Abstract
Purpose
The aim of this study was to (1) investigate the incidence of embryos derived from “unfertilized oocytes” i.e., oocytes not displaying pronuclei (0PN) at the time of the fertilization check and (2) determine the clinical pregnancy rates when transferring 0PN-derived embryos.
Methods
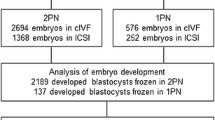
In this retrospective study, 4424 IVF-ET cycles were reviewed.
Results
In total, 11.3 % (4966/43,949) 0PN-derived embryos were observed. It was found that female age, number of oocytes, and the top-quality embryo rate were significantly correlated with 0PN-derived embryo occurrence. The source of embryos transferred did not impact significantly on clinical pregnancy and live-birth rates. Of the 183 cycles included in this study where 275 0PN-derived embryos were transferred in total, only 0PN-derived embryos were available in 70 of those cycles. It was noteworthy that 13 healthy infants resulted from 0PN-derived embryos with an implantation rate of 17.0 %.
Conclusion
These results indicate that the traditional method of excluding embryos because of those oocytes originally lacking any sign of a pronucleus at the fertilization check should be re-considered as transferring 0PN-derived embryos with subsequent expected developmental performance may be considered as an option for those patients where no other embryos are available.
Similar content being viewed by others
References
Staessen C et al. Cytogenetic and morphological observations of single pronucleated human oocytes after in-vitro fertilization. Hum Reprod. 1993;8(2):221–3.
Gras L, Trounson AO. Pregnancy and birth resulting from transfer of a blastocyst observed to have one pronucleus at the time of examination for fertilization. Hum Reprod. 1999;14(7):1869–71.
Feenan K, Herbert M. Can ‘abnormally’ fertilized zygotes give rise to viable embryos? Hum Fertil (Camb). 2006;9(3):157–69.
Aoi YT, Saitou H, Takiue C, Kawakami N, Tone M, Hirata R, et al. Development potential and clinical implication of embryos having either one pronucleus, (1PN) or no pronuclei (0PN). Hum Reprod. 2010;25(20100600):i184–5.
Lee C, Yap WY, Low SY, Lim YX. Euploidy rates for day 3 apronuclear (0PN) and unipronuclear (1PN) embryos. Reprod BioMed Online. 2013;26:S36.
Manor D et al. Undocumented embryos: do not trash them, FISH them. Hum Reprod. 1996;11(11):2502–6.
Burney RO et al. Normal pregnancy resulting from a non-pronuclear oocyte at the time of examination for fertilization. Clin Exp Obstet Gynecol. 2008;35(3):170–1.
Wang XL et al. Outcomes of day 3 embryo transfer with vitrification using Cryoleaf: a 3-year follow-up study. J Assist Reprod Genet. 2012;29(9):883–9.
Reichman DE, Jackson KV, Racowsky C. Incidence and development of zygotes exhibiting abnormal pronuclear disposition after identification of two pronuclei at the fertilization check. Fertil Steril. 2010;94(3):965–70.
Huguet E et al. Time-lapse technology provides relevant information about one pronucleus zygotes (1PNZ) observed with conventional microscopy in the decision-making process. Fertil Steril. 2013;100(3):S237.
Fancsovits P et al. Early pronuclear breakdown is a good indicator of embryo quality and viability. Fertil Steril. 2005;84(4):881–7.
Munne S, Cohen J. Chromosome abnormalities in human embryos. Hum Reprod Update. 1998;4(6):842–55.
Chen C, Kattera S. Rescue ICSI of oocytes that failed to extrude the second polar body 6 h post-insemination in conventional IVF. Hum Reprod. 2003;18(10):2118–21.
Callan VJ, Hennessey JF. Emotional aspects and support in in vitro fertilization and embryo transfer programs. J In Vitro Fert Embryo Transf. 1988;5(5):290–5.
Noyes N et al. Embryo biopsy: the fate of abnormal pronuclear embryos. Reprod Biomed Online. 2008;17(6):782–8.
Werlin L. Are embryos normal obtained from second-day intracytoplasmic sperm injection (ICSI), single pronucleus (1PN), or cleaved embryos from no pronuclei (0PN) initially seen? Fertil Steril. 2007;87(0015–0282):s11–2.
Gianaroli L et al. Pronuclear morphology and chromosomal abnormalities as scoring criteria for embryo selection. Fertil Steril. 2003;80(2):341–9.
Edirisinghe WR, Murch AR, Yovich JL. Cytogenetic analysis of human oocytes and embryos in an in-vitro fertilization programme. Hum Reprod. 1992;7(2):230–6.
Ciray HN et al. Time-lapse evaluation of human embryo development in single versus sequential culture media—a sibling oocyte study. J Assist Reprod Genet. 2012;29(9):891–900.
Rienzi L et al. Significance of morphological attributes of the early embryo. Reprod Biomed Online. 2005;10(5):669–81.
Ming L, L.J.S., Ping Z, Jie Q, Ping L. Evaluate the outcome of embryo transfers just from 0PN oocyte in 101 fresh IVF-ET cycles. Chin J Clin Obstet Qynecol. 2013;14(5): 427–9.
Kondoh E et al. Stress affects uterine receptivity through an ovarian-independent pathway. Hum Reprod. 2009;24(4):945–53.
Acknowledgments
The authors thank Dr. Tim Dineen and Dr. Julie O’Callaghan, members of Cork Fertility Centre, for their assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Zygotes not demonstrating PN at fertilization check are capable of generating term pregnancies.
Rights and permissions
About this article
Cite this article
Liu, J., Wang, X.L., Zhang, X. et al. Live births resulting from 0PN-derived embryos in conventional IVF cycles. J Assist Reprod Genet 33, 373–378 (2016). https://doi.org/10.1007/s10815-015-0644-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0644-6