e2. doi:10.1016/j.fertnstert.2014.12.120.
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999;14(9):2345–9. doi:10.1093/humrep/14.9.2345.
Wang JG, Douglas NC, Dicken C, Nakhuda GS, Guarnaccia MM, Sauer MV. Cryopreservation of supernumerary high quality embryos predicts favorable outcomes for patients undergoing repeated cycles of in vitro fertilization. Fertil Steril. 2008;89(2):368–74. doi:10.1016/j.fertnstert.2007.03.031.
Stern JE, Lieberman ES, Macaluso M, Racowsky C. Is cryopreservation of embryos a legitimate surrogate marker of embryo quality in studies of assisted reproductive technology conducted using national databases? Fertil Steril. 2012;97(4):890–3. doi:10.1016/j.fertnstert.2011.12.050.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen–thawed embryo transfer in normal responders. Fertil Steril. 2011;96(2):344–8. doi:10.1016/j.fertnstert.2011.05.050.
Vitthala S, Gelbaya TA, Brison DR, Fitzgerald CT, Nardo LG. The risk of monozygotic twins after assisted reproductive technology: a systematic review and meta-analysis. Hum Reprod Update. 2009;15(1):45–55. doi:10.1093/humupd/dmn045.
Mneimneh AS, Boulet SL, Sunderam S, Zhang Y, Jamieson DJ, Crawford S, et al. States Monitoring Assisted Reproductive Technology (SMART) collaborative: data collection, linkage, dissemination, and use. J Women’s Health. 2013;22(7):571–7. doi:10.1089/jwh.2013.4452.
Acknowledgments
Caitlin Martin received support from the Marianne Ruby Award in Obstetrics and Gynecology from the Department of Gynecology and Obstetrics of Emory University. We acknowledge Dr. Luca Gianaroli for his help with the initial concept of the study and Dr. Jennifer Kawwass for her critical evaluation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by CDC’s institutional review board.
Authors’ role
All authors helped design the study and critically edit the manuscript. C.M. wrote the manuscript. J.C. performed the statistical analysis. C.M., J.C., S.B., and D.K. worked on the data analysis. All authors approved the final version of the manuscript.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Additional information
Capsule
Predictors of double embryo implantation following double embryo transfer are age <35 years and blastocyst transfer in patients with favorable or average prognosis and retrieval of >10 oocytes in patients with average prognosis. Physicians will find this information useful when counseling patients with these characteristics, and these patients may be good candidates for eSET, which would reduce multiple gestations and associated complications.
Rights and permissions
About this article
Cite this article
Martin, C., Chang, J., Boulet, S. et al. Factors predicting double embryo implantation following double embryo transfer in assisted reproductive technology: implications for elective single embryo transfer. J Assist Reprod Genet 33, 1343–1353 (2016). https://doi.org/10.1007/s10815-016-0770-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0770-9