Abstract
Purpose
This study uses linked cycles of assisted reproductive technology (ART) to examine cumulative live birth rates, birthweight, and length of gestation by diagnostic category.
Methods
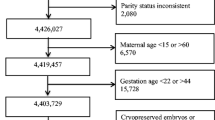
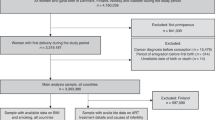
We studied 145,660 women with 235,985 ART cycles reported to the Society for Assisted Reproductive Technology Clinic Outcomes Reporting System during 2004–2010. ART cycles were linked to individual women by name, date of birth, social security number, partner’s name, and sequence of ART treatments. The study population included the first four autologous oocyte cycles for women with a single diagnosis of male factor, endometriosis, ovulation disorders, diminished ovarian reserve, or unexplained infertility. Live birth rates were calculated per cycle, per cycle number (1–4), and cumulatively. Birthweight and length of gestation were calculated for singleton births.
Results
Within each diagnosis, live birth rates were highest in the first cycle and declined with successive cycles. Women with diminished ovarian reserve had the lowest live birth rate (cumulative rate of 28.3 %); the live birth rate for the other diagnoses were very similar (cumulative rates from 62.1 % to 65.7 %). Singleton birthweights and lengths of gestation did not differ substantially across diagnoses, ranging from 3,112 to 3,286 g and 265 to 270 days, respectively. These outcomes were comparable with national averages for singleton births in the United States (3,296 g and 271 days).
Conclusion
Women with the diagnosis of diminished ovarian reserve had substantially lower live birth rates. However, singleton birthweights and lengths of gestation outcomes were similar across all other diagnoses.
Similar content being viewed by others
References
Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. 2002;346(10):731–7.
Reddy UM, Wapner RJ, Rebar RW, Tasca RJ. Infertility, assisted reproductive technology, and adverse pregnancy outcomes: executive summary of a national institute of child health and human development workshop. Obstet Gynecol. 2007;109(4):967–77.
Kalra SK, Ratcliffe SJ, Coutifaris C, Molinaro T, Barnhart KT. Ovarian stimulation and low birth weight in newborns conceived through in vitro fertilization. Obstet Gynecol. 2011;118(4):863–71.
Calhoun KC, Fritz MA, Steiner AZ. Examining the relationship between ovarian reserve, as measured by basal FSH levels, and the risk of poor obstetric outcome in singleton IVF gestations. Hum Reprod. 2011;26(12):3424–30.
Kallen B, Finnstrom O, Nygren K-G, Olausson PO. In vitro fertilization (IVF) in Sweden: infant outcome after different IVF fertilization methods. Fertil Steril. 2005;84(3):611–7.
Schieve LA, Ferre C, Peterson HB, Macaluso M, Reynolds MA, Wright VC. Perinatal outcome among singleton infants conceived through assisted reproductive technology in the United States. Obstet Gynecol. 2004;103(6):1144–53.
Stern JE, Brown MB, Luke B, Wantman E, Lederman A, Hornstein MD, et al. Cycle 1 as predictor of assisted reproductive technology treatment outcome over multiple cycles: an analysis of linked cycles from the society for assisted reproductive technology clinic outcomes reporting system online database. Fertil Steril. 2011;95(2):600–5. doi:10.1016/j.fertnstert.2010.06.009.
Stern JE, Brown MB, Luke B, Wantman E, Lederman A, Missmer SA, et al. Calculating cumulative live-birth rates from linked cycles of assisted reproductive technology (ART): data from the Massachusetts SART CORS. Fertil Steril. 2010;94(4):1334–40. doi:10.1016/j.fertnstert.2009.05.052.
Luke B, Brown MB, Wantman E, Lederman A, Gibbons W, Schattman GL, et al. Cumulative birth rates with linked assisted reproductive technology cycles. N Engl J Med. 2012;366(26):2483–91. doi:10.1056/NEJMoa1110238.
Ramaho de Caraho B, Sobrinho DBG, Vieira ADD, Resende MPS, Barbosa ACP, Silva AA, et al. Ovarian reserve assessment for infertility investigation. ISRN Obstet Gynecol. 2012;2012:576385.
Nangia AK, Luke B, Smith JF, Mak W, Stern JE, Group SW. National study of factors influencing assisted reproductive technology outcomes with male factor infertility. Fertil Steril. 2011;96(3):609–14. doi:10.1016/j.fertnstert.2011.06.026.
Qiao J, Feng HL. Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update. 2011;17(1):17–33. doi:10.1093/humupd/dmq032.
Quaas A, Dorkas A. Diagnosis and treatment of unexplained infertility. Obstet Gynecol. 2008;1(2):69–76.
Maheshwari A, Bhattacharya S (2013) Elective frozen replacement cycles for all: ready for prime time? Hum Reprod. 2013;28(1):6–9. doi:10.1093/humrep/des386.
Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Kirmeyer S, Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70.
Boomsma CM, Eijkemans MJC, Hughes EG, Visser GHA, Fauser BCJM, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update. 2006;12(6):673–83.
Axmon A, Hagmar L. Time to pregnancy and pregnancy outcome. Fertil Steril. 2005;84(4):966–74.
Luke B, Cabral H, Cohen BB, Hoang L, Plummer KM, Kotelchuck M. Comparison of measures in SART database and Massachusetts vital statistics. Fertil Steril. 2012;98:S76–7.
Acknowledgements
SART wishes to thank all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Cumulave live birth rate after 4 cycles of ART varied with infertility diagnosis while length of gestation and birthweight did not.
Rights and permissions
About this article
Cite this article
Stern, J.E., Brown, M.B., Wantman, E. et al. Live birth rates and birth outcomes by diagnosis using linked cycles from the SART CORS database. J Assist Reprod Genet 30, 1445–1450 (2013). https://doi.org/10.1007/s10815-013-0092-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0092-0