Abstract
Purpose
The study was designed to evaluate the relationship between serum progesterone (P4) response after hCG administration and the number of oocytes retrieved and the embryo quality in fresh IVF cycles.
Methods
We conducted a retrospective cohort study of women aged 24–43 years who underwent first fresh IVF cycle from 2011 to 2013 at a single practice. We compared the post-hCG serum P4 level with values on the day of hCG trigger. Patients were analyzed in long and short protocols independently. In addition, patients were stratified by post-hCG P4 response. Number of oocytes retrieved and embryo quality were the primary outcomes of interest. Ordinary least square regression models and logistic regression analysis models were created to identify predictive factors associated with embryological outcomes while adjusting for potential confounders.
Results
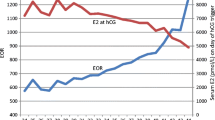
Among the 2,978 IVF cycles, 2,484 patients were in long protocols, and 494 patients were in short protocols. After adjusting for patient age, rFSH duration, and basal FSH levels, the associations between P4 response after hCG administration and number of oocytes retrieved (P < 0.001) remained statistically significant in both long and short protocols. Additionally, mature oocyte rate, fertilization rate, good quality embryo rate, pregnancy rate and implantation rate were not significantly associated with the P4 increase when adjusting for the same factors. However, pregnancy rate and implantation rate from frozen-thawed cycles increased gradually across the seven groups.
Conclusions
Post-hCG P4 levels were positively associated with the number of oocytes retrieved, but did not affect oocyte or embryo quality. Our study suggests that the change in the post-hCG P4 level is another parameter that can be used by clinicians to assess the number of oocytes retrieved, and may further to estimate the pregnancy rate and live birth rate indirectly.
Similar content being viewed by others
References
Srun SW, Nissen BJ, Bryans TD, Bonjean M. Medical device SALs and surgical site infections: a mathematical model. Biomed Instrum Technol. 2012;46:230–7.
Gleicher N, Weghofer A, Barad D. Update on the comparison of assisted reproduction outcomes between Europe and the USA: the 2002 data. Fertil Steril. 2007;87:1301–5.
Hunault CC, Eijkemans MJ, Pieters MH, te Velde ER, Habbema JD, Fauser BC, et al. Antral follicle count at down-regulation and prediction of poor ovarian response. Reprod Biomed Online. 2008;17:508–14.
Traub ML, Van Arsdale A, Pal L, Jindal S, Santoro N. Endometrial thickness, Caucasian ethnicity, and age predict clinical pregnancy following fresh blastocyst embryo transfer: A retrospective cohort. Reprod Biol Endocrinol. 2009;7:33–9.
Pandian Z, Bhattacharya S, Ozturk O, Serour GI, Templeton A. Number of embryos for transfer following in-vitro fertilisation or intra-cytoplasmic sperm injection. Cochrane Database Syst Rev. 2009;2:CD003416.
Thomas MR, Sparks AE, Ryan GL, Van Voorhis BJ. Clinical predictors of human blastocyst formation and pregnancy after extended embryo culture and transfer. Fertil Steril. 2010;94:543–8.
van Loendersloot LL, van Wely M, Limpens J, Bossuyt PMM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Hum Reprod Update. 2010;16:577–89.
Nelson SM, Lawlor DA. Predicting live birth, preterm delivery, and low birth weight in infants born from in vitro fertilisation: a prospective study of 144,018 treatment cycles. PLoS Med. 2011;8:e1000386.
Bosch E, Valencia I, Escudero E, Crespo J, Simon S, Remohi J, et al. Premature luteinization during gonadotropin-releasing hormone antagonist cycles and its relationship with in vitro fertilization outcome. Fertil Steril. 2003;80:1444–9.
Kilic¸dag EB, Haydardedeoglu B, Cok T, Hacivelioglu SO, Bagis T. Premature progesterone elevation impairs implantation and live birth rates in GnRH-agonist IVF/ICSI cycles. Arch Gynecol Obstet. 2010;281:747–52.
Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19:433–57.
Bosch E, Labarta E, Crespo J, Simón C, Remohí J, Jenkins J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization-analysis of over 4,000 cycles. Hum Reprod. 2010;25:2092–100.
Ochsenkühn R, Arzberger A, von Schönfeldt V, Gallwas J, Rogenhofer N, Crispin A, et al. Subtle progesterone rise on the day of human chorionic gonadotropin administration is associated with lower live birth rates in women undergoing assisted reproductive technology: a retrospective study with 2,555 fresh embryo transfers. Fertil Steril. 2012;98:347–54.
Kyrou D, Al-Azemi M, Papanikolaou EG, Donoso P, Tziomalos K, Devroey P, et al. The relationship of premature progesterone rise with serum estradiol levels and number of follicles in GnRH antagonist/recombinant FSH-stimulated cycles. Eur J Obstet Gynecol Reprod Biol. 2012;162:165–8.
Burns WN, Witz CA, Klein NA, Silverberg KM, Schenken RS. Serum progesterone concentrations on the day after human chorionic gonadotropin administration and progesterone/oocyte ratios predict in vitro fertilization/embryo transfer outcome. J Assist Reprod Genet. 1994;11:17–23.
Check JH, Amui J, Choe JK, Brasile D. Relationship of serum progesterone (P) level the day after human chorionic gonadotropin (hCG) injection on outcome following in vitro fertilization-embryo transfer (IVF-ET). Clin Exp Obstet Gynecol. 2009;36:214–5.
Liu L, Zhou F, Lin X, Li T, Tong X, Zhu H, et al. Recurrent IVF failure is associated with elevated progesterone on the day of hCG administration. Eur J Obstet Gynecol Reprod Biol. 2013;171:78–83.
Volpes A, Sammartano F, Coffaro F, Mistretta V, Scaglione P, Allegra A. Number of good quality embryos on day 3 is predictive for both pregnancy and implantation rates in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2004;82:1330–6.
Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z. The optimum number of oocytes in IVF treatment: an analysis of 2,455 cycles in China. Hum Reprod. 2013;28:2728–34.
Kondapalli LA, Molinaro TA, Sammel MD, Dokras A. A decrease in serum estradiol levels after human chorionic gonadotrophin administration predicts significantly lower clinical pregnancy and live rates in in vitro fertilization cycles. Hum Reprod. 2012;27:2690–7.
Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. 2012;97:1321–7.
Acknowledgments
The authors sincerely thank other investigators and physicians who made contributions to this study. This work was supported by grants from the National Natural Science Foundation of China (No. 81270657), the Science and Technology Department Program of Zhejiang (2013C33145), the health department Program of Zhejiang (No. 2012RCA036) and the Natural Science Program of Zhejiang (Y14H040012). There is no conflict of interest in this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Preovulation elavated progesterone was positively associated with the number of oocytes retrieved, but does not affect oocyte or embryo quality.
Rights and permissions
About this article
Cite this article
Zhu, H., Liu, L., Yang, L. et al. The effect of progesterone level prior to oocyte retrieval on the numbers of oocytes retrieved and embryo quality in IVF treatment cycles: an analysis of 2,978 cycles. J Assist Reprod Genet 31, 1183–1187 (2014). https://doi.org/10.1007/s10815-014-0291-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-014-0291-3