Abstract
Purpose
The purpose of the study is to evaluate the association between donor TSH level (independent of recipient TSH level) and recipient pregnancy outcome among fresh donor oocyte IVF cycles.
Methods
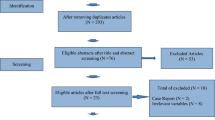
This is a retrospective cohort study investigating 232 consecutive fresh donor-recipient cycles (200 total oocyte donors) at an academic medical center. Main outcome measures include clinical pregnancy and live birth.
Results
Cycles were categorized into two groups based on donor TSH level (< 2.5 and ≥ 2.5 mIU/L). After controlling for multiple donor and recipient characteristics, the probability of clinical pregnancy was significantly lower among donors with TSH levels ≥2.5 mIU/L compared to those with TSH values <2.5 mIU/L (43.1 %, 95 % CI 28.5–58.9, versus 66.7 %, 95 % CI 58.6–73.9, respectively, p = 0.01). The difference in live birth rates between the two groups did not achieve statistical significance (43.1 %, 95 % CI 28.8–58.6, versus 58.0 %, 95 % CI 50.0–65.6, respectively, p = 0.09).
Conclusions
Donor TSH level, independent of recipient TSH level, is associated with recipient clinical pregnancy. These findings suggest that thyroid function may impact the likelihood of pregnancy at the level of the oocyte.
Similar content being viewed by others
References
Colicchia M, Campagnolo L, Baldini E, Ulisse S, Valensise H, Moretti C. Molecular basis of thyrotropin and thyroid hormone action during implantation and early development. Hum Reprod Update. 2014;20(6):884–904. doi:10.1093/humupd/dmu028.
Detti L, Uhlmann RA, Fletcher NM, Diamond MP, Saed GM. Endometrial signaling pathways during ovarian stimulation for assisted reproduction technology. Fertil Steril. 2013;100(3):889–94. doi:10.1016/j.fertnstert.2013.05.027.
Aghajanova L, Stavreus-Evers A, Lindeberg M, Landgren BM, Sparre LS, Hovatta O. Thyroid-stimulating hormone receptor and thyroid hormone receptors are involved in human endometrial physiology. Fertil Steril. 2011;95(1):230–7. doi:10.1016/j.fertnstert.2010.06.079. 7 e1-2.
Practice Committee of American Society for Reproductive M. Diagnostic evaluation of the infertile female: a committee opinion. Fertil Steril. 2012;98(2):302–7. doi:10.1016/j.fertnstert.2012.05.032.
Gracia CR, Morse CB, Chan G, Schilling S, Prewitt M, Sammel MD, et al. Thyroid function during controlled ovarian hyperstimulation as part of in vitro fertilization. Fertil Steril. 2012;97(3):585–91. doi:10.1016/j.fertnstert.2011.12.023.
Fitko R, Kucharski J, Szlezyngier B, Jana B. The concentration of GnRH in hypothalamus, LH and FSH in pituitary, LH, PRL and sex steroids in peripheral and ovarian venous plasma of hypo- and hyperthyroid, cysts-bearing gilts. Anim Reprod Sci. 1996;45(1–2):123–38.
Lindsay AN, Voorhess ML, MacGillivray MH. Multicystic ovaries in primary hypothyroidism. Obstet Gynecol. 1983;61(4):433–7.
Wakim AN, Paljug WR, Jasnosz KM, Alhakim N, Brown AB, Burholt DR. Thyroid hormone receptor messenger ribonucleic acid in human granulosa and ovarian stromal cells. Fertil Steril. 1994;62(3):531–4.
Cecconi S, Rucci N, Scaldaferri ML, Masciulli MP, Rossi G, Moretti C, et al. Thyroid hormone effects on mouse oocyte maturation and granulosa cell aromatase activity. Endocrinology. 1999;140(4):1783–8. doi:10.1210/endo.140.4.6635.
