Abstract
Purpose
To compare the in-vitro fertilization (IVF) outcomes of cancer patients who underwent oocyte retrieval and embryo/oocyte cryopreservation prior to gonadotoxic therapy to those of age and time-matched controls with tubal factor infertility.
Methods
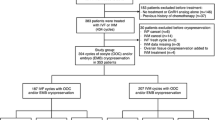
All cancer patients who underwent embryo/oocyte cryopreservation at our institution from 1997 to 2014 were reviewed. Primary outcomes were total dose of gonadotropins used, number of oocytes retrieved, and number of 2pn embryos obtained. Outcomes were compared to age-matched controls with tubal-factor infertility who underwent a fresh embryo transfer within the same relative time period as the IVF cycle of the cancer patient.
Results
Sixty-three cancer patients underwent 65 IVF cycles, and 21 returned for frozen embryo transfer. One hundred twenty-two age-matched controls underwent IVF cycles with fresh transfer, and 23 returned for frozen embryo transfer. No difference was seen between cancer patients and controls with respect to total ampules of gonadotropin used (38.0 vs. 35.6 respectively; p = 0.28), number of oocytes retrieved (12.4 vs. 10.9 respectively; p = 0.36) and number of 2pn embryos obtained (6.6 vs. 7.1 respectively; p = 0.11). Cumulative pregnancy rate per transfer for cancer patients compared to controls was 37 vs. 43 % respectively (p = 0.49) and cumulative live birth rate per transfer was 30 vs. 32 % respectively (p = 0.85). Cancer patients had a higher likelihood of live birth resulting in twins (44 vs. 14 %; p = 0.035).
Conclusions
Most IVF outcomes appear comparable for cancer patients and age-matched controls. Higher twin pregnancy rates in cancer patients may reflect lack of underlying infertility or need for cancer-specific transfer guidelines.


Similar content being viewed by others
References
Cancer Survivors — United States, 2007 [Internet]. [cited 2014 Jun 3]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6009a1.htm.
National Cancer Institute. Surveillance Epidemiology and End Results. Fast Stats. Statistics stratified by age. Available at: http://seer.cancer.gov/faststats/selections.php. Accessed on 12 Oct 2014.
Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360(9):902–11. doi:10.1056/NEJMra0801454.
Donnez J, Dolmans MM. Fertility preservation in women. Nat Rev Endocrinol. 2013;9(12):735–49. doi:10.1038/nrendo.2013.205.
Loprinzi CL, Wolf SL, Barton DL, Laack NN. Symptom management in premenopausal patients with breast cancer. Lancet Oncol. 2008;9(10):993–1001. doi:10.1016/S1470-2045(08)70256-0.
Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009;15(5):587–97. doi:10.1093/humupd/dmp015.
Reh AE, Lu L, Weinerman R, Grifo J, Krey L, Noyes N. Treatment outcomes and quality-of-life assessment in a university-based fertility preservation program: results of a registry of female cancer patients at 2 years. J Assist Reprod Genet. 2011;28(7):635–41. doi:10.1007/s10815-011-9559-z.
Schover LR. Patient attitudes toward fertility preservation. Pediatr Blood Cancer. 2009;53(2):281–4. doi:10.1002/pbc.22001.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol: Off J Am Soc Clin Oncol. 2013;31(19):2500–10. doi:10.1200/JCO.2013.49.2678.
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118(6):1710–7. doi:10.1002/cncr.26459.
Rienzi L, Cobo A, Paffoni A, Scarduelli C, Capalbo A, Vajta G, et al. Consistent and predictable delivery rates after oocyte vitrification: an observational longitudinal cohort multicentric study. Hum Reprod. 2012;27(6):1606–12. doi:10.1093/humrep/des088.
Ethics Committee of American Society for Reproductive M. Fertility preservation and reproduction in patients facing gonadotoxic therapies: a committee opinion. Fertil Steril. 2013;100(5):1224–31. doi:10.1016/j.fertnstert.2013.08.041.
Kim J, Deal AM, Balthazar U, Kondapalli LA, Gracia C, Mersereau JE. Fertility preservation consultation for women with cancer: are we helping patients make high-quality decisions? Reprod Biomed Online. 2013;27(1):96–103. doi:10.1016/j.rbmo.2013.03.004.
