Abstract
Objective
To compare cytogenetic data of first-trimester missed abortions in intracytoplasmic sperm injection (ICSI) for non-male factor-mediated and spontaneous pregnancies.
Methods
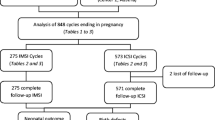
Using karyotype analysis, we conducted a retrospective cohort trial of missed abortions following ICSI for non-male factor and spontaneous pregnancies. Patients experienced missed abortions during the first 12 weeks of pregnancy. Dilation and curettage procedure was performed followed by cytogenetic evaluations. Two patient groups were created: ICSI (n = 71) and spontaneous pregnancies (n = 81). At least 20 GTG-banded metaphases were analyzed in each case for cytogenetic analyses. Statistical analyses were performed using NCSS 2007 Statistical Program software. The significance level and confidence interval for all analyses were set to p < 0.05 and a 95% confidence interval, respectively.
Results
A total of 49.3% (75/152) of the miscarriages were cytogenetically abnormal among the patients. We detected cytogenetically abnormalities in 47.9% (34/71) of the ICSI group and 50.6% (41/81) of the control group, which were not statistically significant differences (p=NS). The sex chromosome abnormalities were similar between the ICSI and control groups (p=NS). The most prevalent abnormalities that were observed in the ICSI and control groups with first-trimester pregnancy loss were trisomy (n = 42; 27.6%), Turner syndrome (45, X0, n = 13; 8.6%), triploidy (n = 13; 8.6%), 48 chromosomes (n = 5; 3.3%), and mixed chromosomal abnormalities (n = 3; 1.2%). In addition, the karyotypes were similar between the ICSI and control groups (p=NS). We observed increases in fetal aneuploidy rates with increased maternal age (<30 years = 23.9% vs. 31–34 years = 37.0% vs. 35–39 years = 82.9% vs. >39 years = 90.9%). However, the observed increases in fetal aneuploidy rates were not statistically significant (p=NS).
Conclusion
The aneuploidy rates and sex chromosome anomalies following ICSI for non-male factor were similar to those following natural conception.

Similar content being viewed by others
References
Simpson JL. Causes of fetal wastage. Clin Obstet Gynecol. 2007;50:10–30.
Wang JX, Norman RJ, Wilcox AJ. Incidence of spontaneous abortion among pregnancies produced by assisted reproductive technology. Hum Reprod. 2004;19:272–7.
Schieve LA, Tatham L, Peterson HB, Toner J, Jeng G. Spontaneous abortion among pregnancies conceived using assisted reproductive technology in the United States. Obstet Gynecol. 2003;101:959–67.
Farr SL, Schieve LA, Jamieson DJ. Pregnancy loss among pregnancies conceived through assisted reproductive technology, United States, 1999–2002. Am J Epidemiol. 2007;165:1380–8.
Simpson JL, Bombard AT. Chromosomal abnormalities in spontaneous abortion: frequency, pathology and genetic counseling. In: Edmonds KBMJ, editor. Spontaneous abortion. London: Blackwell; 1987. p. 51–76.
Angell RR. Aneuploidy in older women. Higher rates of aneuploidy in oocytes from older women. Hum Reprod. 1994;9:1199–2000.
Wright VC, Schieve LA, Reynolds MA, Jeng G. Assisted reproductive technology surveillance—United States, 2002. MMWR Surveill Summ. 2005;54:1–24.
Andersen AN, Gianaroli L, Felberbaum R, de Mouzon J, Nygren KG. Assisted reproductive technology in Europe, 2002: results generated from European registers by ESHRE. Hum Reprod. 2006;21:1680–97.
Baird DT, Collins J, Egozcue J, et al. Fertility and ageing. Hum Reprod Update. 2005;11:261–76.
Woldringh GH, Besselink DE, Tillema AH, Hendriks JC, Kremer JA. Karyotyping, congenital anomalies and follow-up of children after intracytoplasmic sperm injection with non-ejaculated sperm: a systematic review. Hum Reprod Update. 2010;16:12–9.
Squires J, Kaplan P. Developmental outcomes of children born after assisted reproductive technologies. Infants Young Children. 2007;20(1):2–10. Lippincott Williams & Wilkins, Inc.
Wright V, Chang J, Jeng G, Macaluso M. Assisted reproductive technology surveillance—United States, 2003. MMWR Surveill Summ. 2006;55(SS04):1–22.
Wilton L. Preimplantation genetic diagnosis for aneuploidy screening in early human embryos: a review. Prenat Diagn. 2002;22:512–8.
Kushnir VA, Frattarelli JL. Aneuploidy in abortuses following IVF and ICSI. J Assist Reprod Genet. 2009;26:93–7.
Bonduelle M, Van Assche E, Joris H, Keymolen K, Devroey P, Van Steirteghem A, et al. Prenatal testing in ICSI pregnancies: incidence of chromosomal anomalies in 1586 karyotypes and relation to sperm parameters. Hum Reprod. 2002;17:2600–14.
Munne S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64:382–91.
Patrizio P. Intracytoplasmic sperm injection (ICSI): potential genetic concerns. Hum Reprod. 1995;10:2520–3.
de Kretser DM. The potential of intracytoplasmic sperm injection (ICSI) to transmit genetic defects causing male infertility. Reprod Fertil Dev. 1995;7:137–42.
Seamark RF, Robinson JK. Potential health problems stemming from assisted reproduction programmes. Hum Reprod. 1995;10:1321–2.
Simoni G, Brambati B, Danesino C, Rossella F, Terzoli GL, Ferrari M, et al. Efficient direct chromosome analyses and enzyme determinations from chorionic villi samples in the first trimester of pregnancy. Hum Genet. 1983;63:349–57.
Kim JW, Lee WS, Yoon TK, Seok HH, Cho JH, Kim YS, et al. Chromosomal abnormalities in spontaneous abortion after assisted reproductive treatment. BMC Med Genet. 2010;11:153.
Bonduelle M, Camus M, De Vos A, Staessen C, Tournaye H, Van Assche E, et al. Seven years of intracytoplasmic sperm injection and follow-up of 1987 subsequent children. Hum Reprod. 1999;14 Suppl 1:243–64.
Herve C, Moutel G. Sex chromosome abnormalities after intracytoplasmic sperm injection. Lancet. 1995;346:1096–7.
Meschede D, Horst J. Sex chromosomal anomalies in pregnancies conceived through intracytoplasmic sperm injection: a case for genetic counselling. Hum Reprod. 1997;12:1125–7.
Benadiva CA, Kligman I, Munne S. Aneuploidy 16 in human embryos increases significantly with maternal age. Fertil Steril. 1996;66:248–55.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Statement for authors submitting original research: The responsible authors at the institute where the work has been carried out have approved the enclosed manuscript “Comparison of Chromosomal Abnormality Rates in ICSI for Non-Male Factor and Spontaneous Conception”. Authors certify that none of the materials in this manuscript has been published previously in any form and that none of this material is currently under consideration for publication elsewhere. All authors have participated sufficiently in the intellectual content, the analysis of data and the writing the manuscript to take public responsibility for it.
Capsule
The chromosomal anomalies and aneuploidy rates following ICSI for non-male factor were similar to those following natural conception.
Rights and permissions
About this article
Cite this article
Bingol, B., Abike, F., Gedikbasi, A. et al. Comparison of chromosomal abnormality rates in ICSI for non-male factor and spontaneous conception. J Assist Reprod Genet 29, 25–30 (2012). https://doi.org/10.1007/s10815-011-9646-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-011-9646-1