Styer AK, Wright DL, Wolkovich AM, Veiga C, Toth TL. Single-blastocyst transfer decreases twin gestation without affecting pregnancy outcome. Fertil Steril. 2008;89(6):1702–8. doi:10.1016/j.fertnstert.2007.05.036.
Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinologist. 2012;18(6):988–1028.
Rae MT, Gubbay O, Kostogiannou A, Price D, Critchley HO, Hillier SG. Thyroid hormone signaling in human ovarian surface epithelial cells. J Clin Endocrinol Metab. 2007;92(1):322–7. doi:10.1210/jc.2006-1522.
Poppe K, Velkeniers B. Female infertility and the thyroid. Best Pract Res Clin Endocrinol Metab. 2004;18(2):153–65. doi:10.1016/j.beem.2004.03.004.
Karmon AE, Batsis M, Chavarro JE, Souter I. Preconceptional thyroid-stimulating hormone levels and outcomes of intrauterine insemination among euthyroid infertile women. Fertil Steril. 2015;103(1):258–63.e1. doi:10.1016/j.fertnstert.2014.09.035.
Krassas GE, Pontikides N, Kaltsas T, Papadopoulou P, Paunkovic J, Paunkovic N, et al. Disturbances of menstruation in hypothyroidism. Clin Endocrinol. 1999;50(5):655–9.
Scoccia B, Demir H, Kang Y, Fierro MA, Winston NJ. In vitro fertilization pregnancy rates in levothyroxine-treated women with hypothyroidism compared to women without thyroid dysfunction disorders. Thyroid Off J Am Thyroid Assoc. 2012;22(6):631–6. doi:10.1089/thy.2011.0343.
Kim CH, Ahn JW, Kang SP, Kim SH, Chae HD, Kang BM. Effect of levothyroxine treatment on in vitro fertilization and pregnancy outcome in infertile women with subclinical hypothyroidism undergoing in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2011;95(5):1650–4. doi:10.1016/j.fertnstert.2010.12.004.
Cramer DW, Sluss PM, Powers RD, McShane P, Ginsburgs ES, Hornstein MD, et al. Serum prolactin and TSH in an in vitro fertilization population: is there a link between fertilization and thyroid function? J Assist Reprod Genet. 2003;20(6):210–5.
Wakim AN, Polizotto SL, Buffo MJ, Marrero MA, Burholt DR. Thyroid hormones in human follicular fluid and thyroid hormone receptors in human granulosa cells. Fertil Steril. 1993;59(6):1187–90.
Gilbert RM, Hadlow NC, Walsh JP, Fletcher SJ, Brown SJ, Stuckey BG, et al. Assessment of thyroid function during pregnancy: first-trimester (weeks 9–13) reference intervals derived from Western Australian women. Med J Aust. 2008;189(5):250–3.
Reh A, Grifo J, Danoff A. What is a normal thyroid-stimulating hormone (TSH) level? Effects of stricter TSH thresholds on pregnancy outcomes after in vitro fertilization. Fertil Steril. 2010;94(7):2920–2. doi:10.1016/j.fertnstert.2010.06.041.
Aghahosseini M, Asgharifard H, Aleyasin A, Tehrani Banihashemi A. Effects of thyroid stimulating hormone (TSH) level on clinical pregnancy rate via in vitro fertilization (IVF) procedure. Med J Islam Repub Iran. 2014;28:46.
Acknowledgments
We would like to express our gratitude to the Deborah Kelly Center for Outcomes Research of the Vincent Department of Obstetrics and Gynecology, Massachusetts General Hospital for the generous support of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Capsule These findings suggest that thyroid function may impact the likelihood of pregnancy at the level of the oocyte.
Rights and permissions
About this article
Cite this article
Karmon, A.E., Cardozo, E.R., Souter, I. et al. Donor TSH level is associated with clinical pregnancy among oocyte donation cycles. J Assist Reprod Genet 33, 489–494 (2016). https://doi.org/10.1007/s10815-016-0668-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0668-6