Practice Committees of American Society for Reproductive M, Society for Assisted Reproductive T. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99(1):37–43. doi:10.1016/j.fertnstert.2012.09.028.
Styer AK, Wright DL, Wolkovich AM, Veiga C, Toth TL. Single-blastocyst transfer decreases twin gestation without affecting pregnancy outcome. Fertil Steril. 2008;89(6):1702–8. doi:10.1016/j.fertnstert.2007.05.036.
Testart J, Lassalle B, Belaisch-Allart J, Hazout A, Forman R, Rainhorn JD, et al. High pregnancy rate after early human embryo freezing. Fertil Steril. 1986;46(2):268–72.
Berin I, McLellan ST, Macklin EA, Toth TL, Wright DL. Frozen-thawed embryo transfer cycles: clinical outcomes of single and double blastocyst transfers. J Assist Reprod Genet. 2011;28(7):575–81. doi:10.1007/s10815-011-9551-7.
Frattarelli JL, Miller BT, Scott Jr RT. Adjuvant therapy enhances endometrial receptivity in patients undergoing assisted reproduction. Reprod Biomed Online. 2006;12(6):722–9.
Waldenstrom U, Hellberg D, Nilsson S. Low-dose aspirin in a short regimen as standard treatment in in vitro fertilization: a randomized, prospective study. Fertil Steril. 2004;81(6):1560–4. doi:10.1016/j.fertnstert.2004.02.082.
Rubinstein M, Marazzi A, Polak de Fried E. Low-dose aspirin treatment improves ovarian responsiveness, uterine and ovarian blood flow velocity, implantation, and pregnancy rates in patients undergoing in vitro fertilization: a prospective, randomized, double-blind placebo-controlled assay. Fertil Steril. 1999;71(5):825–9.
Veeck LL, Bodine R, Clarke RN, Berrios R, Libraro J, Moschini RM, et al. High pregnancy rates can be achieved after freezing and thawing human blastocysts. Fertil Steril. 2004;82(5):1418–27. doi:10.1016/j.fertnstert.2004.03.068.
Practice Committee of American Society for Reproductive M. Ovarian tissue cryopreservation: a committee opinion. Fertil Steril. 2014;101(5):1237–43. doi:10.1016/j.fertnstert.2014.02.052.
Cakmak H, Katz A, Cedars MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100(6):1673–80. doi:10.1016/j.fertnstert.2013.07.1992.
Keskin U, Ercan CM, Yilmaz A, Babacan A, Korkmaz C, Duru NK, et al. Random-start controlled ovarian hyperstimulation with letrozole for fertility preservation in cancer patients: case series and review of literature. JPMA J Pak Med Assoc. 2014;64(7):830–2.
Klock SC, Zhang JX, Kazer RR. Fertility preservation for female cancer patients: early clinical experience. Fertil Steril. 2010;94(1):149–55. doi:10.1016/j.fertnstert.2009.03.028.
Michaan N, Ben-David G, Ben-Yosef D, Almog B, Many A, Pauzner D, et al. Ovarian stimulation and emergency in vitro fertilization for fertility preservation in cancer patients. Eur J Obstet Gynecol Reprod Biol. 2010;149(2):175–7. doi:10.1016/j.ejogrb.2009.12.023.
Pavone ME, Hirshfeld-Cytron J, Lawson AK, Smith K, Kazer R, Klock S. Fertility preservation outcomes may differ by cancer diagnosis. J Human Reprod Sci. 2014;7(2):111–8. doi:10.4103/0974-1208.138869.
Practice Committee of the American Society for Reproductive M. Aging and infertility in women. Fertil Steril. 2006;86(5 Suppl 1):S248–52. doi:10.1016/j.fertnstert.2006.08.024.
Devesa M, Martinez F, Coroleu B, Rodriguez I, Gonzalez C, Barri PN. Ovarian response to controlled ovarian hyperstimulation in women with cancer is as expected according to an age-specific nomogram. J Assist Reprod Genet. 2014;31(5):583–8. doi:10.1007/s10815-014-0183-6.
Johnson LN, Dillon KE, Sammel MD, Efymow BL, Mainigi MA, Dokras A, et al. Response to ovarian stimulation in patients facing gonadotoxic therapy. Reprod Biomed Online. 2013;26(4):337–44. doi:10.1016/j.rbmo.2013.01.003.
