Abstract
Purpose
To compare pre-cryo data from oocyte cryopreservation (OC) cycles performed for malignancy (MED) vs. elective deferment of reproduction (DR) or oocyte donation (OD).
Methods
All patients were ≤40 y and underwent standard ovarian stimulation and retrieval. Prior to OC, meiotic spindle (MS) and zona pellucida (ZP) retardance was measured using digital polarized light microscopy (DPLM).
Results
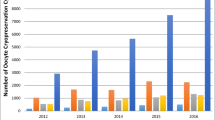
Of 130 OC cycles, 49 were for MED, 73 for DR, and 8 for OD. Cycles completed for MED had an average of 9 ± 1 spindle-positive oocytes with a mean MS retardance of 1.2 ± .02 nm and ZP retardance of 2.1 ± .06 nm, which was clinically comparable to the other groups.
Conclusions
Women with malignancy can achieve adequate ovarian response and similar oocyte parameters to those of women undergoing fertility preservation for non-cancer indications. Such information, coupled with the ability to noninvasively study oocyte dynamics, may improve the counseling of cancer patients seeking fertility preservation.

Similar content being viewed by others
References
Bleyer A, Viny A, Barr R. Cancer in 15- to 29-year-olds by primary site. Oncologist. 2006;11:590–601.
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–31.
El Shafie M, Sousa M, Kruger T. An Atlas of the ultrastructure of human oocytes. A guide for assisted reproduction. New York: Parthenon; 2000.
Wang WH, Meng L, Hackett RJ, Keefe DL. Developmental ability of human oocytes with or without birefringent spindles imaged by Polscope before insemination. Hum Reprod. 2001;16:1464–8.
Oldenbourg R. Polarized light microscopy of spindles. Methods Cell Biol. 1999;61:175–208.
De Santis L, Cino I, Rabellotti E, Calzi F, Persico P, Borini A, et al. Polar body morphology and spindle imaging as predictors of oocyte quality. Reprod Biomed Online. 2005;11:36–42.
Rama Raju GA, Prakash GJ, Krishna KM, Madan K. Meiotic spindle and zona pellucida characteristics as predictors of embryonic development: a preliminary study using PolScope imaging. Reprod Biomed Online. 2007;14:166–74.
Grifo JA, Noyes N. Delivery rate using cryopreserved oocytes is comparable to conventional in vitro fertilization using fresh oocytes: potential fertility preservation for female cancer patients. Fertil Steril. 2010;93:391–6.
Noyes N, Knopman J, Labella P, McCaffrey C, Clark-Williams M, Grifo J. Oocyte cryopreservation outcomes including pre-cryopreservation and post-thaw meiotic spindle evaluation following slow cooling and vitrification of human oocytes. Fertil Steril. 2010. doi:10.1016/j.fertnstert.2010.01.019. Epub ahead of print.
Cobo A, Kuwayama M, Perez S, Ruiz A, Pellicer A, Remohi J. Comparison of concomitant outcome achieved with fresh and cryopreserved donor oocytes vitrified by the CryoTop method. Fertil Steril. 2008;89:1657–64.
Nagy ZP, Chang CC, Shapiro DB, Bernal DP, Elsner CW, Mitchell-Leef D, et al. Clinical evaluation of the efficiency of an oocyte donation program using egg cryo-banking. Fertil Steril. 2009;92:520–6.
Shen Y, Betzendahl I, Tinneberg HR, Eichenlaub-Ritter U. Enhanced polarizing microscopy as a new tool in aneuploidy research in oocytes. Mutat Res. 2008;651:131–40.
Wang WH, Keefe DL. Prediction of chromosome misalignment among in vitro matured human oocytes by spindle imaging with the PolScope. Fertil Steril. 2001;78:1077–81.
Cohen Y, Malcov M, Schwartz T, Mey-Raz N, Carmon A, Cohen T, et al. Spindle imaging: a new marker for optimal timing of ICSI? Hum Reprod. 2004;19:649–54.
Shen Y, Stalf T, Mehnert C, De Santis L, Cino I, Tinneberg HR, et al. Light retardance by human oocyte spindle is positively related to pronuclear score after ICSI. Reprod Biomed Online. 2006;12:737–51.
Liu L, Trimarchi JR, Oldenbourg R, Keefe DL. Increased birefringence in the meiotic spindle provides a new marker for the onset of activation in living oocytes. Biol Reprod. 2000;63:251–8.
Shen Y, Stalf T, Mehnert C, Eichenlaub-Ritter U, Tinneberg HR. High magnitude of light retardation by the zona pellucida is associated with conception cycles. Hum Reprod. 2005;20:1596–606.
Hyun CS, Cha JH, Son WY, Yoon SH, Kim KA, Lim JH. Optimal ICSI timing after the first polar body extrusion in in vitro matured human oocytes. Hum Reprod. 2007;22:1991–5.
Keefe D, Liu L, Wang W, Silva C. Imaging meiotic spindles by polarization light microscopy: principles and applications to IVF. Reprod Biomed Online. 2003;7:24–9.
Montag M. Spindle imaging in human oocytes: the impact of the meiotic cell cycle. Reprod Biomed Online. 2006;12:442–6.
Acknowledgements
The authors would like to thank the entire NYU Fertility Center staff for their involvement in the oocyte cryopreservation program at New York University and especially, the embryology team for their expertise in oocyte assessment and cryopreservation.
Financial support
None
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Oocytes from cancer patients seeking fertility preservation are similar to those of healthy women both in quantity and characteristics as viewed by polarized light microscopy.
Rights and permissions
About this article
Cite this article
Werner, M., Reh, A., Labella, P.A. et al. Laboratory evaluation in oocyte cryopreservation suggests retrieved oocytes are comparable whether frozen for medical indications, deferred reproduction or oocyte donation. J Assist Reprod Genet 27, 613–617 (2010). https://doi.org/10.1007/s10815-010-9455-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-010-9455-y