Nurudeen SK, Douglas NC, Mahany EL, Sauer MV, Choi JM. Fertility preservation decisions among newly diagnosed oncology patients: a single-center experience. Am J Clin Oncol. 2014. doi:10.1097/COC.0000000000000031.
Knopman JM, Noyes N, Talebian S, Krey LC, Grifo JA, Licciardi F. Women with cancer undergoing ART for fertility preservation: a cohort study of their response to exogenous gonadotropins. Fertil Steril. 2009;91(4 Suppl):1476–8. doi:10.1016/j.fertnstert.2008.07.1727.
Quintero RB, Helmer A, Huang JQ, Westphal LM. Ovarian stimulation for fertility preservation in patients with cancer. Fertil Steril. 2010;93(3):865–8. doi:10.1016/j.fertnstert.2008.10.007.
Friedler S, Koc O, Gidoni Y, Raziel A, Ron-El R. Ovarian response to stimulation for fertility preservation in women with malignant disease: a systematic review and meta-analysis. Fertil Steril. 2012;97(1):125–33. doi:10.1016/j.fertnstert.2011.10.014.
Garcia-Velasco JA, Domingo J, Cobo A, Martinez M, Carmona L, Pellicer A. Five years’ experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil Steril. 2013;99(7):1994–9. doi:10.1016/j.fertnstert.2013.02.004.
Domingo J, Guillen V, Ayllon Y, Martinez M, Munoz E, Pellicer A, et al. Ovarian response to controlled ovarian hyperstimulation in cancer patients is diminished even before oncological treatment. Fertil Steril. 2012;97(4):930–4. doi:10.1016/j.fertnstert.2012.01.093.
Reddy J, Oktay K. Ovarian stimulation and fertility preservation with the use of aromatase inhibitors in women with breast cancer. Fertil Steril. 2012;98(6):1363–9. doi:10.1016/j.fertnstert.2012.09.022.
Agarwal A, Said TM. Implications of systemic malignancies on human fertility. Reprod Biomed Online. 2004;9(6):673–9.
Oktay K, Moy F, Titus S, Stobezki R, Turan V, Dickler M, et al. Age-related decline in DNA repair function explains diminished ovarian reserve, earlier menopause, and possible oocyte vulnerability to chemotherapy in women with BRCA mutations. J Clin Oncol: Off J Am Soc Clin Oncol. 2014;32(10):1093–4. doi:10.1200/JCO.2013.53.5369.
Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol: Off J Am Soc Clin Oncol. 2010;28(2):240–4. doi:10.1200/JCO.2009.24.2057.
Robertson AD, Missmer SA, Ginsburg ES. Embryo yield after in vitro fertilization in women undergoing embryo banking for fertility preservation before chemotherapy. Fertil Steril. 2011;95(2):588–91. doi:10.1016/j.fertnstert.2010.04.028.
Sabatini ME, Wolkovich AM, Macklin EA, Wright DL, Souter I, Toth TL. Pronuclear embryo cryopreservation experience: outcomes for reducing the risk of ovarian hyperstimulation syndrome and for fertility preservation in cancer patients. J Assist Reprod Genet. 2011;28(3):279–84. doi:10.1007/s10815-010-9515-3.
Garrido N, Bellver J, Remohi J, Alama P, Pellicer A. Cumulative newborn rates increase with the total number of transferred embryos according to an analysis of 15,792 ovum donation cycles. Fertil Steril. 2012;98(2):341–346 e1-2. doi:10.1016/j.fertnstert.2012.04.039.
Author information
Authors and Affiliations
Corresponding author
Additional information
Eden R. Cardozo and Alexcis P. Thomson contributed equally to this work.
Capsule We report outcomes of 63 women who underwent IVF for fertility preservation prior to chemotherapy. In general they can expect similar outcomes to age matched controls with tubal factor infertility in terms of IVF cycle parameters and outcomes.
Rights and permissions
About this article
Cite this article
Cardozo, E.R., Thomson, A.P., Karmon, A.E. et al. Ovarian stimulation and in-vitro fertilization outcomes of cancer patients undergoing fertility preservation compared to age matched controls: a 17-year experience. J Assist Reprod Genet 32, 587–596 (2015). https://doi.org/10.1007/s10815-015-0428-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0428-z